A fact worth knowing
Did you know that people with MS who have a vascular comorbidity (smoking, obesity, hypercholesterolemia, hyperlipidemia, hypertension and/or established vascular disease) need to use a walking stick about six years earlier than people who don’t have a vascular comorbidity? Now that you know this, you can’t unlearn it, so you need to do something about it.
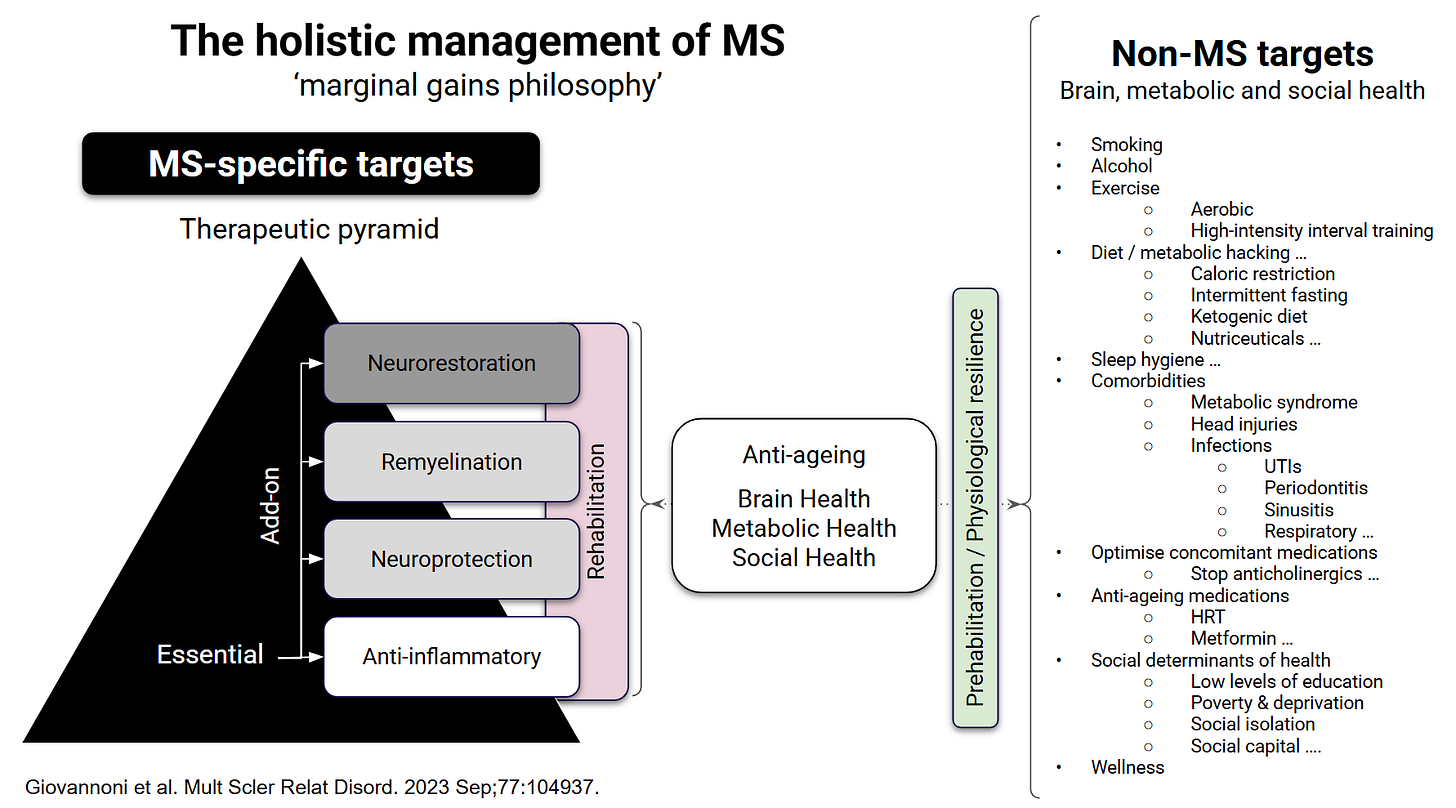
The holistic management of MS
I have been pushing the concept of the holistic management of MS with a focus on both MS-specific and non-MS factors for over a decade. It is clear that factors that are poor for brain health reduce brain reserve or resilience and are associated with worse MS outcomes.
A major contributor to poor MS outcomes is co-existing vascular comorbidities (smoking, obesity, hypercholesterolemia, hyperlipidemia, hypertension and established vascular disease), and people with MS are at increased risk of developing vascular comorbidities (see Marrie et al., below). This study from Canada showed that pwMS with vascular comorbidity reached EDSS 6.0 (needing a walking stick) on average 6 years earlier than pwMS without vascular comorbidities (~12 years versus ~18 years). This difference of 6 years is more significant than the treatment effect of interferon beta on slowing down the acquisition of disability progression. This is why we, as an MS community, need to be aggressive about the prevention and treatment of vascular comorbidities.
The good news is, at least for pwMS in the UK, that when diagnosed with hypertension and treated, they are more likely to reach the treatment target regarding their blood pressure (see Palladino et al. below). I suspect this is because pwMS have more contact with HCPs and may understand the importance of adhering to their medication.
Self-monitoring your BP
As you know, MS-Selfie stands for MS self-management and self-monitoring. I always encourage my patients to measure their blood pressure. My mistake is that I have assumed incorrectly that you know how to measure their blood pressure, which prompted me to write this newsletter.
I subscribe to Journal Watch, an NEJM publication that I read weekly. It is my way of keeping up with developments in general medicine. This week, I was surprised to read a summary of the article by Clapham and colleagues that home blood pressure measurements (HBPM) are not performed according to guideline recommendations, and adults who received ad hoc education did not perform high-quality HBPM. These findings highlight a need for effective teaching to support HBPM for clinical decision-making. This is why I have posted the American Medical Association guide on HBPM so you can refresh your memory.
In general, you should have your blood pressure checked at least annually and more frequently if you have risk factors for high blood pressure, a history of high blood pressure readings or have been diagnosed with hypertension.
I would be interested to know how many of you self-monitor your blood pressure and how many of you have self-diagnosed yourself as having hypertension.
Are these non-MS self-help newsletters helpful or simply clogging up your email inboxes?
Abstracts of interest
Background: Patient education is needed to perform home blood pressure measurement (HBPM) according to blood pressure (BP) guidelines. It is not known how BP is measured at home and what education is provided, which was the aim of the study.
Methods: Mixed-methods study among Australian adults who perform HBPM (June to December 2023). Participants completed a 30-item online survey on whether they followed guideline recommendations and the education they received for HBPM. Phone interviews were conducted among a purposive sample to further explore survey topics.
Results: Participants (n=350) were middle-aged (58±16 years; 54% women), and most (n=250, 71%) had hypertension. Guideline recommendations for HBPM were not always followed by survey participants. Most participants measured BP seated (n=316, 90%) with the cuff fitted to a bare arm (n=269, 77%). Only 15% measured BP in the morning and evening (n=54) and 26% averaged the BP readings over 7 days (n=90). Interview participants (n=34) described measuring BP at "different times of the day after doing different things." One-third of participants (n=112, 37%) received education for HBPM, which interview participants described as vague verbal instructions from health care practitioners. Participants who received education did not perform high-quality HBPM. Participants who did not receive education mimicked BP measurement methods of health care practitioners, "I do it the way I've seen them do it."
Conclusions: HBPM is not performed according to guideline recommendations, and adults who received ad hoc education did not perform high-quality HBPM. These findings highlight a need for effective education to support HBPM for clinical decision-making.
Background: Vascular comorbidity adversely influences health outcomes in several chronic conditions. Vascular comorbidities are common in multiple sclerosis (MS), but their impact on disease severity is unknown. Vascular comorbidities may contribute to the poorly understood heterogeneity in MS disease severity. Treatment of vascular comorbidities may represent an avenue for treating MS.
Methods: A total of 8,983 patients with MS enrolled in the North American Research Committee on Multiple Sclerosis Registry participated in this cohort study. Time from symptom onset or diagnosis until ambulatory disability was compared for patients with or without vascular comorbidities to determine their impact on MS severity. Multivariable proportional hazards models were adjusted for sex, race, age at symptom onset, year of symptom onset, socioeconomic status, and region of residence.
Results: Participants reporting one or more vascular comorbidities at diagnosis had an increased risk of ambulatory disability, and risk increased with the number of vascular conditions reported (hazard ratio [HR]/condition for early gait disability 1.51; 95% confidence interval [CI] 1.41-1.61). Vascular comorbidity at any time during the disease course also increased the risk of ambulatory disability (adjusted HR for unilateral walking assistance 1.54; 95% CI 1.44-1.65). The median time between diagnosis and need for ambulatory assistance was 18.8 years in patients without and 12.8 years in patients with vascular comorbidities.
Conclusions: Vascular comorbidity, whether present at symptom onset, diagnosis, or later in the disease course, is associated with a substantially increased risk of disability progression in multiple sclerosis. The impact of treating vascular comorbidities on disease progression deserves investigation.
Background: People with multiple sclerosis (PwMS) have an increased cardiovascular and cerebrovascular disease burden, but this could be mitigated by vascular risk factor management.
Objectives: We compared the trajectories of vascular risk factors, vascular comorbidities and clinical management in PwMS against the general population post-MS diagnosis while controlling for frailty.
Methods: Retrospective longitudinal analysis using English data from the Clinical Practice Research Datalink between 1987 and 2018 comprising PwMS matched with up to six controls without MS by age, sex and general practice.
Results: We compared 12,251 PwMS with 72,572 matched controls; 3.8% of PwMS had mild-moderate frailty, 1.2% more than matched controls. Compared to controls, PwMS had an elevated incidence of Type 2 diabetes (HR 1.18, 95% CI (1.04, 1.34)), and starting antihypertensive medications (HR 1.40, 95% CI (1.33, 1.47)). Among those with hypertension at baseline, blood pressure trajectories did not differ between PwMS and controls. PwMS had increased rates of meeting targets for hypertension management (HR 1.25, 95% CI (1.12, 1.41)).
Conclusion: The observation that PwMS with hypertension are more likely to meet treatment targets than matched controls is encouraging, but the elevated rates of vascular comorbidities suggest that tighter vascular management may be needed in this population.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.














Share this post