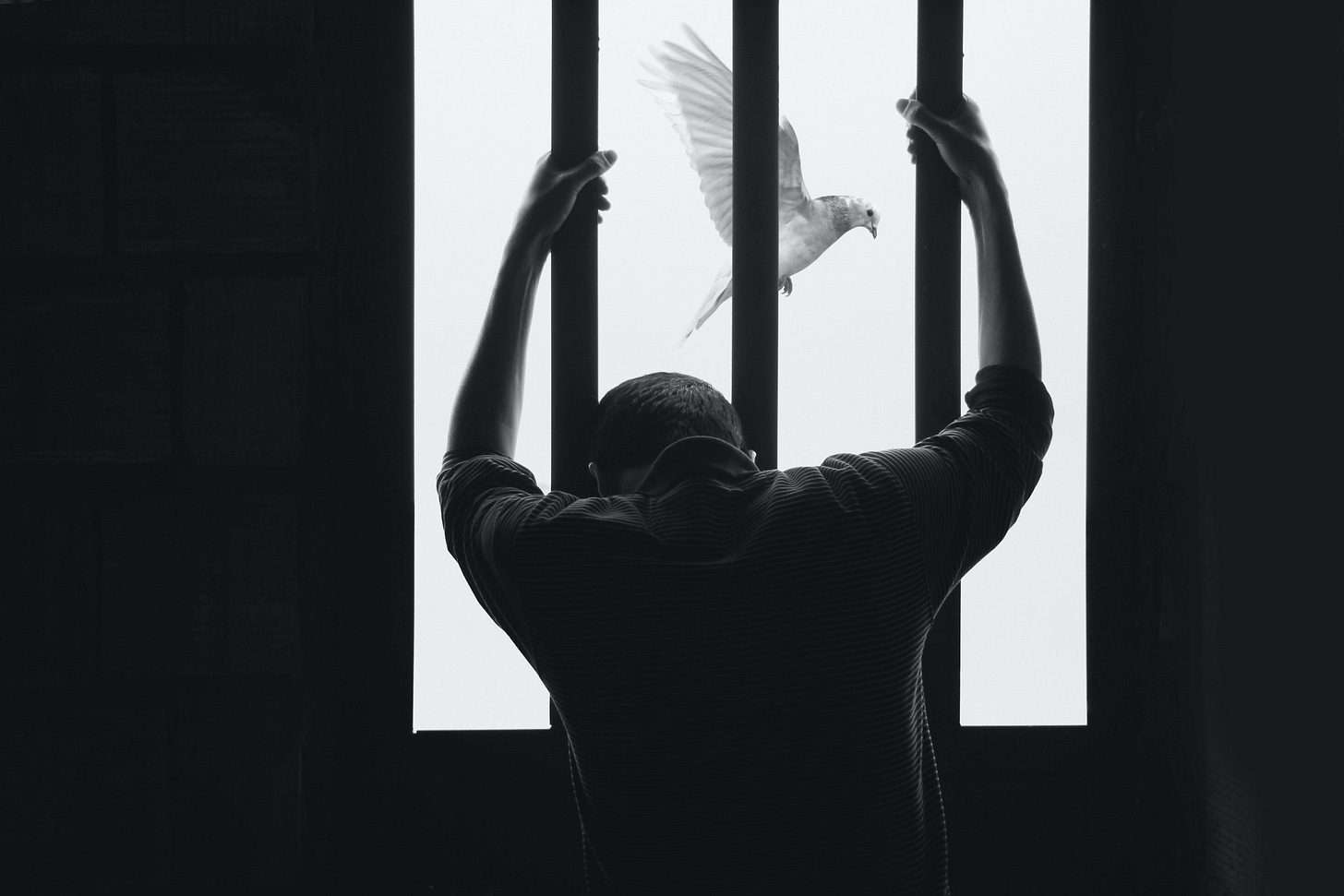
I have difficulty seeing future multiple sclerosis research (MS) outside the EBV-MS hypothesis. I have become a prisoner of my rigid thinking.
It has been clear to me for decades that EBV is the primary cause of MS. It is not the only risk factor, but it is necessary. This point is critical in that if you don’t have EBV, you can’t get MS. This underpins the primary prevention strategy of a population-based vaccine to prevent primary EBV infection, which will protect people from getting MS and other EBV-associated diseases.
However, for people who already have EBV, what can be done? This is where the science gets complex. There are two leading theories for how EBV causes MS. The first is the hit-and-run hypothesis in which EBV acting with other factors triggers autoimmunity and sets off MS; hence targeting EBV after the event will have no effect.
The other hypothesis is that EBV, via latent-lytic infection cycling, is driving MS disease activity. This could be via intermittent priming of autoimmunity or by primary CNS infection. I think the evidence for the latter is strong, which is why we are trying to pursue anti-EBV therapeutic strategies to treat MS.
PwMS have difficulty dealing with EBV. They are more likely to have had infectious mononucleosis than people in the general population. PwMS shed EBV in their saliva more commonly than healthy control subjects. Salivary shedding is a marker of lytic EBV infection. When it comes to anti-EBV immunity pwMS, have a much larger (higher levels), broader (more proteins) and deeper (more epitopes within proteins) antibody and T-cell responses to latent and lytic EBV proteins; these are often referred to as B-cell and T-cell repertoires, respectively. The repertoire data tells us that EBV is likely cycling through more rounds of latent-lytic infection, and each time this happens, it boosts the immune response to the virus that we can detect with our immunological assays.
An important question is where this latent-lytic cycling is occurring. It doesn’t appear to be in the peripheral blood. It is, therefore, likely to be in the central nervous system (CNS) or secondary lymphoid organs, particularly the deep cervical lymph nodes that are enlarged in pwMS. This is an important question because you will need CNS-penetrant antiviral therapies if it is in the CNS. If it is in the secondary lymphoid organs, peripherally acting antiviral strategies will be sufficient.
The observations show that (1) pwMS are more likely to have EBV in their brains, (2) natalizumab rebound may be driven by lytic EBV infection in the CNS and (3) anti-EBV T-cell responses are increased in people on natalizumab, despite natalizumab being an effective DMT, suggests the CNS compartment is where the action is (EBV replication). Do you agree or disagree?
Antivirals
I have argued that any antiviral strategy should ideally target both the latent and lytic cycles of EBV infection. However, this doesn’t mean that an antiviral targeting lytic infection won’t work in MS. For example, our group is investigating famciclovir as a potential treatment for MS.
Several very interesting small molecules could potentially work on both the latent and lytic EBV infection, and I am spending a lot of time trying to help some small pharmaceutical companies and nudge big pharmaceutical companies to test these compounds. In parallel, I am collaborating with one of the best medicinal chemists in the UK to develop a new class of therapeutic agents for this purpose. In parallel, I am trying to get established MS pharma companies to look at the impact their DMTs are having on EBV biology. Anti-CD20s and BTK inhibitors are anti-EBV. Are the anti-CD20 therapies and BTKi working in MS as anti-virals?
Immunotherapies
Another strategy is immunotherapies. It is known that most chronic viral infections induce a state of T-cell exhaustion or relative tolerance, which is how the viruses escape immune detection, cause disease, and from an evolutionary perspective, increase their chances of mutating and transmitting themselves to the next host. EBV is no exception. There is evidence that pwMS have a poor cytotoxic T-cell response to EBV, which explains why they have a problem dealing with EBV. This observation underpins the strategy of cellular therapy, i.e. giving either autologous or allogeneic EBV-specific T-cells as a treatment for MS. Atara Bio is currently running a phase 2 clinical trial testing this strategy. Another company called Tevogen are also hoping to test the same strategy with their propriety product in MS.
Another option is therapeutic EBV vaccines, i.e. boosting immunity to EBV in the hope it increases your antibody and T-cell responses to control the virus. This strategy has been shown to work with VZV (varicella-zoster virus) in that Shingrex, a component vaccine, boosts VZV immunity, which reduces one's risk of getting shingles (VZV reactivation). Let’s hope the vaccine companies take up the challenge of a therapeutic vaccine.
Immune reconstitution therapies (IRTs) may also work as immunotherapies against EBV. All effective IRTs deplete B-cells and purge or at least reduce, the body of pathogenic EBV. When the immune system reconstitutes itself after being depleted, it may boost its immunity, particularly T-cell immunity, to EBV, which then controls the virus and prevents it from driving MS disease activity. AHSCT, alemtuzumab, cladribine and mitoxantrone may be immunological sledgehammers that work as anti-EBV immunotherapies. Surely an EBV vaccine would be a safer and better option.
What about cancer immunotherapies for MS? I am not sure if you are aware that checkpoint inhibitors used to boost immunity to cancers make MS worse or trigger MS-like illnesses in some people. Could these immunotherapies boost anti-EBV immunity, and these T-cells then traffic to the CNS to find the CNS resident EBV-infected cells and trigger focal inflammation? A sort of IRIS (immune reconstitution inflammatory syndrome) or immune effector cell–associated neurotoxicity syndrome (ICANS), which is a common complication of CAR T-cell therapies.
A good analogy for this is PML in patients who are immunocompromised. Checkpoint inhibitors are now being used to successfully boost T-cell immunity to treat PML. If MS is due to CNS infection with EBV, we can expect immunotherapies to cause an IRIS, which will be part of the treatment. IRIS is one of the potential complications we anticipate with CD19- or EBV-targeted CAR T-cells. I have already done an MS-Selfie on the potential of CAR T-cells to treat MS (CAR T-cells as a treatment for MS, 17-Sept-2022). In the interim, we have set up a UK consortium to explore this treatment option. We have approached several companies with CAR T-cell programmes to partner with us. Fingers crossed that one comes on board.
Interestingly many of my colleagues in the field think CAR T-cells are too dangerous to treat MS. These killjoys tend to be the same people who don’t agree with using AHSCT and alemtuzumab as a treatment for MS. Do you agree with them?
Bispecific antibodies
Can we make T-cell immunotherapy safer? Another strategy is using bispecific antibodies to stimulate T-cells adjacent to potentially pathogenic, EBV-infected B-cells, which will then kill them. One such bispecific antibody is glofitamab. Glofitamab targets CD20 (B-cells) and CD3 (T-cells), which redirects T cells to eliminate B cells. The study below, recently published in the New England Journal of Medicine, shows this strategy is effective in refractory B-cell lymphomas. However, hidden in the paper's small print is a potential Achilles heel of this antibody. The so-called immune effector cell–associated neurotoxicity syndrome (ICANS) due to CNS inflammation was uncommon with glofitamab and mostly mild (grade ≥3 events in only 3% of the patients). In contrast with CAR T-cell therapies, ICANS of grade 3 or higher have been reported to be above 10% and as high as 32%. This means glofitamab is not getting into the CNS, whereas CAR T-cells are. Despite my reservations, it would be worth testing glofitamab in MS to purge the peripheral compartment of EBV-infected B-cells.
I would love an induction-maintenance trial with glofitamab in MS. Induction to purge EBV from the peripheral compartment and then to a maintenance phase with a safe and well-tolerated antiviral to prevent EBV reinfection, i.e. to allow B-cell reconstitution in the absence of EBV. Sort of an iTeri trial that I have discussed in the past (teriflunomide is anti-EBV). The problem with the latter study is the primary outcome and showing regulators that this treatment strategy works. Do you have any ideas?
If any Roche employees in the MS drug development group read my newsletters, are any of you interested in this approach?
Background: The prognosis for patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) is poor. Glofitamab is a bispecific antibody that recruits T cells to tumor cells.
Methods: In the phase 2 part of a phase 1-2 study, we enrolled patients with relapsed or refractory DLBCL who had received at least two lines of therapy previously. Patients received pretreatment with obinutuzumab to mitigate cytokine release syndrome, followed by fixed-duration glofitamab monotherapy (12 cycles total). The primary end point was complete response according to assessment by an independent review committee. Key secondary end points included duration of response, survival, and safety.
Results: Of the 155 patients who were enrolled, 154 received at least one dose of any study treatment (obinutuzumab or glofitamab). At a median follow-up of 12.6 months, 39% (95% confidence interval [CI], 32 to 48) of the patients had a complete response according to independent review. Results were consistent among the 52 patients who had previously received chimeric antigen receptor T-cell therapy (35% of whom had a complete response). The median time to a complete response was 42 days (95% CI, 42 to 44). The majority (78%) of complete responses were ongoing at 12 months. The 12-month progression-free survival was 37% (95% CI, 28 to 46). Discontinuation of glofitamab due to adverse events occurred in 9% of the patients. The most common adverse event was cytokine release syndrome (in 63% of the patients). Adverse events of grade 3 or higher occurred in 62% of the patients, with grade 3 or higher cytokine release syndrome in 4% and grade 3 or higher neurologic events in 3%.
Conclusions: Glofitamab therapy was effective for DLBCL. More than half the patients had an adverse event of grade 3 or 4. (Funded by F. Hoffmann-La Roche; ClinicalTrials.gov number, NCT03075696.).
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.
















Share this post