Case study
I have had MS for 18 years and I am now quite disabled. I am very unsteady on my feet with frequent falls. I now have to use a walker or Zimmer frame to try and prevent myself from falling backwards. Unfortunately, I fractured my left humerus last year as a result of a fall. Since then my mobility has deteriorated further. I also have tremors in both hands that prevent me from drinking out of a glass or cup and I now have to use a double-handled closed mug with a straw. I also need help with eating and getting dressed in the morning. One of my biggest problems is nystagmus and poor vision due to my eyes jumping around. This is particularly problematic when I watch TV or try to use my computer or phone. Is there anything that can be done to help my vision?
Please note this case has simply been chosen to illustrate an extreme case of nystagmus and associated oscillopsia; however, saying this MS can cause severe nystagmus.
Prof G’s reply
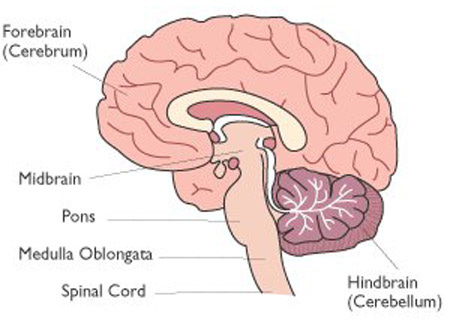
You appear to have cerebellar dysfunction with nystagmus. The cerebellum is a small structure at the back of your brain that is responsible for coordination. I have done a separate Newsletter on the cerebellum and brainstem (Has MS affected your brainstem and cerebellum? 01-Oct-2021).
The following is a list of some of the symptoms that can be associated with cerebellar involvement in MS:
Double vision
Oscillopsia (jumping images)
Jerky eye movements
Unsteady gait or ataxia
Incoordination
Tremor
Vertigo
Slurred speech
Swallowing problems
Choking
Falls
Cognitive impairment (in particular sequencing memories)
Sadly we have no licensed treatments for cerebellar dysfunction and most of our care is supportive.
Oscillopsia is a difficult one. Most patients with oscillopsia find a neutral position when the visual impairment is minimised; this may involve rotating and/or tilting the head to find a position that gets rid of, or minimises, the oscillopsia. Alternate eye patching and using one eye at a time to watch TV, read or use a computer can help. For devices one option is to use a large screen with large font size and to use the high-contrast visual mode. Magnifying glasses are helpful for reading printed text. There are also text-to-voice devices that can be used.
If oscillopsia is a problem I refer patients to a low-vision aid clinic, which is run by ophthalmologists. Sometimes patients come back from this clinic with prisms on their glasses. Prisms typically work when there is a problem with an eye movement in a particular direction, for example, weakness of a muscle pulling one of the eyes outwards or inwards. The prism bends light by a small amount from one eye and this is sufficient to correct the double vision enough so that it is not noticeable.
Occasionally using baclofen in combination with gabapentin can suppress oscillopsia. The problem with this particular combination is that patients often find it too sedating. I have had some patients reporting that their MS-associated oscillopsia responds to medical cannabis. Outside of spasticity or pain, where I think the evidence base for medicinal cannabis, Sativex, THC and nabilone is reasonable, I would not recommend cannabis or its derivatives for this indication.
More recently there have been an increasing number of reports of memantine, a drug that is used in patients with Alzheimer’s disease to improve cognition has been shown to help with oscillopsia. I have tried memantine in a handful of patients and it helped about half of the patients. It is probably worth trying memantine before the baclofen-gabapentin combination as memantine is not associated with sedation.
So there is potentially a lot we can do for this patient. In addition, this patient would need to have a bone density scan to make sure they don’t have osteopenia or osteoporosis. We also have medication to strengthen bones to reduce the risk of fractures from any future falls. I sincerely hope this patient is seeing a physiotherapist and has been enrolled in a falls prevention programme. The physiotherapist and occupational therapy team may also be able to advise this patient on other strategies to reduce her tremor (wrist weights) and other devices and gadgets to help her deal with her disabilities and handicaps.
Please let us know if any of you have oscillopsia and if you have found anything else that works for you.
BACKGROUND: Acquired pendular nystagmus (APN) is a back and forth, oscillatory eye movement in which the 2 oppositely directed slow phases have similar waveforms. APN occurs commonly in multiple sclerosis and causes a disabling oscillopsia that impairs vision. Previous studies have proven that symptomatic therapy with gabapentin or memantine can reduce the nystagmus amplitude or frequency. However, the effect of these medications on visual acuity (VA) is less known and to our knowledge the impact of non-pharmacological strategies such as blinking on VA has not been reported. This is a single observational study without controls (Class IV) and is meant to suggest a future strategy for study of vision in patients with disabling nystagmus and impaired vision.
CASE REPORT: A 49-year-old woman with primary progressive multiple sclerosis with spastic paraparesis and a history of optic atrophy presented with asymmetrical binocular APN and bothersome oscillopsia. We found that in the eye with greater APN her visual acuity improved by 1 line (from 0.063 to 0.08 decimals) immediately after blinking. During treatment with memantine, her VA without blinking increased by 2 lines, from 0.063 to 0.12, but improved even more (from 0.12 to 0.16) after blinking. In the contralateral eye with a barely visible nystagmus, VA was reduced by 1 line briefly (~500 ms) after blinking.
CONCLUSIONS: In a patient with APN, blinking transiently improved vision. The combination of pharmacological treatment with memantine and the blinking strategy may induce better VA and less oscillopsia than either alone.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite that is currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry or Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.













Share this post