Case study
I need your advice about CIN (cervical intraepithelial neoplasia) and ocrelizumab. I am in a tough situation, and I have been given different opinions from various specialists and I am confused about what to do.

Unfortunately, I have an active HPV infection (type 52 and 6) on PCR. Fortunately, my cervical smear tests are all clear. Since reading your article I've been considering getting the Gardasil-9 vaccine before starting ocrelizumab. However, I am not sure I can delay ocrelizumab treatment as I have highly active MS with a poor prognostic profile. My baseline MRI in early 2020 has over 30 visible lesions and I have spinal cord lesions as well. Despite having started on pegylated interferon-beta, which was subsequently changed to teriflunomide, my lesion load has increased. Since starting teriflunomide I have acquired a further four new lesions and my EDSS has increased from 2.0 to 4.0. Apparently, my lesion load is now over 50 lesions.
My neurologist has excluded natalizumab as a treatment because I have a high JCV index of 3.1. Ocrelizumab has been recommended and I have had the necessary vaccinations, i.e. VZV, pneumococcal and COVID-19. It wasn’t until I read your MS-Selfie Newsletter about HPV did I pause my ocrelizumab start date to get myself screened for HPV.
I am worried about delaying starting ocrelizumab for 7 months to have the three doses of Gardasil-9 (month 0, month 2 and month 6). What should I do?
Prof G’s Recommendation(s)
In an earlier email response, I recommended that she should consider oral cladribine instead of ocrelizumab. This will allow her to have the first two doses of the Gardasil-9 vaccine, start cladribine and then have the 3rd or booster dose between months 6 and 12 after starting cladribine. The reason for giving this advice is that vaccine responses are likely to be maintained with cladribine compared to ocrelizumab (anti-CD20), which blunts or prevents B-cell or antibody responses. The latter advice is based on the recent COVID-19 vaccine data being extrapolated to the HPV vaccine.
When this patient asked her neurologist if she could be treated with cladribine he said he wouldn’t be able to prescribe cladribine because of his concerns about the associated cancer risk. He didn’t want to take responsibility for prescribing it in case she develops cancer in the future and ‘blames him’.
Does cladribine cause cancer?
When we completed the phase 3 CLARITY trial (two-doses of oral cladribine vs. placebo in relapsing-forms of MS) there was an imbalance in cancers, which resulted in an obvious cancer signal. In the two treatment arms, there were 4 subjects who developed cancers, compared to no cancers in the placebo arm, i.e. a two to zero ratio (Giovannoni et al. N Engl J Med. 2010 Feb 4;362(5):416-26.). When you have zero in the denominator there will always be a signal. This is why the regulators include cancer as a risk in the Mavenclad label and why it is part of a black-box warning in the USA. Regulators respond to data and that is what the data says.
However, over time new data has emerged to suggest the risk is not an obvious signal, at least in the short- to intermediate-term.
Types of cancer
The types of cancers we saw in the CLARITY trial are not the types of cancers associated with immunosuppression. There was a case each of breast cancer, pancreatic cancer, melanoma and choriocarcinoma of the uterus. Apart from the choriocarcinoma, which is derived from the placenta and is pregnancy-related cancer, the other three cancers probably take years to evolve and are likely to have been developing prior to cladribine exposure. The typical cancers you see with immunosuppression are basal and squamous cell cancers of the skin and lymphomas. We haven’t seen excess numbers of these types of cancers in cladribine-treated patients, which is very reassuring.
Cancer rates
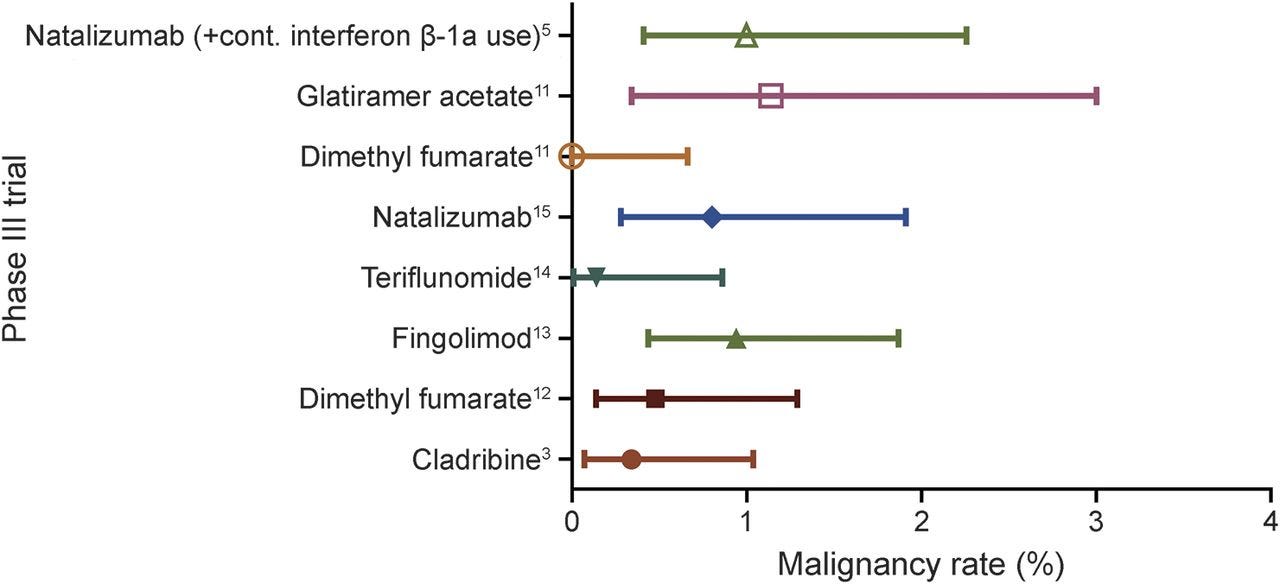
When my colleagues then looked at the cancer rate in cladribine-treated subjects in the trial they found it to be very similar to the cancer rates associated with other MS disease-modifying therapies (Pakpoor et al. Neurol Neuroimmunol Neuroinflamm. 2015 Oct 1;2(6):e158.).
The cancer rate, however, was abnormally low in the placebo-arm of the CLARITY trial and I, therefore, think the reason why there is an apparent cancer signal is that it is been driven by the low rate in the comparator or placebo arm and not a high rate in the treatment arm. In fact, if we had just one cancer in the placebo arm of the trial the cancer signal would not have been there.
Another clue is when we followed up the placebo-treated patients after the phase 3 trials they had a higher rate in the subsequent years compared to the patients in the active treatment arms who were exposed to cladribine. This suggests the placebo-treated subjects just didn’t develop their cancers in the trial but did so afterwards; this is a type of lag-time bias and can happen by chance.
We then compared the cancer rate in the cladribine-treated patients to what is expected in the general population. To do this is you compare the rates in cladribine-exposed patients to the cancer rate in the global cancer registry. When you do this you get a standardised incidence rate or SIR that is very close to one, i.e. the expected cancer rate. Over time the SIR jas remained close to one (no increased risk), but more importantly, the confidence intervals around this value have become very small or narrow. This makes it likely that there is no cancer signal associated with cladribine treatment.
Is cladribine a mutagen?
Contrary to what many people think cladribine is not a mutagen. Although it works through DNA mechanisms, by triggering apoptosis or cell death, it does not cause mutations in DNA. The correct term for a drug like this is a clastogen. I suspect the legacy of cladribine has been determined by the fact that it has been repurposed from oncology, therefore, it is assumed by inference to be a mutagen and that it must damage DNA and work as a cytotoxic therapy. In reality, cladribine’s mode of action is very nuanced and is not cytotoxic.
Cladribine is actually an inactive compound and has to be transported into a cell. Cladribine is only activated in cells that express an enzyme that phosphorylates it (i.e. add phosphate groups to the drug). The only cells that express this enzyme (DCK or deoxycytidine kinase) at high levels are lymphocytes, in particular B-cells. When cladribine is activated it inhibits enzymes that extend DNA chains. When the cells detect that DNA chains can’t be extended the cell triggers the so-called cell death programme and the cell commits suicide or dies by a process of apoptosis. With apoptosis, the cell is not lysed and therefore it does not release its contents, which is why you don’t get a cell lysis syndrome with cladribine and therefore there is no need to be pre-dosed with steroids or to take antihistamines prior to being treated with cladribine. The latter avoids the side effects, such as psychosis, diabetes, hypertension and avascular necrosis of the hip, that has been seen with high-dose steroids that need to be given prior to infusion of some DMTs to prevent infusion reactions.
Another clue to the cladribine cancer signal being a false-positive comes from the oncology registers of patients who have received cladribine and related drugs for hairy cell and chronic lymphoid leukaemia. In this register, there was no increased cancer signal despite these patients being much older than people with MS treated with cladribine (Cheson et al. J Clin Oncol. 1999 Aug;17(8):2454-60.).
Summary
We now have close to half a million patient-years of follow-up of cladribine-exposed patients and there is no apparent increased rate of cancer. Some of the cladribine-exposed patients have been followed for over 10 years. So based on all these factors and an increasing amount of safety data I think the risk of cancer from cladribine treatment is low and unlikely to be above what is expected in the general population.
You have to be aware that ‘shit happens’ and some pwMS will develop cancer, whether or not they are treated with cladribine. So yes there will be people treated with cladribine who develop cancer, but on balance, these cancers are unlikely to be related to cladribine treatment itself.
So based on the above this patient should go back to her neurologist and try to explain the above. If he still says no she may want to consider other options.
Other options for this patient
What about starting on natalizumab and staying on it for 6 -12 months during which you have the Gardasil-9 vaccine and then transition to ocrelizumab once you are immune to HPV? The PML risk associated with natalizumab therapy only goes up after about 12 months of exposure.
Another option is to have the first two doses of Gardasil-9, wait 3-4 weeks to ensure a good vaccine response, and then start ocrelizumab. You can then time your Gardasil-9 booster, or the third dose, to be towards the end of the first year, i.e. 4 weeks before your next ocrelizumab infusion. Please note booster responses are not necessarily blocked by anti-CD20 therapies as these don’t require so-called germinal centre or GC responses. GC responses are however essential for neoantigen or new antibody responses. Another factor is T-cell responses these should be boosted by the vaccine even though you may still be B-cell depleted from the initial two courses of ocrelizumab. In terms of HPV immunity, it is likely that the T-cell responses are more important than antibody responses.
Conclusion
This case study illustrates how important vaccine responses have become in terms of DMT choice and is a good example of the complexities associated with DMT use in clinical practice. I hope this case study helps explain this.
Can I please remind you that the person taking the risk associated with specific treatments is the patient and not the neurologist or HCP? If this patient is prepared to take on the risks of an immune reconstitution therapy such as oral cladribine then should the neurologist really be preventing her or blocking her access to this treatment?
Subscriptions
As you are aware I am raising funds from paid subscriptions to administer the MS-Selfie Newsletter and associated MS-Selfie microsite that is currently in development. So if you are an active paying subscriber thank you, your contribution is much appreciated.
I originally charged a subscription for case studies such as this and made all the other MS-Selfie newsletters free. I subsequently changed the funding model of MS-Selfie and made all content free. However, since doing this I have had a large number of subscribers cancel their subscriptions, which is now threatening the financial viability of MS-Selfie. If this trend continues, which I hope it will not, I will have to reintroduce a two-tiered system with the case studies being restricted to paying subscribers only.
Please note the money raised via subscriptions is being used to pay a professional medical writer to curate, rewrite and transfer the contents of the Newsletter onto a companion MS-Selfie microsite, which is being designed and maintained by a freelance web designer.
So if you find these Newsletters helpful and want the wider MS community to continue to have access to all content I would encourage you to become a paid subscriber. Thank you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.
















Share this post