Is there a place for using mitoxantrone to treat MS?
I suggested mitoxantrone as he was in his late twenties and had not yet started a family.
I was recently asked my opinion on a case with very active MS from North Africa. The patient was a refugee from a neighbouring country. He had recently been diagnosed with MS and had spinal cord and brainstem attacks. His latest MRI showed a very high lesion load with over 20 Gd-enhancing lesions on MRI, including active lesions in the brainstem, cerebellum and spinal cord. The spinal fluid analysis had shown a slightly raised protein and some lymphocytes, which his active spinal cord disease could explain.
As this patient could not afford high-cost licensed therapies, such as natalizumab, his consultant neurologist wanted to treat him with the off-label chemotherapy agent cyclophosphamide. However, I suggested mitoxantrone as he was in his late twenties and had not yet started a family. Cyclophosphamide is toxic to the testes, whereas mitoxantrone does not cross the blood-testes barrier; hence sperm banking is unnecessary. Another factor favouring using mitoxantrone is that it is licensed to treat MS in several countries, whereas cyclophosphamide is not a licensed DMT.
Before starting mitoxantrone, I urge this patient to address the following questions and understand them before making an informed decision about starting treatment. This newsletter covers the issues about mitoxantrone. Please be aware that we rarely use mitoxantrone to treat MS on the NHS anymore. The reason is we have alternative options that are as effective and safer. However, in resource-poor settings such as treating uninsured refugees, mitoxantrone is still a very useful DMT.
What is the risk of not being treated with a disease-modifying therapy (DMT)?
What are the attributes of the specific DMTs or treatment strategies?
Mitoxantrone
S1P modulators
Alemtuzumab
Cladribine
Teriflunomide
Fumarates
Anti-CD20
AHSCT
How can I derisk or reduce my chances of getting certain adverse events on specific DMTs?
Will I be able to become a parent? What about pregnancy and breastfeeding?
Mitoxantrone
Summary
Mitoxantrone (Novantrone) is licensed to treat MS in several countries. It is typically used to treat active secondary progressive, progressive relapsing, or worsening relapsing-remitting MS. It is a repurposed chemotherapy agent and is given as an intravenous infusion. It is either given as a monthly infusion for six months, every three months for up to 2 years, or a combination of these two protocols. Mitoxantrone is associated with potentially severe toxicity (infections, cardiotoxicity, premature ovarian failure and secondary leukaemia), which is why it is not used that often anymore. In some countries, it is used as true induction therapy followed by a maintenance DMT, typically interferon-beta or glatiramer acetate. Because it is toxic to the heart, a limited cumulative dose can be given safely over a lifetime. Mitoxantrone is on my list of essential DMTs because it is generic and is available for treating MS in resource-poor settings.
Trade Names: Novantrone, Mitozantrone, Onkotrone
Mode of action: Mitoxantrone is an immune constitution therapy. It works by inhibiting the enzyme topoisomerase II, which unwinds DNA. As a result of its actions on this enzyme, it disrupts DNA synthesis and repair in cells and causes them to die. White blood cells are particularly sensitive to its actions. Mitoxantrone is derived from a group of chemicals called anthracenediones that are toxic to the heart in high doses.
Efficacy: High to very high
Class: Non-selective IRT, short-term immunosuppression
Immunosuppression: Yes
Infusion protocols:
Edan Protocol: Mitoxantrone 20mg by intravenous infusion (ivi) monthly in combination with 1g methylprednisolone x 6 months (6 doses)
Hartung Protocol: Mitoxantrone 12mg/m2 ivi 3 monthly x 2 years (8 doses)
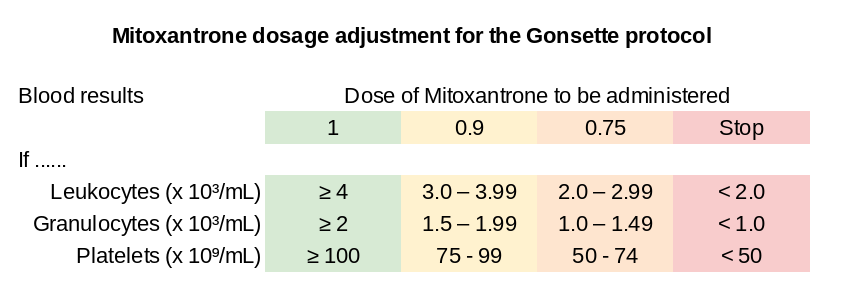
Gonsette Protocol: Mitoxantrone 12mg/m2 ivi monthly x 3 months followed by Mitoxantrone 12mg/m2 ivi 3 monthly up to 2 years (10 doses). Please note the Gonsette protocol includes an algorithm to adjust the next dose depending on the recovery of the peripheral blood cell counts.
Additional courses of mitoxantrone can be given beyond what is stated in these protocols, provided the total lifetime dose of mitoxantrone does not exceed 140 mg/m² and that cardiac monitoring (ECG and ejection fraction) does not show signs of cardiomyopathy (cardiac toxicity).
Adverse events and events of special interest
Infection: Mitoxantrone causes a low white cell count and may increase susceptibility to infection. Therefore it is important that all infections are identified early and treated. The presence of an active infection may delay the next infusion. Chest infections and urinary tract infections are common after mitoxantrone. Maintaining skin integrity is also important, as broken skin or ingrown toenails may become areas harbouring infection. People with MS (pwMS) and their families and/or carers should be educated about assessing and detecting infection so that potential problems are recognised early.
Please note that pwMS treated with mitoxantrone may become neutropenic and susceptible to neutropenic sepsis, including infection with Listeria monocytogenes.
Nausea and vomiting: Nausea may occur during treatment and the next day. Antiemetic drugs are usually prescribed to help manage this. The doses of mitoxantrone used to treat MS are much lower than those used in cancer patients. Therefore, this side effect tends to be milder.
Hair loss: Hair may become temporally thinner during mitoxantrone treatment but will return to normal once the treatment is finished. Hair loss is uncommon and happens in less than 3% of pwMS who receive mitoxantrone. If it does occur, it usually begins 3-4 weeks after the first dose has been administered.
Cardiotoxicity: As high doses of mitoxantrone have been associated with cardiotoxicity, it is necessary to have a baseline heart scan before commencing the first dose of treatment. This scan can either be a MUGA scan or an echocardiogram. These are routine tests that measure the contractility of the heart. The MUGA scan requires the injection of a very low dose of a radionuclide tracer, which is then detected using a machine similar to an x-ray machine. An echocardiogram is a form of ultrasound using a probe applied to the chest. Neither of these tests is painful. The MUGA scan or echocardiogram should be completed at baseline and then 3-monthly before administering the next dose of mitoxantrone. Mitoxantrone treatment may have to be stopped if the tests show a significant decrease in cardiac function, i.e. a decrease in ejection fraction below 50%. These problems generally happen in people with a total lifetime dose of more than 140 mg/m².
Extravasation: Mitoxantrone is an irritant which can produce pain and inflammation along the path of a vein through which it is administered. Extravasation occurs when the drug accidentally infiltrates the tissue outside the vein. To avoid extravasation, the cannula must be sited in the non-dominant arm and away from areas of joint flexion. The site should not be obscured and should be checked at regular intervals. An extravasation kit should be available at the bedside in case of emergency.
Therapy-related leukaemia: Secondary acute myelogenous leukaemia (AML) has been reported in pwMS and cancer patients treated with mitoxantrone. Typically therapy-related leukaemia, with topoisomerase II inhibitors such as mitoxantrone, develops within 2-4 years after chemotherapy has been started. Based on the current data, the risk of leukaemia in subjects with MS treated with mitoxantrone is ~1 in 200-400.
Infertility: Amenorrhea (lack of periods) may occur during treatment and should be investigated as it may respond to treatment with hormonal replacement therapy. A less common complication is the induction of menopause which should be fully investigated should it occur. Transient amenorrhea occurs in ~12% of patients, and persistent amenorrhea, or premature menopause, in ~10% of patients. The risk of persistent amenorrhoea is higher in women older than 35 (14%) and lower in women less than 35 years of age (6.5%). If indicated, women should either be offered GnRH agonists as ovarian protection during the course of therapy or the possible option of egg harvesting and storage.
Pharmacovigilance monitoring requirements and derisking strategies
Baseline: FBC, U&E, LFTs, TFTs, serum protein electrophoresis, serum immunoglobulin levels, serology (VZV, HIV-1&2, hepatitis B&C, syphilis), TB elispot, an up-to-date cervical smear and/or HPV testing, vaccine review, pregnancy test, ECG and cardiac ejection fraction (echocardiography or MUGA scan).
Follow-up:
1 to 3 monthly (predosing) FBC, U&E and LFTs and, in women, a pregnancy test.
Three monthly ECG and cardiac ejection fraction (echocardiography or MUGA scan)
12 monthly TFTs
Endocrine work-up for women pwMS' with persistent amenorrhea
Infection prophylaxis:
If found to be VZV seronegative, you will need to receive the VZV vaccine at least 6 weeks before being treated with mitoxantrone to allow sufficient time to develop immunity and protective antibodies against the virus.
If you have a history of recurrent urinary tract infections, you should be taught to self-monitor for urinary tract infections using home dipstix monitoring of your urine, provided with urine specimen bottles for laboratory testing and possibly an unfilled prescription for a standard first-line antibiotic. The plan is that if you do develop a UTI and self-diagnose it, you can collect and drop off your urine for microscopy, culture and antibiotic sensitivity testing (MCS) at your GP or the laboratory. You can then collect your prescription and start your antibiotics. Once the culture and antibiotic sensitivities come back, your doctor may change the antibiotics. Please note not all GPs support UTI self-monitoring and self-management of your MS.
As you are at risk of developing Listeriosis after mitoxantrone, you should be advised about starting a Listeriosis diet and how to institute a behavioural programme to reduce your chances of exposure to Listeriosis. You may also be offered antibiotic prophylaxis to reduce your chances of developing Listeriosis. Please see the ABN Listeria prophylaxis guideline and the ClinicSpeak web application on this topic.
Rebaselining: A rebaseline MRI needs to be done after completing the course of mitoxantrone. Depending on which protocol you have been treated with, this could be 6 or 24 months.
Pregnancy: Pregnancy is contraindicated during the course of mitoxantrone as it may harm the developing foetus. While taking mitoxantrone, women who might become pregnant should use effective birth control and be sure, before each dose, that they are not pregnant. If unsure, a pregnancy test should be performed.
Breastfeeding: Mitoxantrone is excreted in human milk, and significant concentrations (18 ng/ml) have been reported for 28 days after the last administration. Because of the potential for serious adverse reactions in infants from mitoxantrone, breastfeeding should be discontinued before starting treatment.
Male Fertility: Although mitoxantrone causes transient oligospermia, male infertility has not been a problem. In contrast to other chemotherapy agents, e.g. alkylating agents (cyclophosphamide), after cessation of mitoxantrone therapy, there is complete recovery of sperm production without morphological changes in vitro or genotoxic effects on germinal cells in vivo. Given this offering to male patients, the option of routine sperm banking is unnecessary.
Vaccination: Immunisation may be ineffective when given during mitoxantrone therapy. Immunisation with live virus vaccines is generally not recommended, until after the immune system has reconstituted, which is several months after the last course of mitoxantrone.
Summary of Product Characteristics (SmPC): mitoxantrone (generic)
Switching to Mitoxantrone
Lack of efficacy (repeat course of mitoxantrone): As mitoxantrone is an Immune Reconstitution Therapy (IRT), breakthrough activity may trigger the need for additional courses to be given, provided the total lifetime dose of mitoxantrone does not exceed 140 mg/m² and that cardiac monitoring (ECG and echo/MUGA) do not show signs of underlying cardiomyopathy.
Other DMTs: Provided the baseline screening tests are done and are fine, there are no specific contraindications. I see no reason why mitoxantrone can't be used after any of the licensed DMTs.
Interferon-beta and glatiramer acetate: There are no specific cautions.
S1P modulators (Fingolimod, Siponimod, Ozanimod, Ponesimod): The development of mitoxantrone-related cardiomyopathy and/or cardiac arrhythmia is a contraindication for using S1P modulators after mitoxantrone. It is important to be extra-vigilant when doing the routine baseline cardiac checks post-mitoxantrone. If it has been some time since the last dose of mitoxantrone, I recommend having a cardiac ejection fraction checked with echocardiography or a MUGA scan.
Non-selective cell depleting DMTs (alemtuzumab & HSCT): a persistently low peripheral white cell count post alemtuzumab or HSCT, i.e. a neutrophil count < 1000/mm³ or a total lymphocyte count <800/mm³ is a relative contraindication to using mitoxantrone. Another hit on the bone marrow and the primary and secondary lymphoid organs may worsen their leukopaenia and render them more immunosuppressed. The decision to use mitoxantrone in this situation has to be based on the potential benefits versus the risks of these treatments and the risks of untreated active MS.
Selective cell depleting DMTs (cladribine): a persistently low peripheral lymphocyte cell count post cladribine, i.e. a total lymphocyte count <800/mm³, is a relative contraindication to using mitoxantrone. The effect of mitoxantrone on primary and secondary lymphoid organs may worsen the lymphopaenia and is a risk factor for developing grade 3 or grade 4 lymphopaenia, i.e. <500/mm³ or <200/mm³, respectively. However, the decision to use mitoxantrone in this situation has to be based on the potential benefits of the treatment versus the risks of lymphopaenia and the risks of untreated active MS.
Selective cell depleting DMTs (anti-CD20 therapies, i.e. ocrelizumab, ofatumumab and rituximab): as anti-CD20 therapies are selective B-cell depleting agents, the use of mitoxantrone after an anti-CD20 therapy is theoretically much safer than the other less selective and non-selective agents.
Natalizumab: As mitoxantrone is an IRT that can't be rapidly reversed, it is critical to ensure no asymptomatic PML. Carry-over PML from natalizumab to mitoxantrone is potentially fatal. Therefore, a baseline MRI scan and possibly a CSF examination are essential to exclude the possibility of PML.
Furmarates (dimethyl fumarate, diroximel fumarate): Fumarates reduce the lymphocyte count by approximately 30% and, in some pwMS, more than this. Therefore, pwMS who have lymphopaenia on DMF may be more susceptible to developing clinically significant prolonged lymphopaenia post-mitoxantrone.
Teriflunomide: Because teriflunomide is an antiproliferative agent, it may delay or prevent the recovery of the peripheral white cell count post-mitoxantrone. One option is to do an accelerated teriflunomide washout to prevent this potential problem. Interestingly, rheumatologists who use leflunomide, a prodrug converted to teriflunomide, don't use an accelerated washout when using antiproliferative agents post-leflunomide.
Special circumstances: The presence of other specific comorbidities and adverse events may make it difficult to start mitoxantrone after other DMTs.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription, please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.




I was on Mitoxantrone about 15 or so years ago due to very active MS and was also in my late twenties. After, as maintenance, was put on Copaxone, then Avonex (due to issues with injection sites). Am now on DMF. I have to say, although risky, Mitox immediately brought my relapses under control and have been pretty stable since but it was definitely a hard drug to be on - unfortunately, it was my only choice at the time (was waiting for Natalizumab to be licensed) and felt my MS was just too active to wait as my relapses were disabling me! So, in answer to the question, yes I do think there is a place for using Mitoxantrone where there isn't another option, such as in resource poor settings. It is important to weigh up however against these types of treatments the risks and benefits of doing so and remember that MS, when out of control, can also affect someone's life.