Case study: cervical intraepithelial neoplasia (CIN) and ocrelizumab
There are theoretical reasons why people on anti-CD20 therapies may be at increased risk of developing cancers such as cervical cancer. This has implications for vaccination.
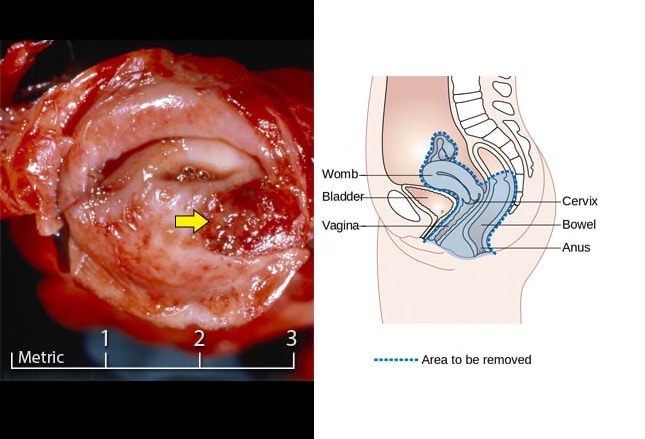
Case study
What would you suggest to a person on ocrelizumab who 10 years previously had CIN 3 (cervical intraepithelial neoplasia grade 3) and was told the only thing stopping it from being cancer was a layer of skin. I had a colposcopy and treatment to remove the abnormal cells. My smears were clear until I started on ocrelizumab and now my last two smears have come back showing a risky strain of HPV (no new sexual partner). Is it likely that the HPV has reactivated because of the immunosuppression from ocrelizumab? I’m over the age where they would have offered me a vaccination. My worry is that they are leaving it another year (which will be 3) and not taking into account that I am on immunosuppressive therapy.

Prof G’s opinion
The current immunological dogma states that anti-viral immunity against the various strains of HPV (human papillomavirus) is predominantly T-cell mediated, in particular, CD8+ cytotoxic T-cells and not via B-cells. However, the presentation of antigen to the immune system, in particularly oncogenic antigens (those antigens linked to cancers) may require B-cell function. Therefore there are theoretical reasons why people on anti-CD20 therapies may be at increased risk of developing cancers.
I am not aware of any data linking ocrelizumab treatment with HPV infection. However, there is some published data that indicates that women on rituximab are at increased risk of being HPV positive. What this is saying is that antibody immunity against HPV may be important in preventing you from becoming infected with HPV or developing a symptomatic or overt HPV infection. This would be compatible with recent insights in relation to COVID-19 and anti-CD20 therapies, i.e. that blunted pre-existing and induced anti-viral antibody responses to coronaviruses put you at increased risk of getting symptomatic COVID-19 and more severe COVID-19.
Will coming off ocrelizumab help you mount, or at least boost, an antibody response to the HPV strain causing your cervical infection? Yes, I suspect so and this would be in my opinion a reason for you to switch treatments. I would suggest de-escalating from ocrelizumab to interferon-beta or teriflunomide, i.e. two classes of DMTs that have been shown to have antiviral effects.
Once off ocrelizumab and you have some peripheral B-cell reconstitution I would recommend being vaccinated with the polyvalent HPV vaccine (Gardasil-9). There is data showing that women with CIN can still benefit from the HPV vaccine, i.e. it will not only boost your immunity against the current strain you are infected with, but it will give you immunity against the strains your immune system has not seen yet.
I note that in many countries the HPV vaccine is not covered by healthcare systems in people who are out of the age range. However, I have examples where when you approach your insurance company for a specific reason they agree to cover the costs of the vaccination.
Other issues around HPV vaccination
Please note that the polyvalent HPV vaccine (Gardasil-9) cuts cervical cancer rates by close to 90% (Falcaro et al. Lancet 2021:November 03). This stunning data doesn’t address the other benefits of preventing HPV infection, which include preventing penile, anal, nasopharyngeal and oesophageal cancers not to mention simple cutaneous warts.
So what to advise pwMS about the HPV vaccine?
The HPV vaccine prevents infection with the sexually transmitted human papillomavirus (HPV) which is known to cause cervical cancer and several other cancers. Therefore, if you have MS are about to decide to go onto an immunosuppressive therapy, in particular, potent immunosuppressive therapies. The suppression of your immune system may allow viruses to escape and start replicating. This is a particular problem with alemtuzumab, HSCT and the S1P modulators (fingolimod, siponimod, ozanimod, ponesimod). In relation to HPV infection, the jury is out regarding anti-CD20 therapies, however, once you start an anti-CD20 therapy your ability to mount a good vaccine response is blunted. So there is a strong augment to get yourself vaccinated, or to upgrade your immunity from the quadrivalent to the polyvalent vaccine, before starting immunosuppressive therapy.
HPV is not only a problem for women. HPV is a well-established cause of penile and anal cancer and causes a small proportion of throat and oesophageal cancers. Therefore it makes sense for males to be vaccinated against HPV as well.
The epidemiology of HPV infection is also changing. People are becoming infected later in life and are spreading the virus. Social media and dating apps have revolutionised the dating world and many older people are becoming promiscuous and are having unsafe sex later in life. As a result of this, there has been a large increase in the incidence of sexually transmitted diseases in older people, including HPV infections. This has prompted some commentators to suggest that public health officials extend the HPV vaccine to all women and possibly all men. Why wouldn’t you want to reduce your risk of getting cervical cancer? Isn’t prevention better than having to treat HPV infection and its downstream effects, i.e. premalignant cervical lesions or cervical cancer?
Question 1: If I have been vaccinated with the older quadrivalent vaccine could I receive the new vaccine to cover the other strains of the virus?
Yes, there is data that shows that the previous vaccination against HPV doesn’t stop your immune system from responding to the vaccine components that cover the new strains.
Question 2: As I am on a DMT can I have the HPV vaccine?
This all depends on the DMT you are on. For the non-immunosuppressive immunomodulators such as interferon-beta, glatiramer acetate and teriflunomide vaccination is unlikely to be a problem. Similarly for the fumarates, natalizumab, cladribine and alemtuzumab the level of immunosuppression and the window of vaccination are unlikely to affect vaccine responses. However, based on the COVID-19 vaccine studies if you are on an S1P modulator (fingolimod, siponimod, ozanimod or ponesimod) or an anti-CD20 (ocrelizumab, ofatumumab, rituximab) the response to the HPV vaccine is likely to be blunted.
Question 3: I need to start a DMT, but I want to have the HPV vaccine or extend my cover with the new polyvalent vaccine, how long will I need to wait before I can start treatment?
The polyvalent vaccine at the moment requires 2 or 3 doses with the last dose given at 5 or 6 months. Ideally, to give your immune system a chance to respond to the vaccine you will need to wait until 4 weeks after the final booster, i.e. 6 or 7 months.
Question 4: Should I delay starting DMTs to have the vaccine?
There is no simple answer to this question. You have to balance the risks and benefits of having the vaccine against the risks of untreated MS. In relation to the IRTs, I would suggest going ahead and starting the IRT and delaying the vaccine until you have reconstituted your immune system. Delaying starting an IRT to have the vaccine does not make immunological sense in that the memory responses you have just made to the vaccine could potentially get depleted and depending on the intensity of the immunodepletion may not recover your immunity. For maintenance DMTs, in particular, the S1P modulators and anti-CD20 therapies you should probably delay starting treatment to have the vaccine. I am not sure a 7-month wait to have all three vaccine doses is justified. A better compromise would be to have the initial two doses and then take a chance with the third booster dose towards the end of year one and as far away from your last dose of anti-CD20 as possible. To answer this question I would urge the pharmaceutical companies to do HPV vaccine studies with their DMTs.
Question 5: If I want the new polyvalent vaccine will the NHS cover it?
At present, the answer is no. The UK is in the process of switching from the quadrivalent (Gardasil-4) to the polyvalent vaccine (Gardasil-9) under the national vaccine programme. At present, if you want to be vaccinated against HPV you will have to cover the costs of the vaccine yourself. This is not too dissimilar to what happens with travel vaccines.
I predict that HPV vaccination is going to be one of those factors that have to be put in the mix when deciding which is the correct DMT for you. It is not a major factor but is an important factor nevertheless. I have only just started to routinely discuss this topic with my patients. It clearly has future health implications.
What is your view on this? Do you think MS healthcare professionals should be obliged to discuss issues around HPV vaccination before pwMS start a DMT?
Subscriptions
Thank you for subscribing to this Newsletter. The subscriptions will make MS-Selfie more functional. However, if you are reading this case study and are not a paid-up subscriber, but you can afford to subscribe, I would encourage you to consider doing so. Subscriptions will help me and the MS community in general. Please note if you can’t afford to subscribe and have MS and want access to all the case studies please drop me an email and I will give you a complimentary subscription.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.





Re. the case study, some questions-
1. How long should she wait once off of ocrelizumab & starting on teriflunomide / interferon before taking the first dose of the vaccine ?
2. Can she change back to ocrelizumab 4 weeks after receiving the third dose of the vaccine?
Really interesting to hear about this case study. Having had HPV infection and smear abnormalities in the past (CIN 1) and had recurrence with associated diathermy treatments I have luckily had clear smear tests (including a recent test showing no HPV) for a number of years. However my husband was diagnosed and successfully treated for intra-epithial penile neoplasia a while ago, suggesting that any HPV infection I might have had may be of one of the higher risk types of HPV.
However, I am now on Tysabri, but at no stage during choice of treatment options was the potential for activation of HPV discussed as a risk factor. As I might have to consider a change to another immune-suppressive DMT at some point then being aware of potential impact of previous HPV infection is worth knowing and I would certainly consider getting a polyvalent vaccine if I could.