Natalizumab
A detailed look at natalizumab and some of the complexities of its use in clinical practice.
Apologies for the delay in getting information onto MS-Selfie about each DMT. I only have so many hours in a day, and I am aware you don’t want too many Newsletters.
The following are the questions a person with MS needs to ask, themselves or their HCP, and understand before they can make an informed decision about starting a DMT (disease-modifying therapy). This newsletter covers natalizumab.
What is the risk of not being treated with a disease-modifying therapy (DMT)?
What are the attributes of the specific DMTs or treatment strategies?
Mitoxantrone
Natalizumab
S1P modulators
Alemtuzumab
Teriflunomide
Fumarates
Anti-CD20
AHSCT
How can I derisk or reduce my chances of getting certain adverse events on specific DMTs?
Will I be able to become a parent? What about pregnancy and breastfeeding?
Natalizumab Summary
Natalizumab is a first-in-class selective adhesion molecule blocker and works by reducing the trafficking of lymphocytes (white blood cells that are thought by some to cause MS) into the central nervous system. Natalizumab is a very high-efficacy DMT capable of achieving long-term NEIDA (no evident inflammatory activity) in most people with MS (pwMS) treated with natalizumab. Natalizumab also goes beyond NEIDA and has a large impact on end-organ damage (slowining down or preventing disabilit accrual and reducing the rates of brain volume loss). Once rebaselined, average annual brain volume loss is close to the range one would see in normal-aged people without MS.
One result of reduced trafficking of lymphocytes in the brain is reduced immune surveillance, which puts pwMS on natalizumab at high risk of an infection of the brain called progressive multifocal leukoencephalopathy (PML). PML only occurs in people infected with the JC virus that causes PML. The risk of PML is variable and can be reduced by using extended interval dosing (EID), i.e. extending the dosing from 4-weekly to 6-weekly or longer. Natalizumab is given as a 4-weekly infusion or by subcutaneous injection. Generally both routes of administration are very well tolerated. A small number of pwMS (<5%) develop infusion reactions, which can be serious. Infusion reactions typically come on with the 2nd, 3rd or 4th infusion and are associated with developing so-called antidrug antibodies (ADAs).
Natalizumab has a rapid onset of action and is the fasting-acting DMT available to treat MS. When used early a large number of pwMS notice an improvement in disability and often report improvement in fatigue and other symptoms such as brain fog, which is why pwMS like natalizumab so much.
Trade Name
Tysabri
Mode of action
Natalizumab is immunosuppressive as it is associated with opportunistic infections and possibly secondary malignancies of the central nervous system. Natalizumab is a monoclonal antibody that targets VLA-4 or α4β1 integrin on lymphocytes, preventing them from crossing the blood-brain barrier. A good analogy of how the lymphocytes cross the blood-brain barrier is velcro. Lymphocyte have to first stick to the wall of the blood vessel before they can cross it. Natalizumab blocks one of the surfaces (or velcro), so the lymphocytes cannot cross the wall of the blood vessel. The following video explains Natalizumab's mode of action. PwMS on natalizumab treatment have an increased number of circulating white blood cells in their blood; the reason this occurs is that pool of cells that tend to be stuck or rolling on blood vessel walls (marginating cells) are now found in the blood.
Efficacy
Very high, particularly in pwMS with rapidly evolving severe MS.
Class
Maintenance, immunosuppressive.
Immunosuppression
Yes, but mainly limited to the CNS.
Posology
Natalizumab 300 mg is administered by intravenous infusion once every 4-6 weeks, or it can be administered as two subcutaneous injections containing 150mg each; the injection volume is 2 x 1ml.
Main adverse events
Adverse events of special interest:
Infusion reactions: These tend to be mild and occur in ~20% of pwMS and may be associated with headache, dizziness, nausea, urticaria and rigours.
Hypersensitivity reactions: these occur in approximately 5% of pwMS. In about a quarter of these, they can be anaphylactoid and typically occur during the infusion or within an hour of completing the infusion, which is why you are asked to stay behind for an hour after the infusion is completed. Hypersensitivity reactions are associated with either low or high blood pressure, chest pain, chest discomfort, shortness of breath, swelling of the throat, rash, urticaria, rigours, nausea, vomiting and flushing. Most hypersensitivity reactions occur on the 2nd, 3rd or 4th infusion and are associated with the development of anti-drug antibodies, i.e. your own body rejects the drug by making antibodies against natalizumab. Persistent anti-natalizumab antibodies develop in approximately 5-6% of pwMS on natalizumab and decrease the effectiveness of natalizumab and cause hypersensitivity reactions.
Infections: In general, natalizumab is not associated with systemic infections. As an immunosuppressive therapy, natalizumab has been associated with opportunistic infections, particularly progressive multifocal leukoencephalopathy (PML). Other opportunistic infections include cryptosporidium diarrhoea and cryptococcal meningitis. Herpes infections (Varicella-Zoster virus, Herpes-simplex virus) occur more frequently on natalizumab. Serious life-threatening encephalitis and meningitis caused by herpes simplex or varicella-zoster can occur on natalizumab. The presentation of these infections is atypical in that natalizumab reduces the trafficking of cells into the CNS, and hence the associated inflammation due to these infections is less intense. So the presentations tend to be more indolent and subacute and tend to evolve over weeks rather than hours to days. Rarely these viruses may infect the retina, which is part of the CNS and can lead to acute retinal necrosis and loss of vision.
PML and granule cell neuronopathy: JCV is the commonest opportunistic infection in seropositive natalizumab-treated pwMS (see section below). JCV causes PML and granule cell neuronopathy (GCN). PML is more common than GCN, and its management is described below. GCN is characterised by lytic infection of the cerebellar granule cell layer and presents with cerebellar ataxia and cerebellar atrophy, and white matter changes in the cerebellum and brainstem on MRI. Many cases of GCN also have white matter changes elsewhere, suggesting an overlap between GCN and PML.
Abnormal liver function tests: Autoimmune hepatitis, increased liver enzymes and hyperbilirubinaemia can rarely occur on natalizumab.
Anaemia: Anaemia and haemolytic anaemia have been rarely reported in natalizumab-treated pwMS.
Malignancies: Several cases of CNS lymphoma have been reported in pwMS treated with natalizumab. The risk of CNS lymphoma is likely to be increased based on the mode of action of natalizumab, i.e. it blocks immune surveillance of the CNS; hence there will be an increased risk of CNS tumours.
Ant-drug (ADAs) and neutralising antibodies (NAbs):
Yes, in approximately 5% of natalizumab-treated pwMS ADAs persistent neutralizng are found at month 12. If these are found the drug needs to be stopped. One in four people with ADAs or NABs will not get infusion reactions, therefore, it is good practice to screen for them at month 12 after starting treatment.
Pharmacovigilance monitoring requirements:
Baseline: FBC, U&E, LFTs, JCV-serology and pregnancy test.
Follow-up: LFTs 3 monthly for the first year, NABs at 12 months and JCV serology every six months. In pwMS, at high risk of PML, 3-4-monthly MRI scans are recommended for PML surveillance, otherwise annual MRI monitoring for disease activity monitoring.
Self-monitoring: All pwMS should be warned about opportunistic infections and informed to be vigilant for symptoms suggestive of infections. Women should be reminded to self-examine their breasts monthly and have cervical smears and/or HPV testing done every three years as part of the national surveillance programme.
Rebaselining
A rebaseline MRI needs to be done after natalizumab has had sufficient time to work. As natalizumab works very quickly, I would recommend it done enzymes 3-6 months after starting treatment and to include Gd-enhancement as part of the rebaselining MRI.
Pregnancy
Animal studies have shown no toxicity from natalizumab, and data from clinical trials and post-marketing studies suggest natalizumab exposure has no adverse effect on pregnancy outcomes. There may be an increased risk of spontaneous abortions on natalizumab; however, there is not enough data on this to be sure. Babies born to pwMS on natalizumab have a transient mild to moderate low platelet count and anaemia, which disappear within weeks of delivery. Many neurologists are now allowing their female patients to fall pregnant whilst on natalizumab and then offer to stop it after they have become pregnant, typically towards the end of the second trimester, when the placenta matures and allows maternal antibodies, including natalizumab, to transfer to the unborn child. Because of the emerging safety profile of natalizumab in pregnancy, some neurologists are letting patients continue natalizumab throughout pregnancy. The decision to do this is based on the risk of rebound MS activity when natalizumab washes out.
Breastfeeding
The amount of natalizumab that crosses over into the breast milk is very small and likely to be digested by the baby's digestive enzymes; therefore, it is safe to breastfeed on natalizumab.
Male Fertility
Safe
Vaccination
Safe for component or inactivated vaccines. Live vaccines are contraindicated. The administration of live viruses, particularly ones that can infect the central nervous system, is potentially dangerous, which is why it is advisable to have live vaccines such as yellow fever and, if required, MMR before starting natalizumab (for more information on vaccines see ‘The rationale for derisking DMTs’ (20-Aug-2022) newsletter.
Summary of Product Characteristics (SmPC)
Switching onto natalizumab
Natalizumab: Recent data has shown that reducing the dosing interval between natalizumab infusions (extended interval dosing or EID) will lower the risk of someone developing PML without affecting the efficacy of natalizumab as assessed on MRI (see EID below).
Restarting Natalizumab: Before restarting natalizumab, it is important to do routine blood tests, a baseline MRI and check for anti-natalizumab antibodies. PwMS who stop natalizumab may develop anti-natalizumab antibodies that put them at risk of developing infusion reactions. The presence of these antibodies is a contraindication to restarting natalizumab. It is not uncommon for pwMS to request being switched back to natalizumab after switching to another DMT. Natalizumab is known to reduce MS-related fatigue and cog fog; this often returns when natalizumab is stopped, and its effects are reversed. The ability to reduce PML risk with EID has increased the number of pwMS requesting to go back onto natalizumab to help manage these symptoms.
Other DMTs: In general, there are no DMTs after which natalizumab cannot be used, provided the baseline screening blood tests are normal. Specific caveats are highlighted below.
Interferon-beta and glatiramer acetate: I have no concerns and would not recommend any specific washout period between stopping either IFN-beta or GA and starting natalizumab.
Non-selective cell-depleting DMTs (alemtuzumab, mitoxantrone & HSCT): I assume you would want to start natalizumab after alemtuzumab or HSCT because of recurrent disease activity. If this is the case, I recommend starting natalizumab as soon as possible. Please note as alemtuzumab and HSCT are immunosuppressive therapies, they render the so-called anti-JCV index unreliable; therefore, you can’t use it to determine your PML risk (see below).
Selective cell-depleting DMTs (cladribine, anti-CD20 [ocrelizumab, ofatumumab, rituximab]): Again the assumption you would want to start natalizumab after cladribine or anti-CD20 because of recurrent disease activity. If this is the case, I recommend starting natalizumab as soon as possible. Please note as cladribine and anti-CD20 therapies are immunosuppressive therapies thet render the anti-JCV index unreliable.
S1P Modulators (Fingolimod, Siponimod, Ozanimod, Ponesimod): No washout period is required when switching to natalizumab. However, if someone has an infectious complication, particularly a CNS infection, it would be ill-advised to start natalizumab until the CNS infection has been cleared. For example, if someone has a fungal meningitis as a complication of fingolimod, you would want to be confident that it has been cleared before starting natalizumab as natalizumab reduces lymphocyte trafficking into the CNS and hence will blunt the immune response to the infectious agent.
Fumarates (dimethyl fumarate, diroximel fumarate): No washout period is required when switching from one of the fumarates to natalizumab. The same warning about CNS infections applies to fumarates mentioned above in relation to the S1P modulators.
Teriflunomide: No teriflunomide washout period is required when switching to natalizumab. However, if the switch to natalizumab is to allows MS disease control so that an pwMS can fall pregnant, the patients will need to undergo rapid teriflunomide elimination because of its long half-life and potential for teratogenicity.
Special circumstances: The presence of specific comorbidities and adverse events may make it difficult to start natalizumab after certain DMTs. These are, however, uncommon in routine clinical practice.
Extended interval dosing
I have several patients who, despite being JC virus (JCV) seropositive, insist on staying on natalizumab when alternative treatment options are available. I even have a few patients who, after switching to another DMT to prevent getting PML, have opted to go back onto natalizumab. The reason for the latter decision typically relates to the return of MS fatigue, or brain fog, after switching from natalizumab to another DMT. Natalizumab is remarkable in this regard and is the only DMT in which an n=1 trial is sufficient to know that the therapy works. Patients often come back after a few months of treatment and say, ‘I feel well, my fatigue has gone, and I am thinking clearly’. This is why anything that decreases the risk of PML for patients on natalizumab has to be a good thing.
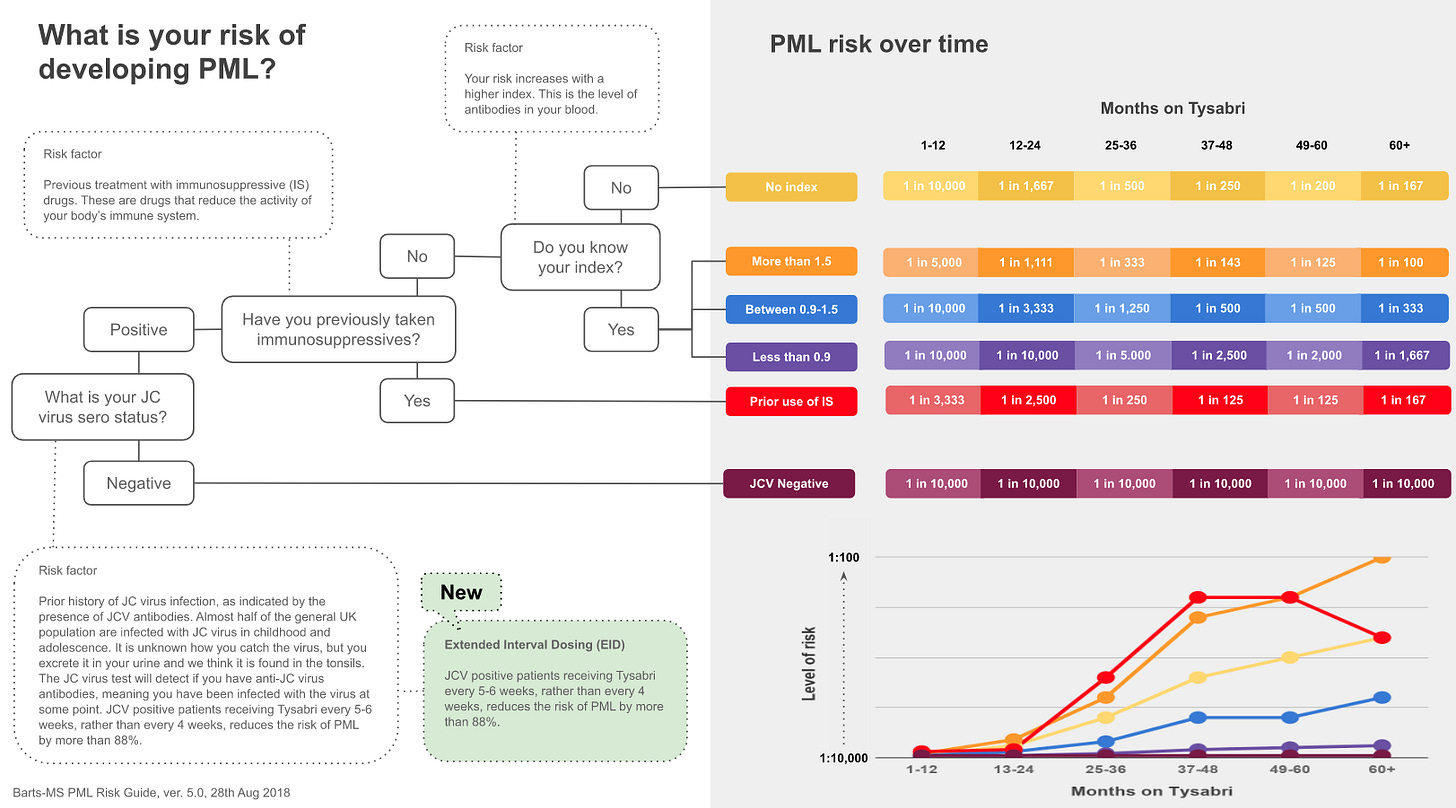
At present, we have JC virus testing (negative and positive), level of JCV antibodies (antibody index), a rising antibody index, previous exposure to immunosuppression, and treatment duration to help guide us concerning the PML risk assessment. We also have frequent MRI monitoring (3-4 monthly) to detect PML early and potentially plasma exchange to remove natalizumab as a backup option if you develop PML. Extended interval dosing (EID) is now another option at hand to reduce the risk of PML.
The theory behind EID is that some cells are less sensitive to the effects of natalizumab and that if you delay the next natalizumab infusion by 1 or 2 weeks, the saturation of their surface receptors drops below a threshold and allows these cells to traffic into the central nervous system. If these less natalizumab-sensitive cells are the antiviral CD8+ T-cells and/or the natural-killer cells that fight viruses, this could allow immune surveillance of the CNS and prevent PML. If you get the EID right, the saturation of the immune cells causing MS, possibly the memory B cells, is sufficient not to allow MS to reactivate. Not all cells are made equal regarding the effect of natalizumab. Importantly, there are several other adhesion molecules on cells that impact on adhesion (stickiness) of immune cells to the blood vessels in the CNS. It could also be a delicate balance between the availability of different accessory adhesion molecules that makes the difference.
These principles were originally adopted by several neurologists in the USA and the data that has emerged from their centres suggests they are correct, i.e. despite being JCV+ve pwMS on natalizumab EID have a much lower risk of developing PML.
When Biogen, who markets natalizumab, saw these EID results, they decided to interrogate their database on the use of natalizumab in the USA. They are fortunate to have the so-called TOUCH programme, a mandatory database of all pwMS on natalizumab in the USA. The TOUCH database allowed the statisticians to find people on EID and compare them to standard interval dosing (SID) for PML risk. Because the TOUCH programme is real-life data and is not a clinical trial database, the periods of EID are variable. To deal with this, the statisticians defined three types of EID with increasing stringency. The remarkable finding is that EID was found to reduce the risk of PML compared to SID, and in the most stringently defined cohort of EID, there were no cases of PML.
What is the impact of EID on the efficacy of natalizumab? In a recently completed study, there was no difference between EID and standard 4-weekly dosing in MRI and clinical relapse activity. These results are reassuring and indicate that if you do switch to 6-weekly infusions, you are not going to compromise on efficacy.
PML
What is PML?
PML stands for progressive multifocal leukoencephalopathy and is a relatively rare but potentially fatal disease of the brain caused by a viral infection. PML is characterised by progressive damage of the white matter of the brain, typically in multiple different areas hence the descriptor multifocal.
PML is caused by the JC virus (JCV), which causes a persistent infection normally kept under control by your immune system. JC refers to John Cunningham the name of the index patient in whom PML was first described; please note the tradition of naming viruses after patients has stopped. In general, the JC virus is harmless and only causes problems in people who are immunocompromised or have weakened immune systems.
You can get infected with the JC virus at any time. Infections start in childhood and increase gradually so that by the time you are an adult approximately 50-60% of the general population are infected with the virus. We estimated that about 0.5% of the population gets infected with the virus every year, i.e. seroconvert. The JV virus is transmitted in urine and saliva. JCV cause an asymptomatic primary, or initial, infection; in other words, you don't have any know ill effects when you become infected with JCV. JCV resides in the kidney, possibly the bone marrow and lymphoid tissue. Infected people intermittently shed the virus in their urine and saliva, which is why we think these two body fluids are responsible for spreading the infection.
When you are infected with the virus, your immune system responds to it by making antibodies, i.e. you become JCV seropositive. We detect these antibodies with a simple blood test. We assume that all people who are JCV-seropositive are still infected with the virus.
How does JCV cause PML?
If you are immunocompetent, your immune system keeps the virus in check. If your immune system is compromised, JCV is allowed to replicate, and as it replicates, it mutates. Some of the mutants acquire the ability to infect glial cells in the brain, i.e. the oligodendrocyte that produces myelin and the astrocyte. Once the mutant JCV infects the glial cells, it hijacks the cells' machinery and reproduces itself. This causes the cell to burst or lyse, releasing thousands of new viruses to infect adjacent cells. After a critical amount of glial cells are infected and killed, you develop focal neurological symptoms. The symptoms you present with PML depend on the areas of the brain that is infected with the virus. The symptoms of PML are very non-specific and can mimic an MS relapse. The latter is a problem as many pwMS have been misdiagnosed as having a relapse when they initially present with their first symptoms of PML. However, if the presenting symptoms are a change in cognition, personality and in the performance of complex motor tasks (apraxia) and are accompanied by seizures, then this is more in keeping with PML.
Why is PML so common in pwMS?
PML was quite rare in pwMS. Before the era of immunosuppressive DMTs, there were no reports of PML occurring in someone with MS. This may be an ascertainment bias in that someone with MS who developed PML in the past, may have simply been misdiagnosed as having worsening or malignant MS. PML is particularly a problem with natalizumab treatment. Natalizumab blocks the trafficking of lymphocytes into the central nervous system (CNS) and thereby prevents the immune system from surveying the brain and spinal cord for viruses. PML also occurs with other immunosuppressive therapies and has been described in patients on fingolimod, dimethyl fumarate, rituximab and ocrelizumab. In these cases, the PML was not related to prior natalizumab treatment, i.e. it was carried over from natalizumab. There have been pwMS who have developed PML on alemtuzumab, teriflunomide, fingolimod, rituximab and ocrelizumab as a carry-over from previous natalizumab therapy. We assume that the PML was asymptomatic when these patients stopped natalizumab and they only presented after they had switched to another DMT. PML is defined as carry-over PML if it occurs within 12 months of stopping natalizumab. However, I don't think the risk from natalizumab ever goes away. This is because PML is a complex disease that takes time to develop. The JCV virus has to acquire several mutations to allow it to cause PML. These mutant strains may persist in the body long term and hence increase your risk, or at least lower your threshold, for developing PML in the future if you remain on immunosuppression.
How do you diagnose PML?
PML is diagnosed clinically with the aid of an MRI scan and cerebrospinal fluid to detect the virus using a lab test called JCV-DNA PCR. Occasionally, a brain biopsy is required to make the diagnosis, but this is required much less often nowadays.
Who is at risk of developing PML?
Everyone who is JCV-seropositive is at risk of PML. If you are JCV-seronegative, you are at very low risk of PML, with the one caveat that you may become infected with the virus. Between 0.5% and 2% of pwMS who are JCV-seronegative become positive annually. If you are JCV seropositive, your risk increases with the duration of treatment; it is particularly low if you have been on natalizumab for less than 12-24 months. The level of antibodies against JCV also predicts risk; people with a raised anti-JCV index are at a higher risk. Please note that not all anti-JCV positive pwMS shed virus; therefore, a subset of pwMS with antibodies to the virus may have cleared the virus from the body and hence be at low risk of PML. This may explain why a persistently low index of antibodies to JCV indicates a low risk of PML. This may simply indicate past infection and no active infection at present. In contrast, those with a high level of antibodies, or a rising level of antibodies, have an ongoing active infection, which boosts the antibody response. This indicates the virus is active, possibly mutating, and hence these patients are at much higher risk of developing PML.
PwMS who have previously been on immunosuppressive therapy, for example, mitoxantrone, azathioprine, or any other immunosuppressive DMTs, are also at high risk of developing PML. Immunosuppressive therapies, presumably allow the virus to escape immune surveillance and acquire the necessary PML-associated mutations and put you at higher risk. Immunosuppressive therapies also blunt the immune response to the virus and affect the JCV antibody index and make it unreliable; in other words, a low index in pwMS previously exposed to immunosuppression is still at high risk of developing PML. Therefore you cannot use the anti-JCV antibody index in pwMS previously exposed to immunosuppressive therapy.
What is my risk of developing PML on natalizumab?
The following table and graph summarise these risk factors. Another bit of information that is missing is data on extended interval dosing of natalizumab. It looks as if receiving natalizumab every 5 or 6 weeks, i.e. extended interval dosing or EID, dramatically reduces your risk of getting PML.
What about switching from natalizumab to another DMT?
A switch is relatively straightforward if you are JC virus seronegative and are switching because of lack of efficacy, or for a lifestyle choice, for example, if you are tired of monthly infusions or you want an IRT (immune reconstitution therapy) that offers you the freedom to fall pregnant without worrying about rebound activity, or you simply prefer the long-term potential that an IRT has to offer. In this situation switching from natalizumab without a wash-out period to prevent rebound disease activity after natalizumab makes sense and should be relatively safe (option 1 below).
The situation if you are JC virus seropositive is much more problematic because of the risk of carry-over PML. With a maintenance agent such as fingolimod, we try and exclude asymptomatic PML by doing an MRI and a lumbar puncture to look for JCV DNA in the spinal fluid. If these tests are clear, we start fingolimod as soon as possible after the last natalizumab infusion with the knowledge that if PML should develop, we can always stop fingolimod, which will be cleared from the body within in 4-6 weeks. This early switching strategy prevents rebound activity when natalizumab wears after approximately 3-4 months.
With an IRT, such as alemtuzumab, things are more complicated because we can't reverse their action of alemtuzumab once it is given hence we have to be confident that there is no carry-over PML. Why am I so concerned? If you develop carry-over PML post-alemtuzumab before reconstitution of your immune system, you are likely to succumb to the PML. I am aware of one pwMS who has died under these circumstances. This is because we must rely on a functioning immune system, particularly a population of cells called CD8+ cytotoxic T-lymphocytes (CTLs), to clear the JC virus from the brain. CD8+ lymphocytes take many months to reconstitute post-alemtuzumab and other IRTs, during which time PML is unchecked and causes severe damage.
Many of you argue that by treating MS, a disabling disease, with immunosuppressive therapies, we simply create another ticking time bomb and swap one disease, MS, for another disease, immunosuppression. The difference between these two diseases is that MS-related disability is generally irreversible and associated with loss of quality of life. Immunosuppression, on the other hand, can be derisked to some extent and its consequences, particularly the opportunistic infections, treated. For more information, please read the Newsletter on derisking DMTS and specific information about each DMT. However, the poster child for derisking opportunistic infections must be natalizumab-associated PML. We now know that pwMS who are JCV-seropositive either need to come off natalizumab or switch to EID because of the risk of PML. In the high-risk subjects who decide to stay on natalizumab, we offer them 3-4 monthly MRI studies to look for asymptomatic PML. People diagnosed with asymptomatic PML and have their natalizumab stopped have a much better prognosis than pwMS who develop symptomatic PML before their natalizumab is stopped.
Can you treat PML?
The short answer is no. There have been some potential treatments proposed for PML, but none have shown to work. In the MS context, it is clear that you need immune reconstitution to clear the virus from the brain, and herein lies the problem. When you wash out natalizumab with either plasma exchange or by waiting for it to wash out spontaneously, your immune cells start re-trafficking into the brain, and you develop an encephalitis. This is called IRIS (immune reconstitution inflammatory syndrome). IRIS in itself can be quite dangerous. Therefore in patients with a large PML burden or PML in strategic brain areas such as the brainstem, we tend to give steroids to try and dampen down the damage associated with IRIS. Anecdotal experience suggests steroids work. Is there another strategy that we can try? There have been case reports describing the anti-HIV drug maraviroc, which blocks a particular chemokine receptor CCR5 on lymphocytes, and may help prevent or dampen down IRIS. T-cells, including cytotoxic CD8+ T-cells, use the CCR5 receptor to cross the blood-brain-barrier. Blocking CCR5 seems to dampen down IRIS and appears to prevent IRIS-related damage in these two cases. Clearly, maraviroc as a monotherapy is not enough to stop the immune system from clearing the JC virus from the CNS. The question that arises is whether or not maraviroc is better than steroids in achieving this. The latter will require further clinical trials.
The mainstay of treating PML in the context of natalizumab treatment is the reversal of the natalizumab effect. To speed this up, we can do plasma exchange, i.e., remove the plasma and the circulating natalizumab. As soon as the natalizumab levels in the peripheral blood drop low enough, the receptors become active again, and immune system re-trafficking occurs and allows your T cells to fight the infection. A problem arises when we can't reconstitute CNS immunosurveillance. This can happen after being treated with IRTs, particularly alemtuzumab and possibly cladribine, or people with persistent lymphopaenia. This is where immunotherapies are needed. One strategy is to give unfortunate people with PML in this situation donor anti-JCV lymphocytes that are matched to their HLA (human leukocyte antigens) to fight the infection. This is an immune transplant, i.e. giving them donor-matched T-lymphocytes to fight JCV. This strategy has been shown to work; T-cells designed to attack the BK virus that cross-react with JCV have helped several people recover from PML when they would have been expected to have died.
The number of cases of natalizumab-associated PML is falling, and I hope it becomes a rare complication of this treatment. Now that we have derisking strategies, and other highly-effective DMTs which are safer do we really need to continue to put pwMS at such a high risk of PML? I suspect yes. Natalizumab is one of the most effective and rapid-acting of all the DMTs at our disposal, and it’s reversible. This is why we are planning to test it in a study called the Attack-MS study to see if very early treatment with natalizumab, i.e. within 14 days of onset of the initial attack, results in a better outcome compared to a delayed start, i.e. after eight weeks, which is the average time it takes in the NHS to gets someone onto a treatment. If the Attack-MS works, then I see a future of us treating MS like we treat stroke; urgently to protect the brain and spinal cord from any further damage that could accrue in the initial few weeks.
Finally, we may, in future, have effective antivirals that clear the body of JCV. This would then allow us to use natalizumab without the threat of PML. Please note that until we get a drug that clears JCV from the body, we will never derisk the PML problem completely. As you are aware, PML is a complication of immunosuppression and therefore, it will remain a rare complication of other immunosuppressive therapies and MS treatments.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.




The other interesting thing with Tysabri is how many people really love it compared to B cell depleters etc
Trauling thru Facebook / social media so many patients on Tysabri rave about it and even when switching to other DMTs. But I don't see the same in Ocrevus groups or others...wonder why that is?
Many thanks for your explanations and rationale - they provide me with greater understanding of the situation I find myself in and help give me confidence that I'm making the best possible choice of new medication. Much appreciation for you taking the time to reply - it makes so much difference!