History
It seems like it was only yesterday when we started to debate the ethics of doing placebo-controlled phase 3 trials in multiple sclerosis (MS). The debate started shortly after interferon-beta and glatiramer acetate had been licensed as treatments for relapsing-remitting MS. The justification for continuing to do placebo-controlled trials was based on inequity, i.e. not everyone had access to a licensed treatment, and some people with MS were needle-phobic and wouldn’t agree to an injectable therapy. This rationale allowed the development of natalizumab, fingolimod, oral cladribine, dimethyl fumarate, teriflunomide and daclizumab.
However, once wider access to MS treatment and oral DMTs became available, phase 3 placebo-controlled trials gave way to an era where new therapies were compared to interferon-beta; this included alemtuzumab, ocrelizumab and ozanimod. Subsequently, when it became increasingly difficult to justify an injectable comparator, teriflunomide supplanted interferon beta as the most acceptable active comparator. Ponesimod, ofatumumab and ublituximab have all been compared to teriflunomide. More recently, the BTK inhibitor trials, which are currently running, are also using teriflunomide as the active comparator. The exception is the fenebrutinib primary progressive trial, where the active comparator is ocrelizumab (ClinicalTrials.gov Identifier: NCT04544449). The reason for the latter is that ocrelizumab is the only licensed therapy for PPMS and hence is considered the standard of care
Have we lost equipoise?
There is now a rising chorus of voices calling for teriflunomide to be replaced as the go-to comparator because (1) it is being used less often and (2) because it is perceived to be a low-efficacy DMT. Several MS experts say any phase 3 trial using teriflunomide as an active comparator should be considered unethical. Do you agree? I am not sure it is unethical, provided certain provisions are implemented to address their concerns. I also think the premise that we have lost equipoise is based on a misinterpretation of how teriflunomide works as a disease-modifying therapy.
Like many others in the UK, I was never impressed with teriflunomide as an MS DMT. Its impact on relapses and MRI activity were moderate, and the monitoring requirements were overwhelming. Until recently, patients had to have liver function tests every two weeks for the first six months. Fortunately, this requirement has changed; liver function tests are only required monthly for the first six months and then ‘regularly’ after that, for example, 6-12 monthly. There is the issue of teriflunomide being labelled teratogenic, which remains a problem. However, this would be a blanket issue for all new DMTs being tested in phase 3 trials.
I also found that people with MS (pwMS) often opt for other options when you mention the possibility of hair thinning. The hair thinning issue also occurs with other agents and is transient. Once clinicians and patients realise that teriflunomide doesn’t cause alopecia but only transient hair thinning, they seem more accepting of this potential side effect.
Over the last few years, I have changed my mind about teriflunomide. I think it is the most underrated DMT in our therapeutic armamentarium. I predict it will become one of the most used MS DMTs once its alternative mode of action becomes widely known, we understand its efficacy, and we change how we use it. There are several reasons for this.
Teriflunomide is much more effective as a DMT than we realise.
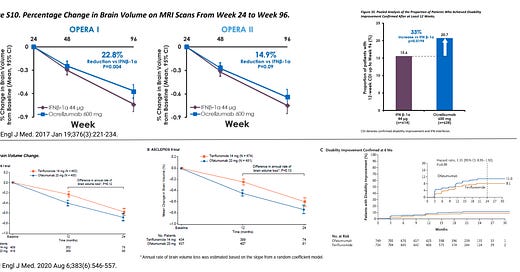
As we reinterpret, old data and new data emerge, it is clear that when we go beyond focal inflammation (relapses and MRI activity), teriflunomide is much more effective than we would expect based on its impact on relapses and MRI activity. Despite reducing relapses by, on average, a third, teriflunomide has a remarkably robust effect on disability progression and slows the accelerated brain volume loss due to MS.
The recent head-2-head studies of ofatumumab and ublituximab (anti-CD20 therapies) against teriflunomide show that despite both anti-CD20 agents being superior to teriflunomide in suppressing relapses and focal MRI activity, they were only marginally more effective than teriflunomide when it came to reduced disability worsening. Ofatumab was better than teriflunomide on disability progression, but ublituximab was not better. When assessing the more objective brain volume loss, an integrator of end-organ damage, teriflunomide, was equivalent to both these agents in slowing MS-related accelerated brain volume loss (BVL). Ofatumumab was superior to teriflunomide in reducing PIRA (EAN 2020), but again the differences are small and may not be clinically significant.
I have often highlighted that relapses and focal MRI activity are not MS and are likely to represent the immune system’s response to what is causing MS (see ‘Hot topic AAN 2023: smoldering MS’; 24-April-2023). This position is based on many observations, one of which is how teriflunomide dissociates the treatment effect on relapses and focal MRI activity from disability worsening and brain volume loss.

Teriflunomide is more effective when used as a switch agent
Another interesting observation regarding teriflunomide is that it is more effective when used second or third-line than as a first-line agent in DMT-naive patients. This observation is robust and is the only DMT to do this. What happens to the biology of MS over time that makes teriflunomide more effective? This observation is important because, in contemporary phase 3 clinical trials, more subjects are not naive to DMTs. Therefore, teriflunomide is likely more effective than anticipated from the phase 3 trial of teriflunomide.

Teriflunomide is also an outlier in terms of memory B-cells
Teriflunomide is also an outlier in terms of its impact on memory B-cells. We have made the point in the past that all of our licensed MS DMTs either reduce or stop the trafficking of memory B-cells into the CNS, except for teriflunomide. Although teriflunomide has been labelled as an immunosuppressive therapy, its profile is not immunosuppressive. In most treated patients, it doesn’t cause significant leukopaenia or lymphopaenia, it is not associated with opportunistic infections nor a secondary malignancy signal and vaccine responses are not blunted. We now know that teriflunomide has broad-spectrum antiviral activity, including against the herpes virus EBV.
Our group has recently shown that teriflunomide reduced salivary shedding of EBV in patients with MS. I have therefore hypothesised that EBV is working as an antiviral in MS. Please note this is not unique to teriflunomide but is relevant to the class of agents that are dihydroorotate dehydrogenase inhibitors (DHODHI), leflunomide, vidofludimus or ASLAN003.
DHODHIs will work best as second or third-line agents, particularly maintenance therapies after induction with a B-cell-depleting agent. Underpinning this hypothesis is to allow B-cell reconstitution to occur in the presence of an antiviral agent that targets EBV. This is the foundation of the so-called iTeri study (see ‘EBV immunotherapy for MS’; 11-Jan-2023).
Teriflunomide will become the go-to agent for de-escalating pwMS off chronic immunosuppressive therapies when they start encountering problems with infections, hypogammaglobulinaemia or poor vaccine responses. The latter is particularly an issue with older patients who are developing immunosenescence.
Teriflunomide will become low-cost
Another driver is economics. Teriflunomide is either off-patent or coming off-patent very soon in many countries. As a small molecule, teriflunomide’s price will plummet by more than 90% with the launch of generics. I have been told that generic teriflunomide is already the cheapest DMT in the USA. In countries where teriflunomide is still on-patent or not available, you can use leflunomide instead; 20 mg or 10 mg of leflunomide is metabolised into the equivalent of 14 mg or 7 mg of teriflunomide, respectively. There is not much difference between teriflunomide and leflunomide. Leflunomide is a prodrug converted into teriflunomide in the body, so if you live in a resource-poor environment and are paying for your DMTs, please ask for generic leflunomide instead. Many neurologists in resource-poor settings are reluctant to prescribe leflunomide instead of teriflunomide. They need a nudge.
Is there an alternative to using teriflunomide as an active comparator in clinical trials?
Teriflunomide is now the go-to comparator in phase 3 clinical trials of new DMTs. The rationale for this is that injectable therapies (interferon-beta and glatiramer acetate) have become unacceptable as active comparators. Firstly, it is hard to manufacture placebo injectables and almost impossible to blind trial subjects from the flu-like side effects associated with interferon-beta. Of the orals, the fumarates (dimethyl fumarate and diroximel fumarate) are not ideal as comparators because they are taken twice daily and associated with flushing and gastrointestinal side effects, which would also unblind study subjects. The S1P modulators are complicated by the logistics of doing the cardiovascular screening, first-dose monitoring for cardiac effects and the need to monitor for macular oedema using OCT (ocular coherence tomography). Selecting a higher efficacy DMTs, such as an anti-CD20 therapy or natalizumab, as the active comparator makes it very difficult to power studies based on relapse or disability outcomes; studies would need to be very large and long, which makes these trials non-viable economically. I am not aware of any MS pharma company that would compare a prospective new DMT to one of tier 3 (higher efficacy monoclonal antibodies). The licensed immune reconstitution therapies are also difficult as comparators because of their odd dosing schedules and high efficacy. This explains why teriflunomide is the current go-to comparator in contemporary clinical trials, including the BTK inhibitors and the planned anti-CD40L/frexalimab studies.
When asked for an alternative to teriflunomide, one commentator suggested dimethyl fumarate based on the assumption that DMF is superior to teriflunomide. This is also not necessarily correct. Recent real-world evidence suggests these agents have a similar impact on annualised relapse rate. I would argue that teriflunomide has superior data on disability progression and brain volume loss than DMF. So how can using DMF be more ethical than teriflunomide? As mentioned above, the S1P modulators are problematic, and the tier-3 agents are a non-starter. Does this mean we have hit the end of the road, and testing new DMTs in phase 3 trials will not be possible? One could do non-inferiority or equivalence studies, but these trials still require high numbers of study subjects and are risky from a regulatory perspective. I am unaware of any Pharma companies wanting to do a phase 3 programme based on equivalence or non-inferiority.
People with MS and the ethics committees may have a different take on this dilemma. Equipoise is about transparency and putting in place procedures to protect patients from unnecessary harm. With teriflunomide-controlled trials, you could potentially have more patients randomised to the active treatment than teriflunomide; say, a two-to-one ratio to give study volunteers a greater chance of accessing the newer and potentially more effective therapy. You could also include an escape clause so that when a study subject reaches the study end-point, i.e. sustained disability progression, they can either come out of the study or be switched to open-label treatment with the new agent. Another strategy is reducing the number of trial subjects in the teriflunomide arm by combining studies and using participants from the control arms of other trials (borrowing control subjects). This strategy is used in platform studies in oncology. Whether the regulators will accept this practice in MS is another story, but the principle underpins the design of adaptive studies with multiple arms.
We mustn’t forget that a rich-world worldview doesn’t address the reality on the ground. In many countries, many pwMS can’t afford DMTs or are uninsured. Therefore participating in clinical trials allows them access to DMTs. Being randomised to teriflunomide in a clinical trial could be considered better than not being on a DMT at all. It is well known that pwMS who participate in clinical trials do better than pwMS managed outside of clinical trials. The latter observation is probably based on patients' overall better care in clinical trials. Should we deny these people access to treatment because people in high-income countries with universal healthcare systems think randomising them to teriflunomide is unethical?
We also mustn’t forget that teriflunomide, despite being less effective in suppressing relapses and MRI activity, is almost, or as good as, anti-CD20 therapies (ofatumumab or ublituximab) when it comes to slowing disability progression and brain volume loss? Can we claim then that we are putting pwMS at greater risk of a poor outcome by randomising them to teriflunomide? Dare I suggest no? We can’t be sure that emerging new therapies, e.g. BTK inhibitors or anti-CD40L, will be better than teriflunomide. This is why we are performing randomised and blinded head-2-head comparisons.
I suggest we have a wider discussion and explore some of the options above with pwMS, organisations representing pwMS, statisticians, ethicists, ethics committees and the wider MS community before we take the moral high ground that teriflunomide comparator trials are unethical.
I need your help with a short (20-second) survey. Do you think we have lost equipoise, and that it is unethical to randomise pwMS to teriflunomide as part of a phase 3 clinical trial?
Paper
Objective: In this study, we compared the effectiveness of teriflunomide (TRF) and dimethyl fumarate (DMF) on both clinical and MRI outcomes in patients followed prospectively in the Observatoire Français de la Sclérose en Plaques.
Methods: A total of 1,770 patients with relapsing-remitting multiple sclerosis (RRMS) (713 on TRF and 1,057 on DMF) with an available baseline brain MRI were included in intention to treat. The 1- and 2-year postinitiation outcomes were relapses, increase of T2 lesions, increase in Expanded Disability Status Scale score, and reason for treatment discontinuation. Propensity scores (inverse probability weighting) and logistic regressions were estimated.
Results: The confounder-adjusted proportions of patients were similar in TRF- compared to DMF-treated patients for relapses and disability progression after 1 and 2 years. However, the adjusted proportion of patients with at least one new T2 lesion after 2 years was lower in DMF compared to TRF (60.8% vs 72.2%, odds ratio [OR] 0.60, p < 0.001). Analyses of reasons for treatment withdrawal showed that lack of effectiveness was reported for 8.5% of DMF-treated patients vs 14.5% of TRF-treated patients (OR 0.54, p < 0.001), while adverse events accounted for 16% of TRF-treated patients and 21% of DMF-treated patients after 2 years (OR 1.39, p < 0.001).
Conclusions: After 2 years of treatment, we found similar effectiveness of DMF and TRF in terms of clinical outcomes, but with better MRI-based outcomes for DMF-treated patients, resulting in a lower rate of treatment discontinuation due to lack of effectiveness.
Classification of evidence: This study provides Class III evidence that for patients with RRMS, TRF and DMF have similar clinical effectiveness after 2 years of treatment.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your own healthcare professional, who will be able to help you.
















Share this post