Are you ahead of the curve?
When I attended the European Association of Neurologists (EAN) meeting in June this year, there was a massive focus on Brain Health and the neurologist's role in promoting this concept. This coincides with the WHOs position paper on “Optimizing brain health across the life course: WHO position paper” (9-Aug-2022). We in the MS community discussed this issue a decade ago, and I launched the first MS brain health challenge in 2016.
Yes, I think we were ahead of the curve.
MS Brain Health
In 2014 I was contacted by a group of very bright women who had been reading my posts on the MS Blog about the proactive management of MS. They thought that I needed to extend my reach into policy and speak to policymakers about the importance of brain health and why time matters in the treatment of MS. A year later, this led to our “Brain Health: Time Matters” policy report (2015) that has helped change the way we manage MS. If you haven’t read the original report and the subsequent publications that have arisen from the report I would urge you do so. All the necessary material is curated on our website.
Marginal gains
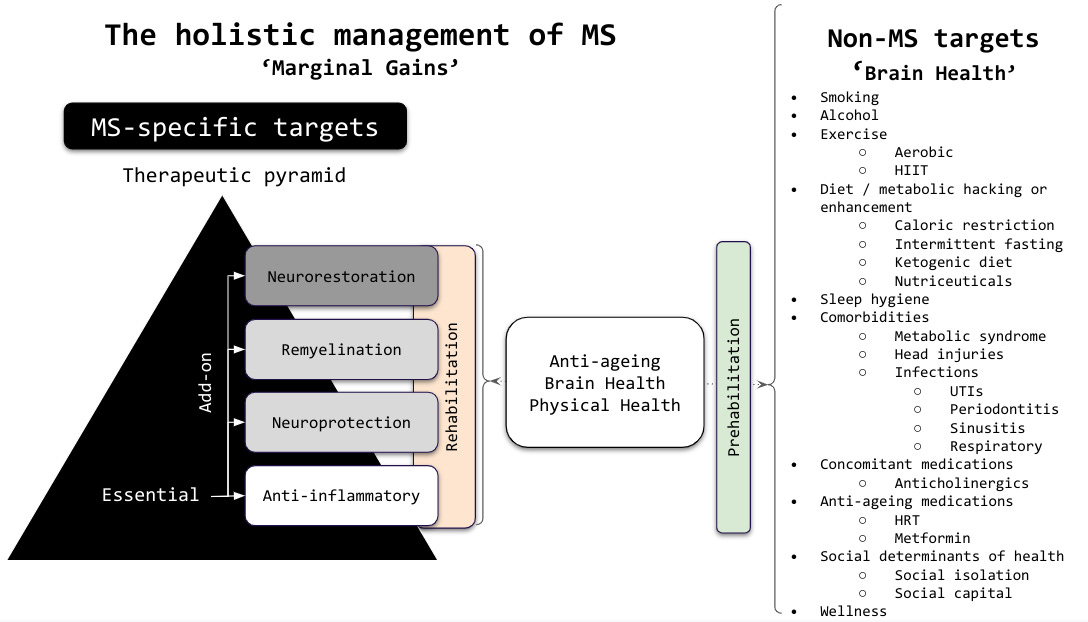
Embedded in the report is the principle we need to manage MS holistically. To achieve this, I have started to adopt the principle of marginal gains as a treatment philosophy for the management of MS. This philosophy is based on Sir David Brailsford's approach to competitive cycling and is one of the reasons why the British cycling teams have been so dominant in the last two decades.
“The whole principle came from the idea that if you broke down everything you could think of that goes into riding a bike, and then improved it by 1%, you will get a significant increase when you put them all together.”
Sir David Brailsford (Brailsford 2015).
"If we break down everything we can think of that goes into improving MS outcomes and then improving it by 1%, we will get a significant improvement when we put them all together.”
Prof G, MS-Selfie, 2022
Improving all the little things will maximise your chances of having very good or excellent MS outcomes. MS impacts you over your lifetime, which is why we need to shift our/your focus on what happens to you in 20, 30 or 40 years time. This means not only treating MS-specific issues, but also focusing on other factors affecting brain health.
So how do you achieve this?
We know from both MS and the general population that lifestyle factors negatively impact brain health and result in worse MS outcomes, for example, smoking, excess alcohol consumption and common co-morbid diseases such as hypertension, diabetes, obesity, high cholesterol and blood lipids, and a sedentary lifestyle (Marrie 2017). This is why it is important to stop smoking, and if you can’t kick your nicotine habit, you are entitled to ask for nicotine replacement therapies (gum, skin patches or e-cigarettes) on the NHS (Sharma et al. 2017).
Obesity and being overweight increase your risk of developing several other diseases that are poor for brain health. If you need help with dietary advice, please discuss this with your GP or family doctor or us. Referral to a dietician may be necessary (NICE 2022). Please remember there is no such thing as an MS diet. Diets must be personalised and compatible with your lifestyle. I recommend reading my newsletter, ‘Which is the best MS diet?’ (25-Aug-2021) for more information on this issue.
Exercise is not only good for your general health, but it improves brain health as well. In the general population, regular exercise has been shown to reduce one's risk of developing dementia (Livingston et al. 2020). There is also evidence that people with MS who exercise regularly have better outcomes than those who do not exercise (Motl et al. 2017). Exercise is a difficult one for people with physical disabilities. However, even people who are wheelchair-bound can benefit from upper limb exercises for health and well-being (Silveira et al. 2022). The WHO recommends at least 150 to 300 minutes of moderate aerobic activity per week (or the equivalent of vigorous activity) (WHO 2020). There is also evidence that high-intensity interval training (HIIT) may be as beneficial, or even more beneficial, than moderate aerobic exercise for people with MS (Joisten et al. 2021). The advantage of HIIT is that as few as three 15-minute sessions per week may be sufficient (Phillips et al. 2017). If you need help with exercise, please speak to us or ask to be referred to a physiotherapist.
Relevant MS-Selfie Newsletters on exercise for you to revisit are:
(1) ”Exercise, exercise, exercise ... how important is it?” (9-Mar-2022)
(2) ”Exercise: how important is it? (23-Nov-2022)”.
Sleep hygiene is crucial for brain health (Livingston et al. 2020). People with multiple sclerosis often have poor sleep hygiene (Zhang et al. 2022). MS causes problems that prevent you from getting a good night's sleep, for example, nocturia or needing to go to the toilet at night, restless legs, leg spasms, pain and anxiety. PwMS may have sleep disorders such as obstructive sleep apnoea that prevents the brain from getting enough good quality sleep (Zhang et al. 2022; Braley and Chervin 2015). Therefore you need to reflect on and, if necessary, assess your sleep quality. If you wake in the morning after an adequate night’s sleep and don’t feel refreshed, you may need to be investigated for sleep disorders or have the MS-related problems mentioned above addressed.
Relevant MS-Selfie Newsletters on sleep for you to revisit are:
(1) “Are you sleep-deprived?” (18-Aug-2021)
(2) “Why am I so fatigued? (9-Aug-2021)
(3) “Food coma” (12-July-2021).
Infections, particularly recurrent infections, exacerbate MS symptoms and may speed up disease worsening (Medeiros Junior et al. 2020). This is why you need to try and prevent or reduce your chances of getting infections. This includes looking after and optimising your bladder function, ensuring your swallowing is safe, having annual vaccinations according to national guidelines and practising good oral hygiene. The most troublesome infections in people with MS tend to be urinary tract infections (Medeiros Junior et al. 2020). If you have recurrent urinary tract infections, you need to see a continence advisor for advice on what can be done to reduce your risk of urinary tract infections. Occasionally you may need to be referred to a urologist for more extensive investigations to rule out uncommon urological causes of recurrent UTIs, for example, bladder stones. Some people with more advanced MS have choking episodes and swallowing problems, which may cause them to get recurrent episodes of aspiration pneumonia (Alali, Ballard, and Bogaardt 2016). If this happens, it is important to see a speech and language therapist to have an assessment and receive advice on how to eat and swallow more safely (Alali, Ballard, and Bogaardt 2016). Vaccinations are also recommended to reduce your risk of getting infections; these typically include the annual flu vaccine and, going forward, COVID vaccines. If you are on immunosuppressive therapy, please see if you are eligible for the pneumococcal and other vaccines. Good oral hygiene prevents tooth and gum disease or periodontitis, which is associated with poor health outcomes (Campos et al. 2022).
Relevant MS-Selfie Newsletters on infections for you to revisit are:
(2) “How to interpret a urine dipstick result” (22-Sep-2022).
Many medications we use to treat MS-related symptoms are poor for brain health. In particular, the class of anticholinergic medications that cross the blood-brain barrier into the central nervous system (Taylor-Rowan et al. 2022). Common anticholinergics medications that enter the brain are the older generation drugs for bladder frequency, for example, oxybutynin, many over-the-counter antihistamines and some older antidepressants, for example, tricyclic antidepressants such as amitryptiline (please see “Amitriptyline: the neurologist's dirty little secret” (29-Sep-2021)). Anticholinergic drugs are the ones that tend to give you a dry mouth or constipation. If you are on an anticholinergic, please discuss it with us, and we can see if there is an appropriate alternative.
Social determinants of health, mental health problems, loneliness and social isolation are all bad for brain health (Livingston et al. 2020). If you suffer from financial problems, are depressed or anxious, are lonely and feel isolated, please speak to us. People with MS are generally more stressed, and the reasons for this are not always obvious, but chronic stress is often related to these social and mental health factors. Therefore it is important to address these problems if they affect you. The NHS has invested money in social prescribing to help counter these problems. As your MS team, we can advise you and signpost you to community services to address these problems.
A relevant MS-Selfie Newsletter on social determinants:
(1) “War: a forgotten social determinant of health” (14-Mar-2022).
Finally, brain health is arguably a part of wellness, which is practising healthy habits daily to attain better physical and mental health outcomes so that instead of just surviving, you thrive. To thrive, you must also assess how you interact with society and the environment. This is why wellness programmes, generally unavailable on the NHS, encourage you to focus on your intellectual, emotional, physical, social, spiritual, occupational and environmental well-being. To achieve this, you may need professional help. We recommend people with MS use mindfulness to help them live with having MS. Improving all these little things, which include preparing yourself for hardship in the future, will impact your brain health and wellness and help optimise your outcome living with MS. This is why prehabilitation is important, i.e. getting yourself as physically healthy as possible just in case you run into problems in the future. I did put together a prehabilitation programme for pwMS during the height of the COVID-19 pandemic, but it remains relevant for whatever awaits you in the future (please see “Prehabilitation the ultimate in self-help” (5-July-2022)).
I want to know how practical this advice is and whether or not you are practising the marginal gains philosophy in relation to self-managing your MS?
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription, please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry or Barts Health NHS Trust. The advice is general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional who will be able to help you.
References
Alali, Dalal, Kirrie Ballard, and Hans Bogaardt. 2016. “Treatment Effects for Dysphagia in Adults with Multiple Sclerosis: A Systematic Review.” Dysphagia 31 (5): 610–18.
Brailsford, Dave. 2015. “Dave Brailsford and Marginal Gains.” BBC. September 15, 2015. https://www.bbc.co.uk/news/magazine-34247629.
Braley, Tiffany J., and Ronald D. Chervin. 2015. “A Practical Approach to the Diagnosis and Management of Sleep Disorders in Patients with Multiple Sclerosis.” Therapeutic Advances in Neurological Disorders 8 (6): 294–310.
Campos, Julya Ribeiro, Carolina Castro Martins, Sandro Felipe Santos Faria, Ana Paula Carvalho, Alexandre Godinho Pereira, Fernando Oliveira Costa, and Luís Otávio Miranda Cota. 2022. “Association between Components of Metabolic Syndrome and Periodontitis: A Systematic Review and Meta-Analysis.” Clinical Oral Investigations 26 (9): 5557–74.
Joisten, Niklas, Annette Rademacher, Clemens Warnke, Sebastian Proschinger, Alexander Schenk, David Walzik, Andre Knoop, et al. 2021. “Exercise Diminishes Plasma Neurofilament Light Chain and Reroutes the Kynurenine Pathway in Multiple Sclerosis.” Neurology(R) Neuroimmunology & Neuroinflammation 8 (3). https://doi.org/10.1212/NXI.0000000000000982.
Livingston, Gill, Jonathan Huntley, Andrew Sommerlad, David Ames, Clive Ballard, Sube Banerjee, Carol Brayne, et al. 2020. “Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission.” The Lancet 396 (10248): 413–46.
Marrie, Ruth Ann. 2017. “Comorbidity in Multiple Sclerosis: Implications for Patient Care.” Nature Reviews. Neurology 13 (6): 375–82.
Medeiros Junior, Washigton Luiz Gomes de, Caio Cesar Demore, Larissa Peres Mazaro, Matheus Fellipe Nascimento de Souza, Laura Fiuza Parolin, Luiz Henrique Melo, Claudio Rogerio Werka Junior, and Marcus Vinicius Magno Gonçalves. 2020. “Urinary Tract Infection in Patients with Multiple Sclerosis: An Overview.” Multiple Sclerosis and Related Disorders 46 (November): 102462.
Motl, Robert W., Brian M. Sandroff, Gert Kwakkel, Ulrik Dalgas, Anthony Feinstein, Christoph Heesen, Peter Feys, and Alan J. Thompson. 2017. “Exercise in Patients with Multiple Sclerosis.” Lancet Neurology 16 (10): 848–56.
NICE. 2022. “Obesity: Identification, Assessment and Management.” National Institute for Health and Care Excellence. August 9, 2022. https://www.nice.org.uk/guidance/cg189.
Phillips, Bethan E., Benjamin M. Kelly, Mats Lilja, Jesús Gustavo Ponce-González, Robert J. Brogan, David L. Morris, Thomas Gustafsson, et al. 2017. “A Practical and Time-Efficient High-Intensity Interval Training Program Modifies Cardio-Metabolic Risk Factors in Adults with Risk Factors for Type II Diabetes.” Frontiers in Endocrinology 8 (September): 229.
Sharma, Ratika, Kristel Alla, Daniel Pfeffer, Carla Meurk, Pauline Ford, Steve Kisely, and Coral Gartner. 2017. “An Appraisal of Practice Guidelines for Smoking Cessation in People with Severe Mental Illness.” The Australian and New Zealand Journal of Psychiatry 51 (11): 1106–20.
Silveira, Stephanie L., Brenda Jeng, Gary Cutter, and Robert W. Motl. 2022. “Perceptions of Physical Activity Guidelines among Wheelchair Users with Multiple Sclerosis.” Multiple Sclerosis Journal - Experimental, Translational and Clinical 8 (2): 20552173221097580.
Taylor-Rowan, Martin, Olga Kraia, Christina Kolliopoulou, Anna H. Noel-Storr, Ahmed A. Alharthi, Amanda J. Cross, Carrie Stewart, Phyo K. Myint, Jenny McCleery, and Terry J. Quinn. 2022. “Anticholinergic Burden for Prediction of Cognitive Decline or Neuropsychiatric Symptoms in Older Adults with Mild Cognitive Impairment or Dementia.” Cochrane Database of Systematic Reviews 8 (August): CD015196.
WHO. 2020. “Physical Activity.” World Health Organization. November 26, 2020. https://www.who.int/news-room/fact-sheets/detail/physical-activity.
Zhang, Ye, Rong Ren, Linghui Yang, Haipeng Zhang, Yuan Shi, Michael V. Vitiello, Larry D. Sanford, and Xiangdong Tang. 2022. “Sleep in Multiple Sclerosis: A Systematic Review and Meta-Analysis of Polysomnographic Findings.” Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, September. https://doi.org/10.5664/jcsm.10304.















Share this post