Which is the best MS diet?
Prof G tries to tackle the thorny issue of diet and MS. Which diet should I eat to manage my MS? Can diet really be disease-modifying?
I am always being asked about the ideal diet for someone with MS.
The simple answer is there is no ideal MS diet. What you eat is about personal choices and has to be compatible with your cultural background and your social and economic circumstances. There is so much more to eating food than what you actually eat.
Most HCPs when giving advice about diets default to the ‘heart-healthy’ diet. However, since the scandal surrounding the low-fat ‘heart-healthy’ recommendations having been exposed as not being evidence-based and being heavily influenced by the food industry it is difficult to know what diet to recommend. I even have serious doubts about the so-called Mediterranean diet, which is a very nebulous entity and in all likelihood was invented and promoted as a marketing tool for the olive oil industry. You will find it difficult to find a place that eats the typical Mediterranean diet.
I, therefore, propose using evolutionary medicine when it comes to my dietary advice, which can be summarised as five principles.
Eat socially
Eat real food, i.e. avoid processed and ultra-processed food
Eat local
Eat seasonally
Eat mindfully
Eat Socially
Eating is or at least it should be a social activity. Meals should be about sitting down with family, friends and colleagues and enjoying each other's company. A lot of our rituals, religious and non-religious, revolve around eating; often in the form of feasts. If your diet prevents you from using meal times as a social activity it will impact your social capital and hence health outcomes.
If I don’t eat my evening meal with family and/or friends my day feels strangely incomplete. The same goes for our ritual Sunday family roast. I look forward to preparing the Sunday roast and enjoying it with my family; a week without our family roast is an incomplete week.
Eat real food
Real food is knowing its provenance and being able to identify what it is. In general, real food is whole, single-ingredient food. It is mostly unprocessed, free of chemical additives, and rich in nutrients. In essence, it’s the type of food we ate exclusively for thousands of years and it's the type of food that drove our evolution. The types of real food that are processed include fermented, cured and dried foods. The fermentation process is used to preserve food when they are abundant for times of scarcity and to help with digestion. For example, the move from eating sourdough or slowly fermented bread using a wild culture (yeasts and bacteria) to modern ultra-processed bread with added sugar to catalyse rapid fermentation using a monoculture (single yeast species) is hypothesised to be one of the reasons for the rise in gluten sensitivity. The wild sourdough culture includes not only yeast but symbiotic bacteria that break down gluten differently from monoculture yeast used in industrial bread production.
The main problem with processed and ultra-processed food is what it does to our metabolism. Complex (unprocessed) carbohydrates tend to have a low GI index (unless you juice them), i.e. they release their sugars slowly and induce less insulin. In comparison, processed foods are high in carbohydrates and have a high glycaemic index (GI). High GI foods don’t need much digestion and hence release their sugars very quickly, which are rapidly absorbed, which then stimulates high levels of insulin, which activates the body to process the high sugar levels. We now know that insulin is not only produced for sugar in the here and now but also as an anticipatory hormone. The insulin response expects sugars to be absorbed over several hours, which is what happens with low GI foods or real food.
The excess insulin in response to high GI, or processed foods, then lowers your glucose levels causing relative hypoglycaemia. This occurs because processed sugars are rapidly absorbed from your intestine without a long absorption tail that we see with low GI complex carbohydrates. Low blood glucose after high GI foods triggers a hunger response and drives one to seek more food. As this occurs between meals it results in snacking between meals. In studies when people eat a diet high in processed and ultra-processed foods they consume over 500 calories more a day compared to periods when they eat a real-food diet. This extra calorie intake would have almost certainly been driven by the excess insulin-induced hypoglycaemia from high GI foods and resulted in more weight gain.

Try and avoid processed and ultra-processed foods, with the exception of traditionally prepared fermented foods; know their provenance.
Eat local
Eat local is about the environment and supporting your own farmers. The economic and environmental arguments for this are well-rehearsed. Why eat foods with a large carbon footprint when you can eat local sustainable foods. I try to buy local, but it is not always possible because the agribusiness is now a global industry that controls the food environment we live in. Eating local produce needs political support to make it happen on a large scale. If you are passionate about this get involved in politics.
Eat seasonally
For the evolutionary medicine purist, this makes sense. It is particularly important to eat seasonally in relation to carbohydrate metabolism. Interestingly a lot of chefs understand this concept and will only present seasonal menus in their restaurants. I suspect the reason for this is they understand the importance of the seasonal cycle to our metabolism. We pay a massive price by ignoring the seasonal rhythms in relation to our diets and metabolism.
Eat mindfully
Pay attention to what you eat and think about it in the moment, i.e. your own thoughts and feelings about the food you are eating and the impact this is having on those around you and the environment. Being mindful will challenge you when you are eating for comfort and not because you are hungry or being sociable. This will also allow you to adopt an environmentally friendly diet.
Mindful eating is compatible with the slow food movement which envisions a world in which all people can access and enjoy food that is good for them, good for those who grow it and good for the planet. The slow food movement is based on a concept of food that is defined by three interconnected principles: good, clean and fair.
GOOD: quality, flavoursome and healthy food
CLEAN: production that does not harm the environment
FAIR: accessible prices for consumers and fair conditions and pay for producers
So, in summary, I don’t think there is a right answer when it comes to diet. However, if you adopt some of the basic principles above your diet will contribute to your overall wellness.
Diet as an MS disease-modifying therapy
The question about diet being an actual treatment for MS, however, is a different question. Here I would support a ketogenic diet and intermittent fasting.
Studies of caloric restriction (CR), intermittent fasting (IF) or ketogenic (K) diets in animal models of MS demonstrate a disease-modifying effect, i.e. fewer attacks and less disability. The mode of action of all these diets is probably via ketosis and inducing high levels of circulating β-hydroxybutyrate, a so-called ketone body. Ketone bodies are the source of energy the body uses when we have depleted our sugar stores (glycogen) and are fasting or not absorbing sugar from the gut.
Interestingly, β-hydroxybutyrate works via the hydroxycarboxylic acid receptor 2 (HCA2), which is also known as niacin receptor 1 (NIACR1) and GPR109A. Why is this so important? This is the same receptor that fumaric acid works on. Yes, ketosis works at a cellular level in the same way that dimethyl fumarate (DMF) and diroximel fumarate work, i.e. two licensed MS DMTs.
Yes, CR/IF/K diet may induce a metabolic pathway that is known to be disease-modifying in MS.
There is extensive literature, which I discovered about two years ago, showing that β-hydroxybutyrate works via NRF2, a transcription factor that acts as a metabolic switch in our cells. NRF2 downregulates NFKappa-B, the master inflammatory transcription factor. In other words ketosis, in particular, β-hydroxybutyrate is anti-inflammatory and stimulates a programme called programmed cell survival. The latter pathway has been shown to be antiageing and neuroprotective in many different animal models. β-hydroxybutyrate may even be better than the fumarates as a treatment for MS because it is likely to penetrate the CNS better than oral fumarates.
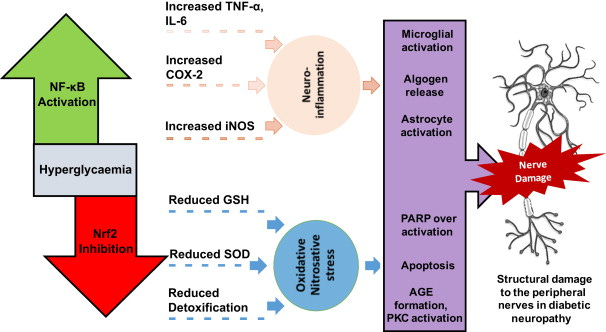
The corollary of the above could also explain why a processed and ultra-processed high carbohydrate diet is pro-inflammatory. Most people put it down to the pro-inflammatory signals from adipose tissue, but it could be related to the fact that carbohydrates, via insulin, inhibit ketosis and suppress β-hydroxybutyrate levels in the body.
It is also noteworthy that metformin, a drug used to treat type 2 diabetes, also works via NRF2, but not via the HCA2 receptor. This may explain why metformin promotes rejuvenation of oligodendrocyte precursors and is being explored as a potential remyelination therapy in MS. Metformin is also being explored as an anti-ageing drug and is why many biohackers take metformin.
Some statins, including simvastatin, activate NRF2. This could also be the potential mode of action of simvastatin in MS and is why I am soo eager to find out the results of the phase 3 simvastatin trial in secondary progressive MS.
Despite observational evidence showing that pwMS do well on CR/IF/K diets, the data is really not good enough to say they are actually disease-modifying. However, the studies do show that these diets are generally safe. However, we need controlled evidence before promoting these diets to pwMS as a potential adjunctive treatment for MS. The good news is that there are ongoing studies looking into this.
Please note ketogenic diets and intermittent fasting are not incongruent with my diet philosophy.
I also don’t support one diet over another. The evidence that any diet is better than another is weak and a lot of dietary advice is not based on science. Person-specific factors, such as gut microbiome, have a greater influence than the diet in relation to metabolism and that genetic variation only has a modest impact on the metabolic responses to food linked to cardiometabolic disease. The only metabolic output that has been shown to be influenced by diet is blood glucose or sugar levels, which is dictated by carbohydrate intake and the type or quality of carbohydrates you consume.
In summary, apart from carbohydrate metabolism, it is horses for courses and personal factors (gut microbiome and genetics) which dominate how your diet impacts your metabolism.
The good news is you can manipulate your carbohydrate metabolism; it is relatively simple. Both ketogenic diets and intermittent fasting reduce your sugar intake and blunt or flatten your blood glucose levels and the subsequent downstream insulin response, which is clearly one of the bad guys in driving cardiovascular risk. I truly believe what is good for your heart is good for your brain and would suggest you explore altering your diet based on the principles above.
I hope you have enough information at hand for you to make an informed decision about your diet without having to ask your HCPs and to counter conflicting advice.
Subscriptions
I am raising funds from subscriptions to administer the MS-Selfie Newsletter and microsite. The subscriptions, for case studies only, will be used to hire an administrator to proofread, curate and transfer the contents of the Newsletter onto the companion MS-Selfie microsite. If you find these Newsletters helpful and can afford to subscribe I would urge you to do so; it will help me and the MS community. Thank you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.





I have been following a keto diet since I was diagnosed with MS in Dec 2018.i have had no relapses since then, and now I look at food in a totally different way. Yes, I have the occasional lapse esp when potatoes or parsnips are on offer, my weakness, but overall I have persisted in this. I am also going thru menopause, which doesn't help my brain fog, but I have kept my job as a nurse, which involves a LOT of thinking, and I think it works for me. So that's my story. I am also getting infusions of Tysabri every 6 weeks. I have RRMS, and I know I don't know what life holds for me in the future, but I can only try.
It's no wonder there is so much conflicting information on a one fits-all diet, they dont exist. Checking your DNA with promothease isn't too bad, it will tell you if you have a methyl-folate deficiency for example or a vitamin d deficiency(probable if you have MS). You can get a gut microbiome test done at microba.com, it will give you some insight on how well you can digest oxalates, fats or if you have bacteria involved in mitophagy(mitochondrial renewal). If you cant get a hold of metformin, berberine may be just as good or even better and doesn't need a prescription. You can also get a continuous glucose monitor if you'd like to track which foods spike your insulin(they are different for different people), the Apple watch series 7 may have this built-in, here's to hoping :)