Has MS affected your brainstem and cerebellum?
People with MS who have lesions in the posterior fossa have a poorer prognosis. However, there are things that can be done for each of the problems that arise from posterior fossa involvement.
Do you know if you have any lesions in the part of the brain that is found in the posterior fossa of the skull? This area includes the part of the brain called the brainstem and cerebellum.

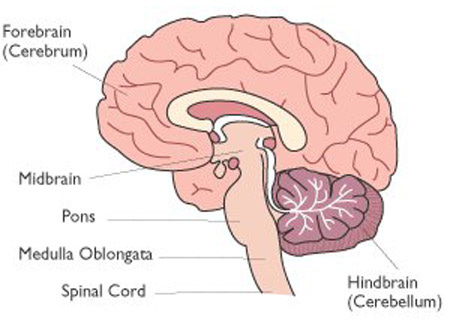
The brainstem is the part of the central nervous system (CNS) between the spinal cord and the so-called cerebral hemispheres. The brainstem consists of three parts the medulla oblongata, pons and midbrain. The brainstem is like a very busy railway junction with many fibre tracts (axons) passing through it on the way to the spinal cord (cerebrospinal) and back from the spinal cord to the brain (spinocerebral). In addition, the brainstem houses many of the so-called autonomic centres that control breathing, blood pressure, pulse rate and swallowing. The brain stem also houses the centres for eye movements, hearing, balance, coordination, walking and the nerve cell bodies of most of the cranial nerves.
The brainstem is also closely linked to the cerebellum or mini-brain that controls many motor functions. The brainstem and cerebellum are housed in the posterior fossa of the skull. When MS lesions occur in the posterior fossa, i.e. brainstem and cerebellum, they are frequently symptomatic and can be very devastating. People with MS (pwMS) with posterior fossa disease have a worse outcome than those without lesions in this area, which is why I include posterior fossa signs in my prognostic index when advising patients about MS disease-modifying therapies (DMTs). If you have had a recent MRI you should ask your neurologist if you have any lesions in the posterior fossa.
The following is a list of some of the symptoms that can be associated with posterior fossa involvement in MS:
Double vision
Oscillopsia (jumping images)
Jerky eye movements
Unsteady gait or ataxia
Incoordination
Vertigo
Tinnitus
Deafness
Hyperacusis
Nausea
Vomiting
Hiccoughs
Slurred speech
Swallowing problems
Loss of taste
Loss of sensation on the face or in the mouth
Emotional incontinence or inappropriate crying or laughing
Hallucinations (pontine hallucinosis).
Cognitive impairment
Recently we have begun to identify cognitive impairment has been linked to disease of the cerebellar hemispheres. Typically pwMS with severe cerebellar dysfunction have poor memory and the correct sequencing of memories. PwMS who have severe cerebellar involvement may come across as being very vague. As many fibre tracts pass through the brainstem weakness of the limbs, loss of sensation on the body, bowel, bladder and sexual problems can also occur from brainstem disease. It is clear that the brain stem is a very important structure and needs to be protected from the ravages of MS whenever possible.
There are many specialised neurophysiological techniques to assess brainstem function. Unsurprisingly, pwMS with brainstem involvement have more disability.
Cardiovascular and autonomic dysfunction is not uncommon in MS and is related to the involvement of the autonomic areas of the brain that supply the heart; these are located in the area of the brain stem called the medulla oblongata. It has been suggested that the involvement of these areas may contribute to the occurrence of sudden death in MS. There are case reports of people with active relapsing-remitting MS who have died unexpectedly due to the sudden onset of cardiac arrhythmias. Post-mortem examinations in these cases have shown the presence of active demyelinating lesions in the medulla oblongata. I suspect, sudden death in MS or SUDMUS may be commoner than we think. In epilepsy, for example, it took decades for neurologists to recognise sudden death in epilepsy or SUDEP as being a problem.
We have meant symptomatic treatments and/or specialised and targeted neurorehabilitation programmes for the problems caused by posterior fossa lesions. If you have any of these symptoms and they are impacting your quality of life and ability to function, please speak to your HCP about them. Over the next few years, I am sure to write individual MS-Selfie Newsletters on each of the specific problems mentioned in the list above.
I’m assuming that knowing how MS can affect the function of different parts of your brain and spinal cord will help you understand your MS. Is my assumption wrong?
Subscriptions
I am encouraging readers to subscribe to the MS-Selfie Newsletter. The subscriptions will give you access to the case studies and the archive of these case studies. Please note all other newsletters, such as this one, are free. The money from subscriptions will be used to administer, transfer and curate the contents of the Newsletter onto a companion MS-Selfie microsite. The objective is to create an MS self-help guide.
The MS-Selfie case study from the 27th of September is about the management of a woman with rapidly evolving severe MS who is failing natalizumab and wants to start a family.
Please note if you have MS and can’t afford the subscription please drop me an email and I can arrange a complimentary one.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.




Thank you, and yes, it is very helpful! I was diagnosed 40 years ago in 1981, with RRMS, and have now been in SPMS for several years. My MS is considered inactive, but I have many lesions both on the brain and on the brain stem and spine. I do have gait issues, vertigo occasionally and have experienced most of the symptoms listed at one time or another, as well as others. I refuse to give up, and I stay active, walking, gardening, volunteering with the Master Gardeners and the Humane Society. I am not on any DMT currently, and I see my Neurologist up to 4 times a year for check-ups.
I’ve read this article and it describes my MS to a tee! At time of official diagnosis my MRI showed many lesions on my spine, whole brain and brain stem with one of the most significant appearing as a ‘chunk’ penetrating into my cerebellum! I have experienced almost all of the symptoms listed! I was started on Ocrevus as my first line treatment and it has been amazing for me! I went through an horrendous time for 18 months suffering from up to five seizures a day but after just over two years on this amazing drug things have calmed right down and I live with relatively little disability with my main symptoms being extreme fatigue and cognitive impairment. I actually view myself as a bit of a medical miracle and I do think the amount of exercise I have done over the years and still to this day has help to keep the disability at bay? I still manage to swim 2km a day (most days)-it’s my therapy!