Do I have active MS?
Before deciding to start a disease-modifying therapy you need to know if you have active MS.
Yesterday, I received this direct message on Twitter: “… I am quite confused - I had a diagnosis of optic neuritis in 2012, zero relapses since, lesions on MRI seem stable, never had any medication - do you honestly think yearly MRI and DMTs are necessary?”
This is the kind of question that this MS-Seflie newsletter is here to answer.
Before making a decision about starting a disease-modifying therapy you need to understand MS and the principles underpinning the decision-making processes. i.e. you need to know and understand the answers to the following questions. For this case above, let’s assume they have MS. To be eligible for DMTs you have to have active MS.
What is multiple sclerosis (MS)?
Am I sure that I have MS?
What type of MS do I have?
What prognostic group do I fall into?
What is the risk of not being treated with a disease-modifying therapy (DMT)?
Do I have active MS?
Am I eligible for treatment with a DMT?
What is the difference between a maintenance/escalation DMT and an IRT (immune reconstitution therapy)?
Do I understand the difference between short-term intermittent and long-term continuous immunosuppression?
Do I understand the concept of treat-2-target?
What are the attributes of the specific DMTs?
How can I derisk or reduce my chances of getting certain adverse events on specific DMTs?

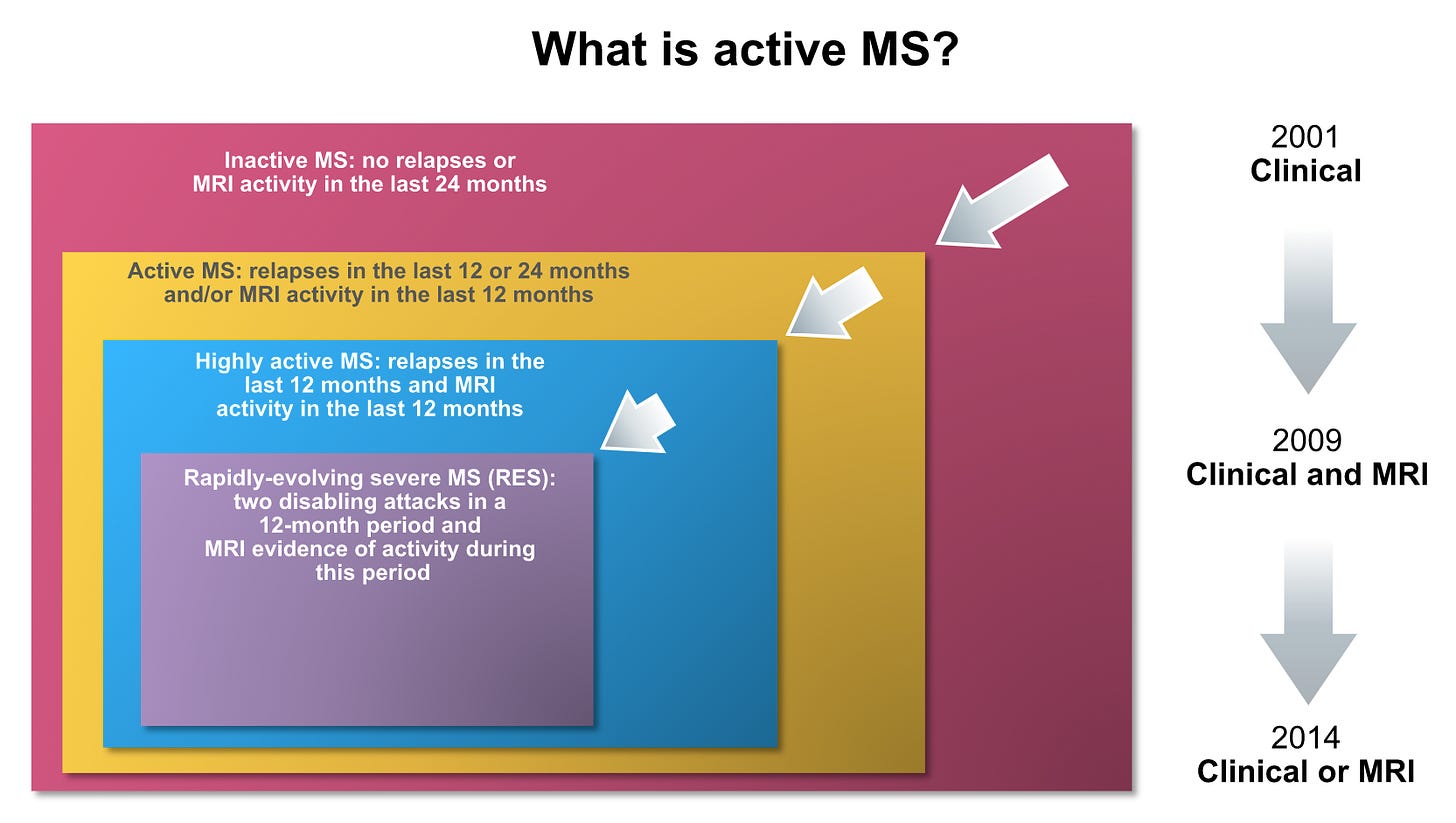
Active MS is the term that's increasingly being used to refer to current or recent evidence of focal inflammatory activity, i.e. new lesions on MRI or relapses. In contrast, the gradual worsening of disability that occurs in people with more advanced MS (which may, or may not, occur in the presence of focal inflammatory activity) has many potential causes, only one of which is focal inflammation. Inflammation damages axons, or nerve processes. When the lesion develops it can cut, or transect, the axons, demyelinate them or stop them from working. This is due to the effects of inflammatory mediators.
Relapses
When a new MS lesion occurs in an eloquent part of the central nervous system it causes new, or an exacerbation of old, symptoms that are usually interpreted as a relapse. Relapses by definition involve new symptoms, or an exacerbation of old symptoms, that last at least 24 hours in the absence of an infection or a fever.
Intermittent symptoms or pseudorelapses
Unfortunately, a large number of pwMS experience frequent intermittent symptoms that come on when they are tired, after exercise or have a raised body temperature from a fever, exercise, hot bath or a warm environment. These intermittent symptoms are usually quite stereotyped and last minutes to hours. They are indicative of a previously damaged pathway.
Asymptomatic lesions
Most of the focal MS disease activity that occurs does not cause any overt symptoms because the brain has a way of compensating for damage. For every clinical relapse there at least 10 or more lesions that come, and potentially go, on MRI. Therefore what we see clinically in terms of relapses is the tip of the iceberg. Even standard MRI is relatively insensitive in detecting and monitoring MS disease activity. The standard MRI misses new lesions that are smaller than 3-4 mm in size and does not detect the majority of lesions that occur in the grey matter of the brain (cortex and deep grey matter nuclei, e.g. thalamus and basal ganglia). Therefore MRI activity is also the tip of the iceberg. This is one of the reasons we have started using spinal fluid, or CSF neurofilament levels, as a marker of this microscopic activity.
Disease activity
Active MS
Most neurologists require evidence of disease activity in the last 12 months, with some of us accepting a 24-month window if there is no serial MRI support. The corollary of this is if you have had no relapses in the last 24 months, and serial MRI studies covering this period show no new lesions, then your MS is defined as being inactive. This does not mean your MS is necessarily stable. I have already said you could have worsening disability as part of the progressive phase of the disease. If you have so-called inactive MS you need to be monitored, as inactive MS may reactivate and you could then become eligible for treatment.
In the early 2000s, we used to define disease activity using clinical criteria only; i.e. you needed to have at least 2 documented relapses in the last 2 years to be eligible for DMT. This meant you needed to be seen by a neurologist so that he/she could examine you to confirm abnormalities on examination compatible with a relapse. The problem with this is that many pwMS who didn’t have rapid access to a neurologist would recover from their attack before being assessed, so many of their relapses could not be documented. This was very frustrating for pwMS wanting to start a DMT, as some neurologists were not prepared to accept historical attacks. I remember seeing lots of patients for a second opinion over this issue, as a kind of arbitrator to decide who was right: the assessing neurologist who would not accept undocumented historical relapses or the patient who knew they had had a relapse. I tended to give patients the benefit of the doubt, particularly if they had MRI evidence to support recent disease activity. How could we deny patients access to a DMT because they couldn’t be seen in a timely way to have their relapse documented in the clinical notes?
In 2009 our criteria incorporated MRI into the definition to allow us to treat so-called high-risk patients with CIS (clinically-isolated syndromes compatible with demyelination). These criteria required patients with CIS to have 9, or more, T2 lesions on MRI or at least one Gd-enhancing lesion. These MRI criteria were based on the McDonald diagnostic criteria at the time. I personally have never agreed with them. What makes someone with 2 lesions on MRI different from someone with 20 lesions on MRI? It could simply be that the person with 20 lesions has had asymptomatic MS longer than the person with 2 lesions on MRI. If we adopt the principle of treating MS early to prevent damage, why would we want to wait for the patient with CIS to acquire more lesions and hence more damage before offering them a treatment? I take the position that a pwCIS presenting with a low lesion load is lucky in that they presented early with their disease and hence have a greater opportunity to benefit from early treatment. The pwCIS with a high lesion load unfortunately is the unlucky one. This dilemma is really only a UK problem; outside of the UK, almost all neurologists offer pwCIS DMTs if they have two or more lesions on MRI.
In 2014 NICE (The National Institute for Health and Care Excellence) gave us permission to use alemtuzumab in adults with active relapsing MS defined clinically or on MRI (see below). This could mean defining activity based on MRI only. I doubt NICE or the EMA realised the implications of this ruling. I suspect the "OR" refers to re-treatment criteria and not the treatment criteria to initiate treatment. It would be hard to justify, in the current climate, starting alemtuzumab in pwMS without any recent clinical activity, i.e. relapses. In fact, some of my colleagues are refusing to offer alemtuzumab at all; they have taken the position that the therapy is too risky to justify its use as a first or even second-line therapy. I think their position is unacceptable; it is not them taking the risk but their patients.
Rapidly-evolving severe MS
For those of you who have active MS, there is are a further two subdivisions you need to know about. The first is so-called rapidly-evolving severe MS (RES), defined as two disabling attacks in a 12 month period with MRI evidence of activity during this period. This subgroup is eligible for natalizumab and fingolimod.
Highly-active MS
The other subgroup is the so-called highly active MS. These are pwMS with unchanged or increased relapse rates, or ongoing severe relapses compared with the previous year, despite treatment with beta-interferon, or another so-called first-line DMT. The latter definition is part of the NICE final appraisal determination for fingolimod. Please note that this exposes a quirk in the NHS system in that fingolimod can only be prescribed as second-line therapy in England. In contrast, natalizumab can be used as a first-line treatment in patients who fulfil the definition for having rapidly-evolving severe MS and alemtuzumab for pwMS who have active MS defined clinically or on MRI.
“… I am quite confused - I had a diagnosis of optic neuritis in 2012, zero relapses since, lesions on MRI seem stable, never had any medication - do you honestly think yearly MRI and DMTs are necessary?”
So based on the observation that this person doesn’t have active MS she would not be eligible for DMTs in the NHS. The questions I can’t answer is whether or not this person has ongoing smouldering MS, i.e. does she have slowly expanding lesions (SELs), accelerated brain volume loss, evidence of ongoing damage with raised neurofilament levels and/or evidence or persistently raised immunoglobulins in the spinal fluid. I would discuss these issues with this patient and probably offer them a more detailed assessment before stating that they don’t have active disease.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.



Prof G, you have emphasized many times MS is inflammatory from beginning to end and neurodegenerative from beginning to end. In other words there is no such thing as truly “inactive” MS. Therefore how can you ethically justify ever not putting someone with MS on a DMT? Aren’t you basically saying you’re OK with your “inactive” patients sustaining more brain damage than necessary simply because the DMT won’t have as much impact for them as for “active” patients? People with cancer are regularly given expensive drugs or treatments that extend life by only a few years or even a few months, why wouldn’t we apply the same thinking to saving brain in MS?
Another interesting article, thank you. I am 64 and recently had a contrast mri to see if my ms was active. It isn’t but when I asked does that mean it will never reactivate, the answer was almost certainly not.
I didn’t get diagnosed until I was 53 and had no problems until I was 62 and this article has helped me understand why my disability is getting progressively worse.
I was struck down with Ramsay Hunt at 62 syndrome and think the Tecfidera had possibly suppressed my immune system and from that time I’ve really noticed a physical decline. I’m now off the DMT.
Thanks for helping us all understand this awful disease!