Case study
I saw a 56-year-old male with primary progressive MS several years ago. He had been diagnosed about three years earlier and had gone from a mild limp to needing a walking stick in just over three years. When I examined him, I noticed he had halitosis due to poor oral hygiene and severe periodontal disease. He was a heavy smoker, common in people with periodontal disease. I referred him to the dentist. Unfortunately, his periodontitis was so severe he had to have all his teeth extracted and was fitted with dentures. After having his teeth extracted, he noticed an improvement in his general health. He also felt that his MS stabilised, i.e. didn’t notice any further deterioration in his physical function over the next two years. He subsequently moved to another part of the country, and I didn’t see him again, so I am unsure if he developed ‘burnt-out MS’.
Prof G’s opinion
In general chronic and recurrent infections make MS worse. The infection stimulates inflammatory mediators called cytokines that result in sickness behaviour and stimulate innate immune reactions within the central nervous system that may speed up smouldering inflammation. The latter is part of the hot microglial hypothesis of smouldering MS. We know from work done on animal models that systemic inflammation induced artificially with bacterial endotoxin (LPS or lipopolysaccharide) makes animals with neurodegenerative diseases much worse. They often don’t return to their baseline because of the effects of innate immune activation in the central nervous system. I am sure many of you have had a severe bacterial or viral infection that causes a recrudescence of old symptoms that takes you weeks or months to recover from, and in some instances, you don’t get back to baseline. I have a few patients that this happened to with severe COVID-19.
This patient had rapidly worsening PPMS that seemed to stabilise once his periodontitis or gum infection was treated. Is this patient a one-off? I am not sure, but he changed my behaviour. I now actively recommend patients see a dentist when I detect periodontal disease, which is more common in pwMS than in the general public (see paper below).
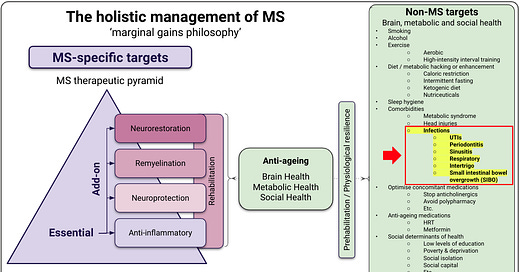
In my holistic management of MS infographic, you will see periodontitis on the list of infections to look out for. The association between MS and periodontitis has been known for some time. The other infections on the list include urinary tract (UTIs), respiratory, intertrigo, ingrown toenails and sinusitis. I have recently added small intestinal bacterial overgrowth (SIBO).
UTIs relate to neurogenic bladder dysfunction that is very common in pwMS (please see ‘Infection’, 29-June-2021). Respiratory infections are also commoner and relate to swallowing problems, resulting in aspiration and aspiration pneumonia. SIBO is related to chronic constipation, which has been reported to occur in around half of people studied with MS. Recurrent and chronic sinusitis also seems more common in pwMS and has been causally associated with MS; i.e., people with sinusitis are more likely to get MS in the future.
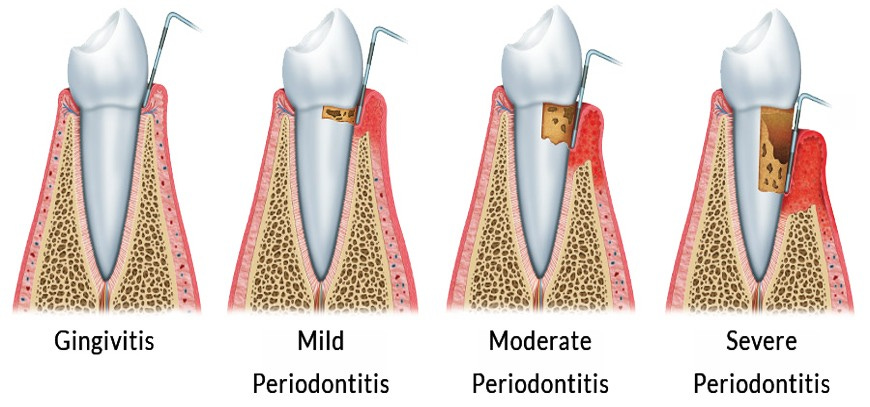
Periodontitis or gum disease
Chronic periodontitis is a common gum disease affecting the teeth' surrounding tissues. It is characterised by inflammation and destruction of the supporting structures of the teeth, including the gums, periodontal ligament, and alveolar bone. If left untreated, chronic periodontitis results in tooth loss.
Several factors contribute to the development and progression of chronic periodontitis. The most significant risk factor is poor oral hygiene. Inadequate brushing and flossing allow plaque and tartar to accumulate on the teeth, leading to bacterial growth and infection. Smoking is a major risk factor for developing chronic periodontitis.
Having comorbidities, such as diabetes, also increases your risk of developing chronic periodontitis. Hormonal changes, such as those occurring during pregnancy or menopause, make gums more susceptible to inflammation and infection.
Genetics play a role in chronic periodontitis as well. Some individuals may be more genetically predisposed to developing gum disease than others. Additionally, age is a risk factor, as the likelihood of developing periodontitis increases with age. Other factors contributing to chronic periodontitis include immunosuppression, stress, poor nutrition, some medications, and teeth grinding or clenching. Antacids, anticholinergics, antihistamines, antidepressants, calcium channel blockers, decongestants, phenytoin, cyclosporin and other immunosuppressive therapies and analgesics are associated with gum disease.
As a person with MS, it is important to be aware of these risk factors and take appropriate measures to prevent or manage chronic periodontitis. Practising good oral hygiene, quitting smoking, managing your underlying medical conditions, and regularly visiting a dentist and oral hygienist for professional cleanings and check-ups can help reduce the risk of developing this destructive gum disease. I know this is easier said than done in the UK because of the current crisis with NHS dental services, but there is a lot you can do yourself.
Many of my patients are unaware that they have gum disease because they assume the state of their mouth and gums is normal. The following is a list of symptoms and signs of periodontitis to look out for:
Gums that are red, swollen, tender, and/or bleeding
Painful or uncomfortable chewing
Teeth sensitivity
Loose teeth
Chronic bad breath
Receding gums
I know the cynics will say, ‘Oh no, not another thing to worry about’ gum disease. Everybody should worry about gum disease, which is linked to poor health outcomes, particularly cardiovascular disease and reduced life expectancy. Many argue that periodontitis should be considered one of the social determinants of health. Why would we ignore periodontal disease if we are going to adopt a marginal gains approach to managing MS?
“The whole principle came from the idea that if you broke down everything you could think of that goes into riding a bike, and then improved it by 1%, you will get a significant increase when you put them all together.”
Sir David Brailsford (Brailsford 2015).
"If we break down everything we can think of that goes into improving MS outcomes and then improving it by 1%, we will get a significant improvement when we put them all together.”
Prof G, MS-Selfie, 2022
I would be interested to hear if any of you have been diagnosed with periodontal disease and whether or not you have noticed any link with the worsening of your MS symptoms.
Paper
Background: Chronic periodontitis (CP) is a multifactorial, chronic inflammatory disease of microbial etiology that manifests as a result of the dysfunction of the immune mechanism, culminating in the destruction of the alveolar bone of the jaws. Multiple sclerosis (MS) is an autoimmune disorder that affects the central nervous system (CNS), leads to demyelination and degeneration of nerve axons and often causes severe physical and/or cognitive impairment. As CP and MS involve inflammatory mechanisms and immune dysfunction, researchers have attempted to study the association between them.
Aim: To systematically review the literature on the epidemiological association between CP and MS in adults.
Methods: PRISMA 2020 statement was used in the study protocol. The design was done according to the Cochrane methodology. A comprehensive literature search was performed in PubMed, Scopus and Cochrane databases; a manual search and evaluation of the gray literature was also performed. The meta-analysis was performed by Review Manager (RevMan) 5.4. Odds ratio (OR) with 95% confidence interval (CI) was defined as the effect size of the outcome. Heterogeneity was assessed by Chi-square and I2. The articles evaluated were written in English, without a time limit, concern observational studies (patient-controls) and report the diagnostic criteria of the diseases. Duplicate entries were excluded. To evaluate the reliability of the results of each study, Newcastle-Ottawa Scale (NOS) and GRADE tools were used. Two independent reviewers did all evaluations with a resolution of discrepancies by a third.
Results: Meta-analysis included three observation studies examined 3376 people. MS patients are significantly more likely to be diagnosed with CP than healthy controls (OR 1.93, 95% CI 1.54-2.42, p<0.0001).
Conclusion: A high prevalence of CP was found among MS patients compared with healthy controls. Healthcare professionals should be aware of the association between these pathological entities to provide patients with high-quality care through an effective and holistic diagnostic and therapeutic approach.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your own healthcare professional, who will be able to help you.














Share this post