As natalizumab’s or Tysabri’s patent is about to expire Biogen the company that market’s the product has launched a new subcutaneous (SC) formulation and now have a very active marketing campaign to get us to switch our patients from the IV formulation to the SC formulation. Their argument is that moving from a 60-minute intravenous infusion to two subcutaneous injections of 1mL each will save both the NHS and patient’s on natalizumab time.
Another lever that Biogen is pulling is that have said they will be withdrawing all nursing support for natalizumab infusions across the UK. You may ask why does the NHS need support to administer natalizumab infusions? The sad thing is that most MS infusion services are understaffed and MS pharmaceutical companies employ or pay for additional infusion nurses to help with the infusion of their products. In our unit, we have had support from Biogen infusion nurses for many years to help with natalizumab infusions.
The following is an email I received from Biogen on 17-March-2022 making the case for the switch from IV to SC formulation.
Why the sudden push from Biogen to get the SC-Tysabri formulation adopted?
The threat is that Sandoz, a generics and biosimilar company owned by Novartis, is planning to launch a natalizumab biosimilar in the near future. As biosimilars are cheaper than innovator compounds it is likely the NHS will mandate we switch from Natalizumab to the biosimilar to save the NHS money. If, however, all our patients on natalizumab are on the SC formulation and we start using the SC formulation in natalizumab-naive patients then Biogen will protect its market share; at least for a time as Sandoz will have to develop a SC-biosimilar themselves and this will take time.
A very similar thing happened with glatiramer acetate (Copaxone). Teva the company that manufactured Copaxone pushed to get all pwMS on the 20mg SC daily Copaxone formulation to switch to the 40mg SC three times a week formulation just before the patent expired and a 20-mg biosimilar was launched. The pharmaceutical companies refer to these tactics as the life-cycle management of their product with the aim of maintaining market share beyond the date of the patent expiry.
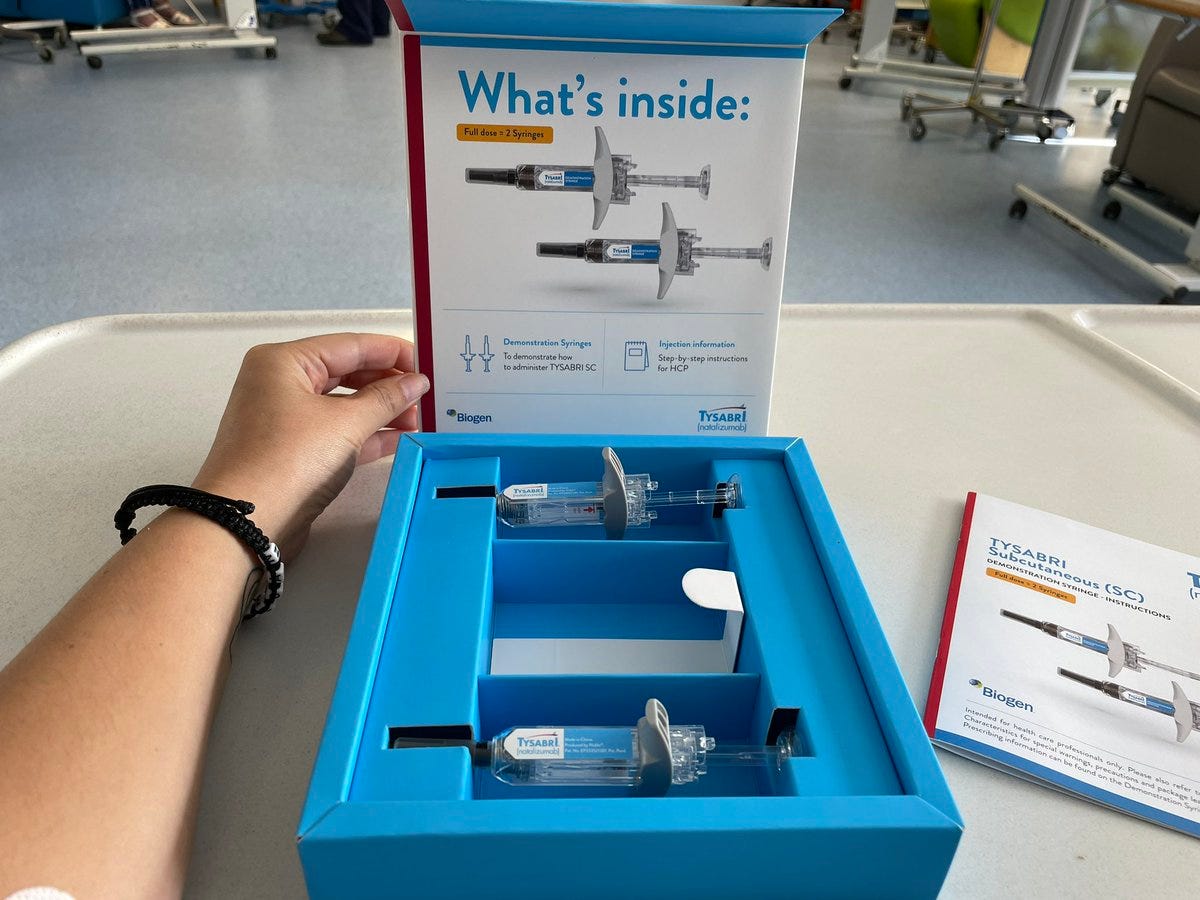
Biogen is making the argument that the SC formulation will save both patients and staff time, but is this correct? PwMS on natalizumab will still have to come to the hospital for their two SC injections and will still have to wait for an hour to make sure that they don’t have an allergic reaction to the injections. Yesterday, I heard that the Tysabri injections have to be left at room temperature for at least 30 minutes, to allow their contents to warm up to room temperature before being administered. Unless this is preplanned this 30-minute wait may need to be added onto the time it takes to give sc Tysabri. So the actual time saving may be small. What about the patient? Would you prefer a short intravenous infusion or two relatively large SC injections? I suspect some pwMS will choose the former and some the latter. This is why patients on natalizumab should be given the choice on whether or not to switch from the IV to SC formulation of Tysabri. Do you agree?
Another worrying thing that I was not aware of until earlier this week is that the FDA has rejected Biogen’s application for the SC-Tysabri formulation. I tried to find the reason online and couldn’t. I then emailed a Biogen member of staff who passed my email up the chain of command and have yet to get a response. I then did some of my own detective work and I suspect the reason may be a lack of anti-drug antibody (immunogenicity) data. The data on how much natalizumab is absorbed from the skin enters the circulation (bioavailability) and blocks the velcro (receptors) on circulating lymphocytes, i.e the so-called pharmacokinetics and pharmacodynamics of SC-natalizumab seems convincing enough, but not the data on anti-drug antibodies or ADAs.
As you know all biological or protein-based therapies have the potential to induce your own immune system to produce ADAs, which are usually neutralizing antibodies or NABs. With iv-natalizumab this occurs in roughly 10% of subjects within the first 6 months and persists in about 6% of patients at 12 months. These antibodies not only stop natalizumab from working but are a common reason for infusion reactions; 75% of study subjects with ADAs get infusion reactions, which leads to them having to stop natalizumab.
The European Summary of Product Characteristics (SPC) states the following in relation to SC-Tysabri’s immunogenicity:
“In 10% of patients antibodies against natalizumab were detected in 2-year controlled clinical trials in MS patients receiving natalizumab intravenously. Persistent anti-natalizumab antibodies (one positive test reproducible on retesting at least 6 weeks later) developed in approximately 6% of patients. Antibodies were detected on only one occasion in an additional 4% of patients. Persistent antibodies were associated with a substantial decrease in the effectiveness of natalizumab and an increased incidence of hypersensitivity reactions. Additional infusion-related reactions associated with persistent antibodies included rigors, nausea, vomiting and flushing (see section 4.4). In the 32-week DELIVER study in MS patients with no prior exposure to natalizumab, persistent anti-natalizumab antibodies developed in 1 subject (4%) from 26 subjects who received natalizumab subcutaneously. Antibodies were detected on only one occasion in another 5 subjects (19%). In the 60-week REFINE study in MS patients, no subjects (136 subjects) who switched from natalizumab intravenous administration to subcutaneous administration had detectable ADA during the study (see section 5.1).
If, after approximately 6 months of therapy, persistent antibodies are suspected, either due to reduced efficacy or due to the occurrence of infusion-related events, they may be detected and confirmed with a subsequent test 6 weeks after the first positive test. Given that efficacy may be reduced or the incidence of hypersensitivity or infusion-related reactions may be increased in a patient with persistent antibodies, treatment should be discontinued in patients who develop persistent antibodies.”
I suspect the FDA looked at this data and said it is simply not robust enough. I don’t blame them. The data from the REFINE study can’t be used as all these subjects had been on iv-natalizumab for at least a year and were ADA negative before starting SC-Tysabri (Trojano et al. Mult Scler. 2021 Dec;27(14):2240-2253). Therefore the only immunogenicity data available is from the DELIVER study which included natalizumab-naive subjects. Six natalizumab-naive subjects out of 26 (23%) developed ADAs with ADAs persisting in only 1 subject (Plavina et al. J Clin Pharmacol. 2016 Oct;56(10):1254-62). This is clearly a very small study and does not give me any confidence in using the SC-Tysabri formulation in naive patients.
In general, the subcutaneous route of administration tends to be more immunogenic than the intravenous route. The reason for this is that the protein, in this case, natalizumab an antibody, first has to go via regional lymph nodes before getting into the circulation and the lymph nodes are primed for making antibody responses. In comparison when you give a drug intravenously, particularly in large doses, most goes to the spleen and it tends to trigger so-called high-zone tolerance a mechanism that causes the immune system to ignore foreign proteins and to treat them as self, i.e to not make an ADA response.
I suspect the FDA regulators remember what happened with EPREX a subcutaneous formulation of a drug called erythropoietin - also known as EPO - that stimulates the production of red blood cells in the bone marrow. When patients with chronic renal failure were moved from intravenous EPO to sc-EPO (EPREX) it resulted in an epidemic of a condition called aplastic anaemia, because the ADAs induced by EPREX neutralised the body’s own EPO. The EPREX saga was a watershed moment in how regulators manage biosimilar medications and required extensive immunogenicity data and now require an extensive immunogenicity data package before licensing a biosimilar.
On reflection, I am not surprised the FDA rejected Biogen’s SC-natalizumab application and I am very surprised the EMA has licensed it. Why? When I was the principal investigator on the Rebif New Formulation (RNF) study, which was designed to reduce the immunogenicity of SC interferon-beta-1a, the regulators were adamant we needed at least 200 subjects treated for two years for the study to pass muster. When I say the regulators I mean both the EMA and FDA. I suspect the EMA blinked with SC-natalizumab, but not the FDA and I suspect they have asked Biogen to do a proper immunogenicity study.
Does this have implications for clinical practice? Yes, it does. On reflection, I will now be very uncomfortable starting natalizumab-naive patients on SC-natalizumab and will recommend we use the iv formulation for 12 months before offering a switch to the SC formulation. In this way, we will potentially reduce the risk of unnecessarily exposing our patients to the development of ADA from the SC administration route.
What about saving time? I think we should now go ahead and do a safety study of the standard 1-hour infusion of iv-natalizumab and compare it to a rapid 15 min infusion time and a bolus push-in over 60 seconds. This study will need to be done in all subjects who have been on natalizumab for 6-months or more and are anti-natalizumab ADA negative. I am prepared to offer good odds that both the rapid and bolus push-in administration of natalizumab will be well tolerated and will not cause any safety concerns. In fact, I did ask Biogen to do this study a few years ago but they declined. Maybe Sandoz who will be manufacturing and marketing the natalizumab biosimilar should do this study. If they want a marketing advantage over Tysabri that is not only based on price this could be an opportunity.
If you are on iv-Tysrbri would you be willing to participate in a study to shorten the time it takes to administer the drug?
Do you find these types of posts of interest? The reason why I am discussing this issue is that it has relevance to pwMS on natalizumab and pwMS who may have to make a decision to start natalizumab in the future. Hopefully, this Newsletter will help you make an informed decision between the SC and IV formulation assuming you are given a choice between the two formulations.
Subscriptions and donations
I am using the paid subscriptions to administer the MS-Selfie Newsletter and associated MS-Selfie microsite that is currently in development. If you are an active paying subscriber thank you, your contribution is much appreciated. At the request of several readers, I have now added the option of making a one-off donation as well. Funds from subscriptions and donations are being used to pay a professional medical writer to curate, rewrite and transfer the contents of the Newsletter onto a companion MS-Selfie microsite, which is being designed and maintained by a freelance web designer.
Thank you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.















Share this post