The following is a list of questions from Dr Iman Redha our MENACTRIMS Trainee that she had after watching me give a webinar on sequencing MS DMTs in the presence of lymphopaenia.
1. Would you be worried about starting azathioprine for inflammatory bowel disease (IBD) in a patient who has a diagnosis of MS on fingolimod given the risk of lymphopenia?
Yes, I would be. As you are probably aware S1P modulators work in IBD. Recently ozanimod, a second-generation S1P modulator has been shown to be effective in IBD. Therefore combining fingolimod with azathioprine would concern me regarding more intense immunosuppression from the combination.
Baumgart & Le Berre. Newer Biologic and Small-Molecule Therapies for Inflammatory Bowel Disease. N Engl J Med. 2021 Sep 30;385(14):1302-1315.
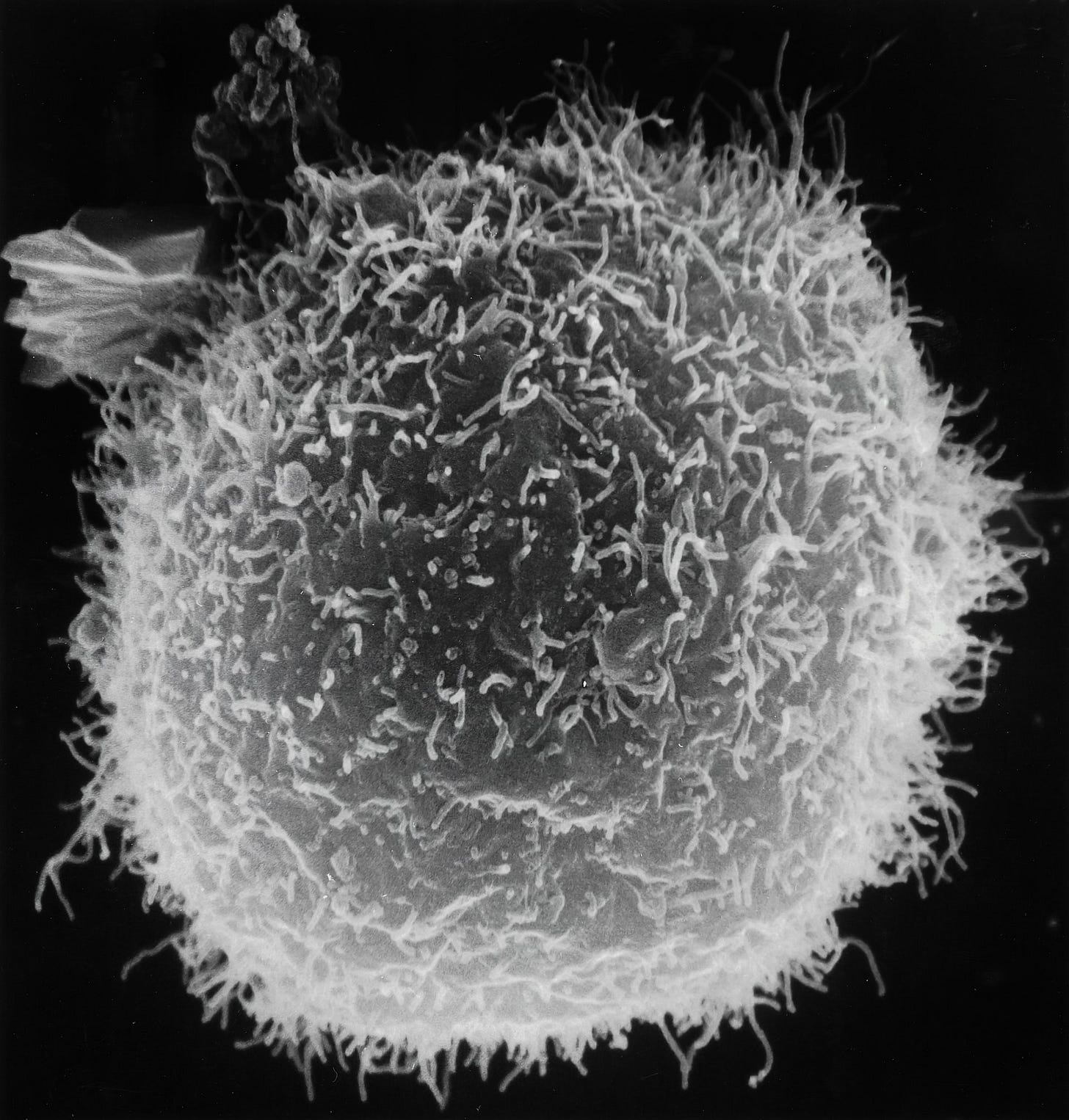
Azathioprine is an antimetabolite and inhibits purine synthesis. Although, its exact mechanism of action is not entirely understood it is likely to be related to its inhibition of purine synthesis, along with inhibition of B and T cells. 6-thioguanine triphosphate, a metabolite of azathioprine, modulates activation of rac1 when costimulated with CD28, inducing T cell apoptosis, which may be mediated through rac1's action on mitogen-activated protein kinase and NF-kappaB.
In this patient Azathioprine effects on adaptive immunity are likely to increase the general immunosuppression associated with fingolimod.
2. Addressing the same question, what would be your preference in terms of DMTs in a patient who is either on azathioprine or MMF?
I would consider switching this patient to natalizumab. Natalizumab is licensed to treat both MS and IBD and may be more effective and safer than a fingolimod/azathioprine in combination. It is also associated with less systemic immunosuppression. Obviously, you would need to check the JCV status and make a judgement call with the patient about whether or not to start and continue natalizumab long-term.
3. With regards to malignancy, what would be your DMT preference in a patient with renal cell carcinoma, thyroid and breast carcinoma. Would interferon be a good option? Additionally, if the patient was for instance on ocrelizumab, would de-escalating put the patient at risk of relapse?
Yes, in patients with a prior history of malignancy I would go with an immunomodulator (interferon-beta, glatiramer acetate or teriflunomide) and if you need higher efficacy an immune reconstitution therapy (IRT) such as cladribine. The advantage of an IRT is that once immune reconstitution occurs peripheral immune surveillance is restored and hopefully the immune system can keep any metastases, recurrent of the primary or new secondary tumours from developing.
What about natalizumab? The problem with natalizumab is that it reduces trafficking and immune surveillance of the CNS and gastrointestinal tract. This may create a safe haven for metastases to travel to and develop. Saying this not all tumours metastasize to the CNS and many that do use VLA-4 (natalizumab’s target) as part of the mechanism for crossing the blood-brain barrier into the brain. Therefore, the risks associated with natalizumab is theoretical.
Case study: I have had one patient with MS who had bowel cancer with liver and lung metastases who was about to be treated with a combination of two checkpoint inhibitors, which are known to exacerbate MS by stimulating or taking the brake off T-cells. I put this patient on natalizumab during her cancer treatment and her MS remained stable. Saying this bowel cancer infrequently metastasises to the brain, which is why I felt reasonably confident doing this.
Case study: For another patient with rapidly evolving severe MS and a recent history of melanoma, which is a tumour that metastasises commonly to the brain, I avoided natalizumab and chronic immunosuppression, and treated her with cladribine instead. She, unfortunately, has a spinal relapse and month 7 post her first course of cladribine, which prompted me to bring forward her second course of cladribine by 3 months.
4. Is the target lymphopenia more than 0.8 for switching someone from fingolimod or dimethyl fumarate to ocrelizumab or alemtuzumab? Is the same applied for switching to natalizumab?
No. The reason for wanting the lymphocyte count to recover to above 0.8x10^9/L is to make sure when you use another depleting agent you don’t leave the patient chronically lymphopaenic. The risk of lymphopaenia is related to its severity, qualitative changes, for example, are the CD8+ T-cells more affected than the CD4+ T-cells, the duration of lymphopaenia, age or comorbid immunosenescence and their previous treatment history. Some DMTs imprint on the immune system and the risks carry over with them; this may be mild persistent lymphopaenia, which is the norm after alemtuzumab or cladribine, or PML risk, with natalizumab.
Please note the pathogenesis of PML is complex. The wild-type JC virus has to evolve to be able to cause PML with the average PML strain acquiring 4 or 5 mutations in its capsid protein and mutation(s) in its regulatory region. When you stop natalizumab the pre-PML strains are likely to persist in the body and hence increase the risk of PML on the next therapy.
5. In someone with HIV and a new diagnosis of MS what would your DMT of preference be given the risk of opportunistic infections?
Firstly, comorbid HIV and MS are quite rare. Saying this there are a small number of case reports in the literature. Did you know that having HIV protects you from getting MS? We have a theory that highly active antiretroviral therapies (HAART) are active against EBV may work to reduce MS risk via targeting EBV. This is why we did a trial of an antiretroviral (raltegravir) in MS and there is a group in the US doing a similar trial.
Another interesting observation is in people who have MS that predates them becoming HIV positive do very well from the MS perspective when they go onto antiretroviral therapies. We wrote up a case of a patient whose MS has gone into long-term remission after starting antiretrovirals. This observation has been reported by others and is another reason why we need to explore anti-retroviral therapies as a treatment for MS.
So in your scenario above, I would make sure their HIV is well controlled on HAART and I would monitor their MS. If their MS remained active I would then explore treatment with an immunomodulator (interferon-beta or teriflunomide) and not a chronic immunosuppressive therapy. Please note there is good laboratory data that teriflunomide has antiviral effects against HIV-1, which would make it my DMT of choice in this situation.
6. What is your view of using cyclophosphamide in treating patients with highly active MS? If treatments such as cladribine and alemtuzumab have failed and HSCT is not available?
I am not sure if you are aware that a large number of HSCT protocols use cyclophosphamide for both stem cell mobilisation and myeloablation. So HSCT is a form of cyclophosphamide treatment. There is also a large literature on very high-dose cyclophosphamide treatment of MS. This was called Revimmune and was offered by a group at John Hopkins. The Revimmune protocol stopped being used when highly-effective DMTs emerged. However, the real reason was its toxicity and associated complications. The low-dose trials of pulsed cyclophosphamide treatment done in the 1980s were poorly designed and overall the evidence is weak with a high chance of unblinding. I suspect based on its mode of action that low-dose pulsed cyclophosphamide therapy will work as a DMT in MS.
I personally would not advocate cyclophosphamide as a treatment for MS. It is associated with ovarian and testicular toxicity and a relatively high risk of infertility. As a DNA alkylating agent it causes secondary malignancies. The latter is the same reason why mitoxantrone as a treatment for MS has fallen out of favour.
Saying this if I worked in a resource-poor environment and had to look after people with very active MS who couldn’t afford high-cost innovative MS DMTs I would still be using mitoxantrone. In fact, both mitoxantrone and cyclophosphamide are on my essential low-cost alternative DMT list of use in low and middle-income countries (see below).
Azathioprine*
Cladribine
Cyclophosphamide*
Fludarabine*
Leflunomide
Methotrexate*
Mitoxantrone
Rituximab*
Generic dimethyl fumarate (Skilarence)
Compounded dimethyl fumarate
HSCT
*on the 19th WHO Model List of Essential Medicines (April 2015)
Subscriptions/Donations
I have changed the funding model of MS-Selfie. Access to MS-Selfie and the microsite, when it is ready to go live, will be free to all readers. I am therefore relying on voluntary paying subscribers and future paying subscribers to continue supporting the site for everyone. So if you value these Newsletters and Case studies please consider becoming a paying subscriber. I would like to thank those of you who have become paying subscribers already; your support is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.













Share this post