I have had several people with MS write to me about how unsatisfactory their annual follow-up consultation is. I suspect the short and incomplete annual assessments are part of a broader problem in the NHS related to understaffing and an increasing number of people with MS. Another aspect is that as pwMS get more educated about having MS and living with its consequences, they are expecting more from their MS services including more time with their MS neurologist and MS nurse specialist.
More than fifteen minutes is needed for an annual follow-up appointment. Do you agree? These are just some of the reasons why.
Since the NHS adopted a specialist model of MS care to improve the management of people with long-term conditions, you need to remain under your MS service for your care. The Association of British Neurologists recommends follow-up appointments take 15 minutes. From comments on this platform, it is clear that many patients don’t get 15 minutes for their annual appointment. It is also obvious that as our treatment goals get more ambitious and we adopt a holistic approach to managing MS, we need a new way of doing things.
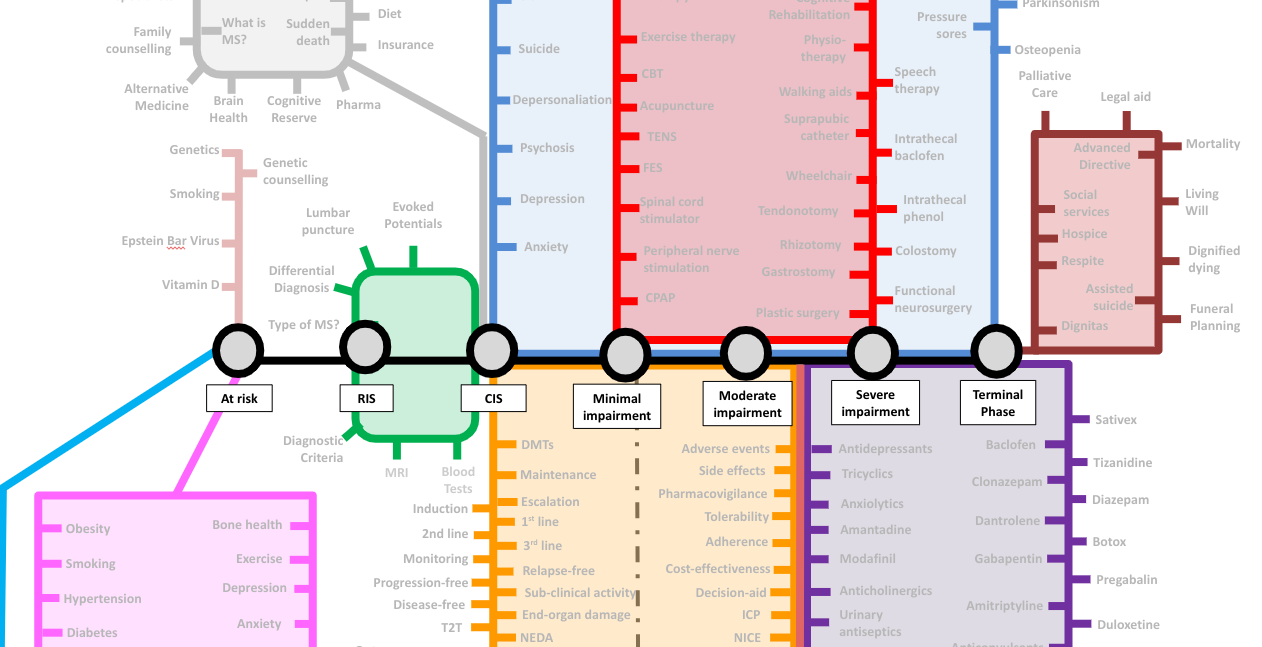
You must know that the needs of people with MS (pwMS) change over time. As an analogy, I used a train journey and the London Underground map to illustrate this. Someone who develops MS typically starts their journey as being at risk of getting MS. They then pass through asymptomatic, prodromal and diagnostic phases. Once diagnosed with MS, they go through the stages of no or minimal disability, moderate disability, severe disability and finally, the terminal stages of having MS. Please note that completing the train ride is not inevitable. Many pwMS hop off when treated with high-efficacy DMTs, particularly early on, preventing them from becoming disabled. I have also included a dashed grey line that leads to long-term remission and an MS cure. This line is still under construction as we don’t have enough data to claim an MS cure.
The needs along the MS journey change, and the annual follow-up appointments must reflect this. Some HCPs want to create specific care pathways to manage all the problems pwMS complain about. However, care pathways can fragment MS care if they are not part of a different and separate specialist service. For example, we may refer patients to see their local continence team or refer them to the spasticity clinic to consider a baclofen pump. A different team deals with these problems, and they justify a specific, well-defined care pathway. Having separate care pathways for multiple problems often increases healthcare utilisation and costs. This is why MS teams should try and deal with most problems themselves.
The following typically needs to be done at the annual follow-up appointment in no particular order:
Is your MS active?
Have you had any relapses in the last 12 months, and has your annual MRI scan shown any new lesions? This is important as it may make you eligible for starting, switching or escalating your disease-modifying therapy (DMT).
Are all your pharmacovigilance and derisking activities been done?
This involves ensuring your blood tests are okay and you have had your annual vaccines and, if necessary, screening for malignancies. Please note that blood tests and procedures required are unique to each class of DMTs; for example, if you are on natalizumab, this will include a 6-monthly JC virus antibody index and potentially a 4-monthly PML monitoring MRI.
Are you stable or getting worse?
In our centre, we are asking patients to self-monitor to get them to engage with their own MS and to save time. We now expect our patients to complete the online web-EDSS, their own timed 25-foot walk and 9-hole peg test, and the online SDMT (symbol digit modality test). Some patients do more than this; for example, they record their walking or running times and produce activity monitoring data. This will be expanded to include neurological stress tests and even home sleep monitoring using wearable technology. Most pwMS have a sleep disorder, which contributes to poor brain health and exacerbates fatigue. Getting people with MS to sleep better will improve many other MS symptoms.
Current medications?
Before a detailed symptom review, I like to review a list of current medications. This can be easy if you remember to take a list with you. Often the medication review forms the basis of the consultation. It is not only the current list that is helpful but any changes from teh last visit and a review of additional supplements. PwMS are increasingly using supplements on top of their prescribed medications to try and improve their outcome. It is incredible how often supplements and alternative therapies hijack the annual visit.
Do you have any symptomatic problems?
This list of symptoms you ask about and apply here depends on where you are on the MS train journey. There is little point asking about spasticity and falls in a patient is not disabled and runs marathons. I always start with the bladder and bowel function and then proceed to sexual dysfunction. In the past, I tended to miss asking women with MS about the latter. This was a cognitive bias, and I now ask all my patients. If someone attends a clinic with a friend or family member, it may be inappropriate to discuss their sexual function, which is why using other tools for monitoring and screening will improve MS care.
Then walking, trips and falls. Even if a patient is not falling, they may be at risk of falls and need to be referred to a fall prevention programme and assess their bone health. The latter involves having a DEXA or bone density scan and taking vitamin D supplements (4,000U per day). If you are osteoporotic, you have been prescribed calcium.
I then move on to fatigue, sleep, nocturnal spasms, restless legs and pain. I then bring up the issue of mood and anxiety, which are common problems in pwMS.
Brain Health
I try to address all the issues I have mentioned in the past that can impact brain health, including exercise, diet, comorbidities and other lifestyle factors such as alcohol, smoking and other substances and HRT (hormone replacement therapy). In an ideal world, I would love to be able to screen my patients for hypertension and the state of their metabolic health, but I don’t have time for this, and the management of these problems needs to be done by the general practitioner. It is quite depressing that many of my patients who have comorbid hypertension or diabetes are not as engaged with managing their comorbidities as much as their MS. If you have hypertension and/or diabetes, you need to self-monitor your blood pressure and blood sugars and feedback the information to your GP.
Social Determinants of Health
More recently, I have started addressing modifiable social determinants of health. This includes questions about work, whether patients come out each month financially, loneliness and social isolation. We focus on social issues because we can now refer or ask the GP to refer patients for help using social prescribing.
Cognition
I don’t specifically ask about cognition because self-reporting cognitive problems is not helpful. I am unsure if you know that pwMS who complain of cognitive problems are more likely to be depressed and anxious than have significant cognitive impairment. I prefer to pick up clues from the consultation that cognition is an issue and try and deal with the consequences as best I can. For example, an occupational health assessment may be the most appropriate action if someone is not coping at work. Now that we are monitoring cognition with the online SDMT, it is noteworthy that some people with relatively low scores still cope very well at work.
Activities of Daily Living
In patients who are disabled, it is important to ask about activities of daily living. Are they managing their own self-care? Can they wash and dress themselves? Brush their teeth? What is the state of the oral hygiene? Do they have caries or gum disease that needs attention? Who is looking after their feet? Can they cut their toenails? Do they need a referral to a podiatrist? Can they wash, dry and brush their hair? Can they transfer themselves from the bed to the wheelchair to the toilet? If they are battling, do they have the necessary home adaptations? In almost every clinic, one or two of my patients must be seen by the community-based disability team because of these problems.
Social Care
For some patients, we need to address other social issues, i.e. is the care package sufficient, and are they managing to get everything done when their carers come in? Sometimes their carers are on such a tight schedule and can’t even wait for their clients to complete a meal. This may result in a truncated feeding time. I have had rare patients who become malnourished as a result.
Bulbar function
In pwMS, who are more disabled, I always ask about swallowing problems and choking episodes. This frequently prompts a referral for a speech and language assessment. Similarly, if their speech is affected, they may need help.
Advanced Directives
On top of this, we need to prompt patients to get their GP to complete an advanced directive (a form or a living will). This needs to be done early in the course of the disease when you have insight and can discuss the issues with your partner and family. Waiting until you have advanced MS is too late for an advanced directive.
Question time and trials
On top of the above, we are expected to give our patients time to ask questions. This usually prompts questions about MS research and clinical trials. Discussing clinical trials takes time.
I give my average patients more than 15 minutes, but I often have to limit the consultation or precis what is discussed because of time constraints. This is why I am a big fan of asynchronous consultations using email or a portal that automates some of the above may help, and why you need to be more proactive about managing your own MS.
Please note I was once heavily criticised for including the more advanced and terminal phases of MS as part of the MS journey. I was told pwMS don’t need to know about this. The argument was that people recently diagnosed or with early MS don’t need this information upfront; they can learn about it later. I countered the argument that unless they know how severe MS can become, how will they incorporate this into their decision-making about MS risk and the risks associated with treating MS with high-efficacy DMTs? Asymmetric knowledge creates cognitive biases; pwMS have the right to know about the late stages of MS and its consequences. Deliberately holding back this information is tantamount to malpractice and would not be considered appropriate from a legal perspective.
This newsletter is not meant to be comprehensive but is written to provide an overview of our problems with managing MS holistically on the NHS. The solutions are self-management and using technology to help.
Please let me know if I missed anything and what your annual MS review is like. Please note I have written previously on preparing for your annual follow-up appointment, using ‘My MS Piorities’ and ‘Your MS Questionnaire’. This advice still holds (see ‘What are your priorities in relation to 'Your MS'?’; 4-Oct-2021).
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.













Share this post