Nutraceuticals is a term used to describe any product derived from food sources with potential extra health benefits over-and-above of the basic nutritional value found in the product. I am mentioning this because I spoke to a group of people with MS and their families at the Chilterns MS Centre on the weekend, and my slide on the holistic management of MS mentioned potential nutraceuticals.

Unlike pharmaceuticals, the main problem with nutraceuticals is that they are mainly unregulated; hence, we don’t have a sound evidence base to recommend their use as treatments for MS. Despite this, the nutraceutical healthcare market is enormous, with many people spending large amounts of their disposable income on unproven therapies.
I was asked at the meeting if I recommend nutraceuticals to patients with MS. Outside of vitamin D supplements that I recommend for bone health and as a potential preventive strategy for MS in children, siblings and the extended family of people with MS, I don’t make any other general recommendations regarding nutraceuticals.
Another nutraceutical I frequently recommend in individual patients is D-mannose as one component of a strategy to prevent urinary tract infections. I recommend lactulose, senna, psyllium husks and fibre supplements to manage constipation, and occasionally iron supplements for some patients with restless legs syndrome.
I don’t recommend multivitamin supplements. If you eat a balanced diet, you should be getting more than enough vitamins from your diet. The exception is a vegan diet, which is an unbalanced diet. Generally, vegans must take extra vitamin B12, zinc, iron, selenium, and possibly iodine, calcium, and some essential fatty acids (Please see my blog post ‘Calling all Vegans’; 6-Mar-2019).
From a scientific perspective, I am very interested in short-chain fatty acids that are either antioxidants or mimic ketosis, as they may be neuroprotective in MS. The most exciting are alpha lipoic, propionic and butyric acid. There is preliminary data supporting alpha lipoic acid as a neuroprotective agent in MS (see paper 1 below), and it is currently being investigated in the MS Society-supported OCTOPUS trial. Similarly, an emerging evidence base supports propionic and/or butyric acid as an anti-inflammatory and promoting remyelination (see paper 2 below).
Biohacking
In my talk, I also discussed, albeit very briefly, the concept of biohacking. Biohacking is largely a US phenomenon in which individuals ‘hack their biology’ to optimise health and wellness as an anti-ageing strategy. Biohackers use nutraceuticals, diet, exercise, mindfulness/meditation and pharmaceuticals. The most commonly used pharmaceutical is metformin, which reprogrammes your cells to counteract senescence and promote maintenance and recovery of function. Good animal data support the potential use of metformin in MS. Metformin reprograms senescent oligodendrocyte precursors so that they remyelinate as quickly as young mice.
Interestingly, at the latest European Charcot Foundation meeting in Baveno last year, Professor Robin Franklin gave a very erudite lecture on their work using metformin to rejuvenate the remyelination capability in aged rats. When he asked the audience, which consisted mainly of MSologists, for a show of hands to see who was taking metformin as an anti-ageing medication, about 15-20% of the audience raised their hands.
One prominent Canadian MSologist said at dinner that evening that after listening to Professor Franklin’s talk when he returned to Canada, he planned to double his metformin dose from 500mg twice daily to 1,000mg twice daily. Professor Franklin also implied in his talk that he was also taking metformin. Maybe this is why when someone with MS asked me if I recommend and/or prescribe metformin for my patients with MS, I said no, but rather hesitantly. However, I would not stop them from taking it off-label. If one in five MSologists is self-medicating with the drug and many biohackers are taking it as part of their core antiageing regimen, it is clear the metformin horse has already bolted. Despite this, metformin is one of the other interventions in the OCTOPUS trial. Metformin is also it is being studied in combination with clemastine to try and promote remyelination in pwMS (ClinicalTrials.gov Identifier: NCT05131828) and there are four other studies on the ClinicalTrials.gov site exploring metformin as a treatment for MS.

Diet
Please note nutraceutical advice overlaps with dietary advice. When it comes to diet, I don’t recommend any of the so-called ‘MS-specific’ diets. However, I suggest to my patients to try intermittent fasting and ketogenic diets based on the evidence that these diets may be neuroprotective, and many patients find that these diets improve their symptoms.
Please note when it comes to diet, it is horse-for-courses, and you need to work out what works for you. I suggest you read my MS-Selfie Newsletter ‘Which is the best MS diet?’ (25-Aug-2021), which explains my diet philosophy and some of my thinking behind intermittent fasting and ketosis. Please note butyric acid or butyrate supplements as nutraceuticals probably mimic IF and ketogenic diets; however, until we have more evidence, I would not recommend these supplements.
I would be interested to know what nutraceuticals you use and how you get along with them. For example, I am aware that many of my patients are already taking alpha lipoic acid and metformin, which might make it difficult for the OCTOPUS trial to recruit and give a definitive answer. I suspect the Octopus study will act as a catalyst for new generations of biohackers, which is a pity as we need a definitive answer on whether these two interventions slow smouldering-associated worsening (SAW) in pwMS.
Paper 1 - Lipoic Acid
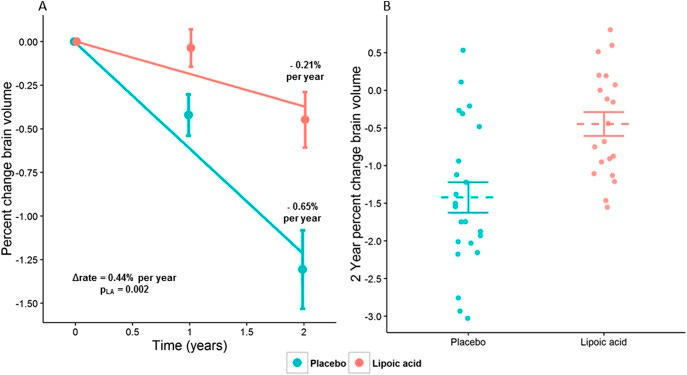
Objective: To determine whether lipoic acid (LA), an endogenously produced antioxidant, slowed the whole-brain atrophy rate and was safe in secondary progressive MS (SPMS).
Methods: Patients with SPMS aged 40-70 years enrolled in a single center, 2-year, double-blind, randomized trial of daily oral 1,200 mg LA vs placebo. Primary outcome was change in annualized percent change brain volume (PCBV). Secondary outcomes were changes in rates of atrophy of segmented brain, spinal cord, and retinal substructures, disability, quality of life, and safety. Intention-to-treat analysis used linear mixed models.
Results: Participation occurred between May 2, 2011, and August 14, 2015. Study arms of LA (n = 27) and placebo (n = 24) were matched with mean age of 58.5 (SD 5.9) years, 61% women, mean disease duration of 29.6 (SD 9.5) years, and median Expanded Disability Status Score of 6.0 (interquartile range 1.75). After 2 years, the annualized PCBV was significantly less in the LA arm compared with placebo (-0.21 [standard error of the coefficient estimate (SEE) 0.14] vs -0.65 [SEE 0.10], 95% confidence interval [CI] 0.157-0.727, p = 0.002). Improved Timed 25-Foot Walk was almost but not significantly better in the LA than in the control group (-0.535 [SEE 0.358] vs 0.137 [SEE 0.247], 95% CI -1.37 to 0.03, p = 0.06). Significantly more gastrointestinal upset and fewer falls occurred in LA patients. Unexpected renal failure (n = 1) and glomerulonephritis (n = 1) occurred in the LA cohort. Compliance, measured by pill counts, was 87%.
Conclusions: LA demonstrated a 68% reduction in annualized PCBV and suggested a clinical benefit in SPMS while maintaining favorable safety, tolerability, and compliance over 2 years.
Clinicaltrialsgov identifier: NCT01188811.
Classification of evidence: This study provides Class I evidence that for patients with SPMS, LA reduces the rate of brain atrophy.
Paper 2 - Propionic Acid
Short-chain fatty acids are processed from indigestible dietary fibers by gut bacteria and have immunomodulatory properties. Here, we investigate propionic acid (PA) in multiple sclerosis (MS), an autoimmune and neurodegenerative disease. Serum and feces of subjects with MS exhibited significantly reduced PA amounts compared with controls, particularly after the first relapse. In a proof-of-concept study, we supplemented PA to therapy-naive MS patients and as an add-on to MS immunotherapy. After 2 weeks of PA intake, we observed a significant and sustained increase of functionally competent regulatory T (Treg) cells, whereas Th1 and Th17 cells decreased significantly. Post-hoc analyses revealed a reduced annual relapse rate, disability stabilization, and reduced brain atrophy after 3 years of PA intake. Functional microbiome analysis revealed increased expression of Treg-cell-inducing genes in the intestine after PA intake. Furthermore, PA normalized Treg cell mitochondrial function and morphology in MS. Our findings suggest that PA can serve as a potent immunomodulatory supplement to MS drugs.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your own healthcare professional, who will be able to help you.













Share this post