Do we need to challenge the dogma that traditional MRI is good enough to monitor MS?
Our current treatment target in MS is no evident inflammatory disease activity or NEIDA. In other words, there should be no relapses or focal MRI activity (new or expanding T2 lesions or Gd-enhancing T1 lesions).
Question: Is the NEIDA treatment target appropriate?
I don’t think so for several reasons.
Not all relapses are relapses
If you have MS, you are likely to attribute new neurological symptoms, particularly if they persist, to a relapse. Can you be sure it is a relapse and not a pseudorelapse?
Differentiating pseudorelapses from relapses can be challenging, as pwMS are often unaware of preexisting deficits in the particular neuronal pathway from which the new symptoms arise. The recurrence of old symptoms, such as blurred vision in an eye previously affected by optic neuritis, is easy to understand. However, new symptoms in a pathway affected by smouldering MS are typically interpreted as a relapse. Smouldering MS gradually reduces the neurological reserve in a path that then becomes exposed when you have a pseudorelapse (see figure below).
Before the physical (exercise), cognitive (exam) or systemic insult (infection or pyrexia) that caused the pseudorelapse, the pwMS would say this pathway was unaffected by MS. It is only when it is stressed that the pwMS develop symptoms. The stressor acts as a neurological stress test to expose pre-existing damage, albeit in a neurological path not previously affected by a symptomatic relapse (please note that I refer to new Gd-enhancing lesions without symptoms as asymptomatic relapses).
In the future, we will distinguish between biochemically confirmed relapses (new focal inflammatory activity) and pseudorelapses by measuring blood neurofilament levels. A new lesion will likely cause new damage, transecting axons and releasing neurofilaments into the blood. In comparison, pseudorelapses are caused by a temporary conduction block in a previously damaged pathway and will not be associated with a neurofilament spike. Relapses will be classified as “biochemically confirmed” or “biochemically unconfirmed” relapses, with the former being much more severe.
Please be aware that only three of four relapses (75%), confirmed by a neurologist, are associated with new MRI activity (new or Gd-enhancing lesions), i.e. only 75% of relapses are MRI-confirmed. I am aware that many of these MRI unconfirmed relapses are associated with raised neurofilament levels, which may be more sensitive in detecting or confirming ‘true relapses’. This indicates that many MRI unconfirmed relapses are likely to be due to small lesions below the detection threshold of the MRI or stress-induced symptoms and signs due to loss of reserve from smouldering MS.
This is why we must challenge the current dogma and definition of a relapse; patient-reported and physician-determined relapses are not good enough to document relapse disease activity.

What about Gd-enhancing lesions?
The detection of Gd-enhancing lesions depends on how frequently you are scanned, the dose of gadolinium administered, how long the radiographer waits before repeating the T1 scan to detect enhancement and the neuroradiologist who reads the scan. You should wait at least 10 minutes after the IV administration of gadolinium before repeating the T1 scan. I know many patients have their repeat scan done earlier than 10 minutes. The reason is that radiographers are impatient in completing the scan before moving on to the next patient. In healthcare, time is money, so the quicker you process patients, the more time you have to scan additional patients. If, on the other hand, you are prepared to wait 20 minutes after the administration of Gd before repeating the T1 scan, you are much more likely to find gadolinium-enhancing lesions. A similar story is true for triple-dose versus single-dose gadolinium. Finally, I have also seen many MRI reports being changed from non-enhancing lesions to enhancing lesions after a second opinion. I am sorry to disappoint you. Nothing is black and white regarding whether or not Gd-enhancing lesions are detected on MRI.
Will enlarging T2 lesions be better?
Labelling an enlarging T2 lesion as enlarging due to focal inflammation secondary to an adaptive immune response (B & T cells) from the periphery may also be a wrong call or dogma. Chronic active lesions, either PRLs (paramagnetic rim lesions) or SELs (slowly expanding lesions), become more prominent with time due to what we think is from innate immune activity and not necessarily from the influx of adaptive immune cells such as T and B lymphocytes. Can we, therefore, expect peripherally acting anti-inflammatory treatments to affect PRLs and/or SELs?
This will come to a head when the T2 lesion data from the tolebrutinib study is analysed differently. Does it have a more significant effect on new T2 or enlarging T2 lesions? I predict the latter, as the data from the relapsing tolebrutinib trials, the Gemini 1&2 studies, suggest that tolebrutinib impacts how T2 lesions evolve, i.e., how much innate immune activation remains after a new Gd-enhancing lesion.
Another curved ball for the MS community was the recent MS-Base study referenced below, which showed that high-efficacy DMTs were superior to low-efficacy DMTs in suppressing new lesion activity on brain MRI but not on new spinal cord lesions. The data from this study suggest that the biology of spinal cord lesions differs from that of brain lesions. Despite these patients being primarily NEIDA, spinal cord lesions appeared over time. Could these new T2 spinal cord lesions be SELs that evolve from microscopic lesions and don’t have a Gd-enhancing or relapsing phase? I say this as the current dogma states that new spinal cord lesions are more likely to be symptomatic, and this is the main reason we don’t do annual or regular spinal cord monitoring MRI scans.

In the past, I was told that spinal cord activity and brain activity cluster, i.e., if you develop new lesions in the spinal cord, you are also likely to develop new brain lesions in parallel. This is another reason why brain MRI monitoring is meant to be sufficient to detect MS disease activity. Again, this dogma needs to be challenged.
We may have to revisit this position as we seem to be missing important MS disease activity, albeit smouldering disease activity, that is not seen on brain MRI but on spinal cord imaging.
What about new T2 lesions?
Whether new and expanding T2 lesions can emerge spontaneously without going through a Gd-enhancing phase has become a critical question for the field of MS. Based on my worldview of MS, I would say yes. The MS-Base paper on the spontaneous appearance of new T2 spinal cord lesions is evidence of this. These lesions have emerged as largely asymptomatic lesions in pwMS on DMTs who are relapse-free. This implies they are emerging from the spinal cord and are independent of relapse or focal inflammatory disease activity, hence representing smouldering MS.
A counterargument is that DMTs are ineffective in suppressing all focal inflammatory lesions, particularly those that are microscopic below the scanning resolution of current MRI scanners. It is vital to note that using high-efficacy DMT in patients with PIRA reduces the likelihood of long-term persistence and further PIRA events compared to lower-efficacy DMTs (see Zhu et al. below).
The late Professor Giancarlo Comi always pointed out that just because you are not detecting focal inflammatory lesions clinically as relapses and/or on MRI does not mean that focal inflammation is not occurring. Sorting this out is critical for the future treatment of MS, as some people with apparent SAW may need to switch DMTs to suppress microscopic focal inflammation, and others may need a combination approach to add-on treatments to address SAW (smouldering-associated worsening).
The following is a figure I have been working on to try and explain the evolution of MS lesions on MRI. Does it make sense to you?
IM-SMOULDERING Trial
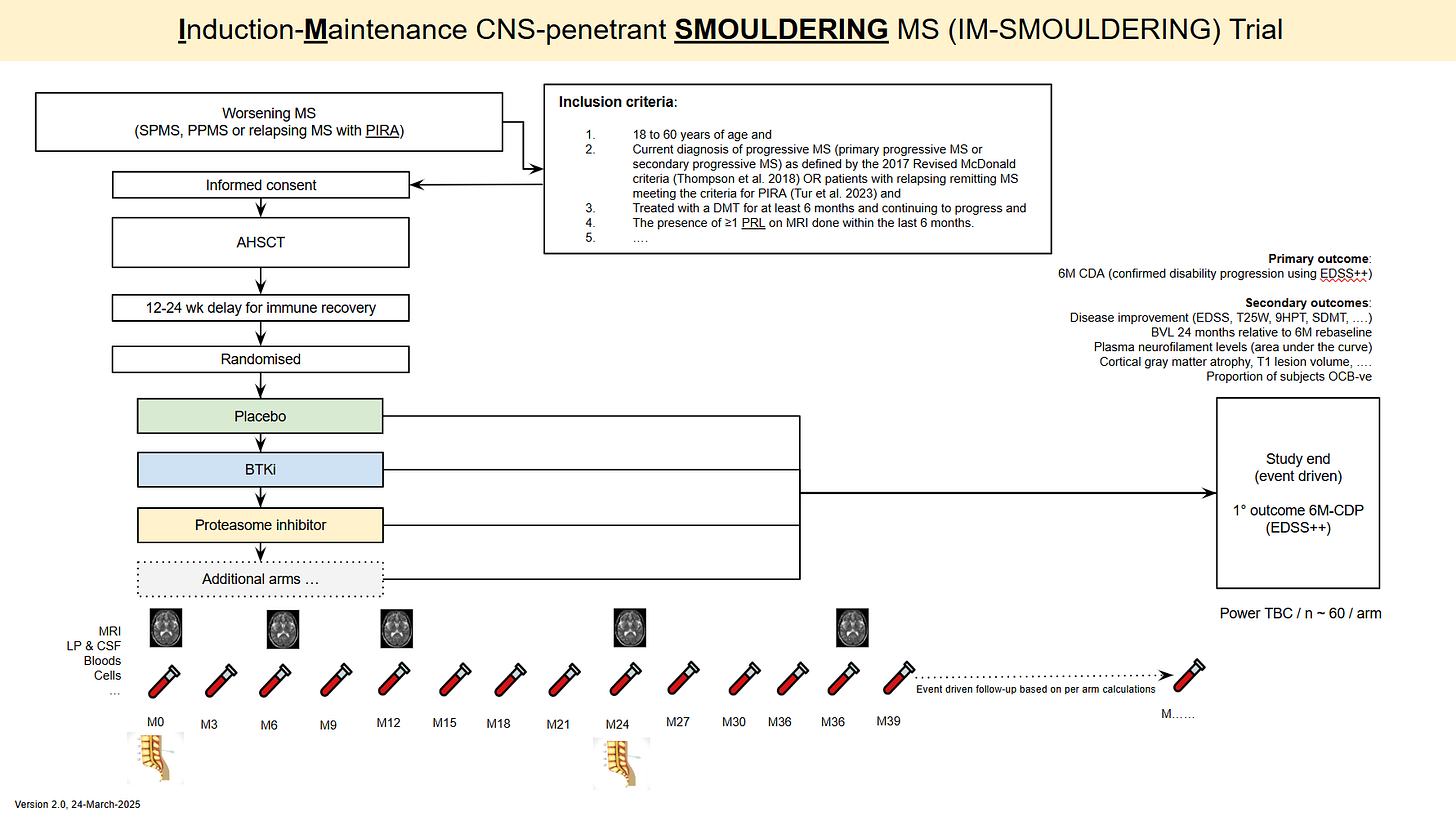
This is why we are proposing to test an induction maintenance strategy in patients with smouldering MS followed by an add-on CNS penetrant therapy to target smouldering MS. To be eligible for the trial, you have to have smouldering MS as detected by a PIRA event (progression-independent of relapse activity) and PRLs on your baseline scan. The latter is to enrich the study for pwMS, who are more likely to worsen in the future, i.e. having further PIRA events.
We want to use AHSCT as the induction therapy as it is the most effective therapy we have and puts a large number of people with MS into remission. Do you agree with this? We need feedback from the MS community for our grant application. So, if you can spare two minutes, I would appreciate it if you could complete this short survey.
Thank you.
Paper 1
Background: Spinal cord lesions in multiple sclerosis (MS) have considerable impact on disability. High-efficacy disease-modifying treatments (hDMTs) are associated with greater reduction of relapses and new brain lesions compared to low-efficacy treatments (lDMTs). Knowledge on the impact of DMTs on cord lesion formation is limited as these outcome measures were not included in MS treatment trials. This study aims to investigate whether hDMTs reduce the formation of cord lesions more effectively than lDMTs.
Methods: Patients with relapse-onset MS, a cord magnetic resonance imaging (MRI) within 6 months before/after initiation of their first DMT and ≥1 cord MRI at follow-up (interval > 6 months) were extracted from the MSBase registry (ACTRN12605000455662). Patients treated with hDMTs ≥90% or lDMTs ≥90% of follow-up duration were considered the hDMT and lDMT groups, respectively. Matching was performed using propensity scores. Cox proportional hazards models were used to estimate the hazards of new cord lesions, brain lesions and relapses.
Results: Ninety-four and 783 satisfied hDMT and lDMT group criteria, respectively. Seventy-seven hDMT patients were matched to 184 lDMT patients. In the hDMT group there was no evidence of reduction of new cord lesions (hazard ratio [HR] 0.99 [95% CI 0.51, 1.92], p = 0.97), while there were fewer new brain lesions (HR 0.22 [95% CI 0.10, 0.49], p < 0.001) and fewer relapses (HR 0.45 [95% CI 0.28, 0.72], p = 0.004).
Conclusion: A potential discrepancy exists in the effect of hDMTs over lDMTs in preventing spinal cord lesions versus brain lesions and relapses. While hDMTs provided a significant reduction for the latter when compared to lDMTs, there was no significant reduction in new spinal cord lesions.
Paper 2
Introduction: Some patients with relapsing-remitting multiple sclerosis (RRMS) experience sustained disability progression independent of relapse activity (PIRA), which can be a sign of early secondary progressive MS (SPMS). However, PIRA events may regress over time. Persistent PIRA indicates ongoing sustained disability or progression of disability without improvement, so understanding the factors that would predict this is crucial.
Objectives/Aims: To examine risk factors for persistent PIRA (defined as persisting to the end of follow-up) and the risk differences in long-term disability worsening between patients with persistent and non-persistent PIRA.
Methods: This cohort study used data collected from patients enrolled in the MSBase registry between April 16, 1995 and Jan 10, 2024. The median follow-up was 6.8 years.
The baseline was set at the time of PIRA occurrence. The primary outcome was time to 6-month confirmed non-persistent PIRA. The secondary outcomes were time to 6-month confirmed EDSS 6 and time to SPMS (following Lorscheider criteria). A stratified Cox regression model was used to identify the risk factors associated with non-persistent PIRA. We matched persistent PIRA patients with non-persistent PIRA patients in a 1:1 ratio (1164 patients in each group) using their propensity scores, and then compared the risk of reaching EDSS 6 using the Cox regression model. We re-matched patients with complete Kurtzke Functional Systems Scores (733 patients in each group) to compare the risk of reaching SPMS.
Results: We included 3536 RRMS patients with PIRA (mean [SD] age, 42.41 [9.77]). Use of high-efficacy disease-modifying therapies (DMT) at baseline (hazard ratio [HR], 1.37; 95% CI, 1.20-1.56; p<.0001), baseline EDSS (HR, 0.74; 0.69-0.79; p<.0001), age (HR, 0.98; 0.97-0.99, p<.0001), and disease duration (HR, 0.99; 0.98-1.00; p=.04) were associated with non-persistent PIRA. Compared with non-persistent PIRA, the HR was 6.56 (95% CI, 4.71-9.13, p<.0001) for reaching EDSS 6 and 4.46 (3.00-6.65, p<.0001) for reaching SPMS in the patients with persistent PIRA.
Conclusion: Persistent PIRA risk was higher in older patients, with longer disease duration or worse disability at baseline. Use of high-efficacy DMT during PIRA events markedly reduced the likelihood of long-term persistence. Patients with persistent PIRA were at a substantially higher risk of reaching EDSS 6 and SPMS.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.














Share this post