MS-Selfie rose-tinted-odometer = ★★★☆☆
A few readers have recently found some of my newsletters so unsettling and dark that one of them unsubscribed. Therefore, I have reinstated my rose-tinted-odometer, a simple 5-star rating of the type of content the Newsletter contains. The rating will allow you, the reader or listener, to make a call on whether or not you want to be exposed to content that is not so rose-tinted.

Another criticism is that the content of the MS-Selfie podcast and newsletters are not sufficiently curated to allow people with MS and their families to self-manage their condition, and they are written in a way that is too scientific or highbrow, i.e. the content is for HCPs and not pwMS. I’m afraid I have to disagree with the latter criticisms. I have deliberately positioned MS-Selfie at a high level. Firstly, it is my understanding that pwMS want something more than what the MS charities provide. For example, the MS Society’s content is written for a reading age of 12. Am I correct in this assumption? Secondly, as many pwMS become more health literate, they are often as well-informed and, in some cases, better informed than their HCPs. This is why the content on MS-Selfie is for both pwMS, their families and HCPs. With the democratisation of knowledge, everybody has access to similar levels of information and having a platform that potentially caters to both patients and HCPs is an advantage. Or maybe I am being naïve?
One of the main aims of MS-Selfie is health literacy, which gives people with MS (pwMS) agency and the confidence to make decisions about their MS care or to at least ask the questions that will lead to better management of their MS. Health literacy is even being identified by the World Health Organisation as an agent or change.
The WHO has stated that “improving health literacy provides the foundation on which citizens can play an active role in improving their own health, engage successfully with community action for health, and push governments to meet their responsibilities in addressing health and health equity. Promoting health literacy in all but in particularly marginalised societies is crucial in accelerating progress in reducing health inequities and advancing broader social, economic, and environmental goals outlined in the 2030 Agenda for Sustainable Development”.
I want to repurpose what the WHO says about population health literacy in managing MS.
“Improving health literacy provides the foundation for pwMS to play an active role in improving their health, engaging successfully with their HCPs, and pushing payers, third-party providers and their governments to meet their responsibilities in addressing health and health equity in managing MS.”
PwMS interacts with its healthcare professionals (HCPs) at different points in their MS journey. The diagnostic and initial treatment phase tends to take precedence over the rest of the MS journey. However, in reality, the ongoing day-to-day management of MS is much more critical in the life of someone with MS.
As the NHS and other healthcare systems come under increasing pressure due to unsustainable funding models, demographic changes, and economic and political pressures, it is clear that people with chronic diseases need to do more to self-manage the impact of their disease(s) on their functioning. MS is no exception. So, ask not what the NHS or your HCP can do for you but what you can do to help yourself.
Many, if not most, pwMS are dissatisfied with their 3-monthly, 6-monthly or annual follow-up consultations. Yes, in some healthcare systems, for example, Germany, pwMS get 3-monthly follow-up appointments. Short and incomplete follow-up assessments are part of a broader problem in the NHS related to understaffing, an increasing number of pwMS, i.e. both the incidence and prevalence of MS are increasing, and there is less time for patient contact due to the digitalisation of our practice. About the latter, we now have more administrative duties on the electronic health record that consume time. Another aspect that needs to be addressed is that pwMS are more educated about having MS than they were in the past. Hence, they expect more from their MS services, including more time with their MS neurologist and nurse specialist. Many patients come with lists of questions that could quickly be answered by subscribing to a resource such as MS-Selfie. Many patients know the answers to most of these questions but want the answers validated.
So, I would like to ask you for advice on how you would like MS-Selfie to evolve. Do you want me to ‘dumb down’ the content to make it more understandable to MS newbies? Should the content be sugar-coated or rose-tinted? Should I only focus on MS self-management? Should I avoid research topics and other musings that are arguably quite obtuse?
The following is an example of what a typical self-management newsletter could look like.
Self-Management 101 - What to expect from your scheduled follow-up appointments
Preparing for your follow-up appointments is important. Before you arrive at the clinic, collect data and complete a proforma. A well-designed clinic proforma could act as a crib or manifesto for the self-management of MS.
Since the NHS adopted a specialist model of MS care to improve the management of people with long-term conditions, you need to remain under your MS service lifelong. Yes, until we prove we can cure you of having MS, MS remains a lifelong condition, and hence, you need lifelong support from a specialist MS service.
The Association of British Neurologists recommends follow-up appointments take 15 minutes. From comments on this platform, it is clear that many patients don’t get 15 minutes for their annual appointment. It is also evident that as our treatment goals get more ambitious and we adopt a holistic approach to managing MS, we need more than 15 minutes for follow-up appointments, or we need a new way of doing things.
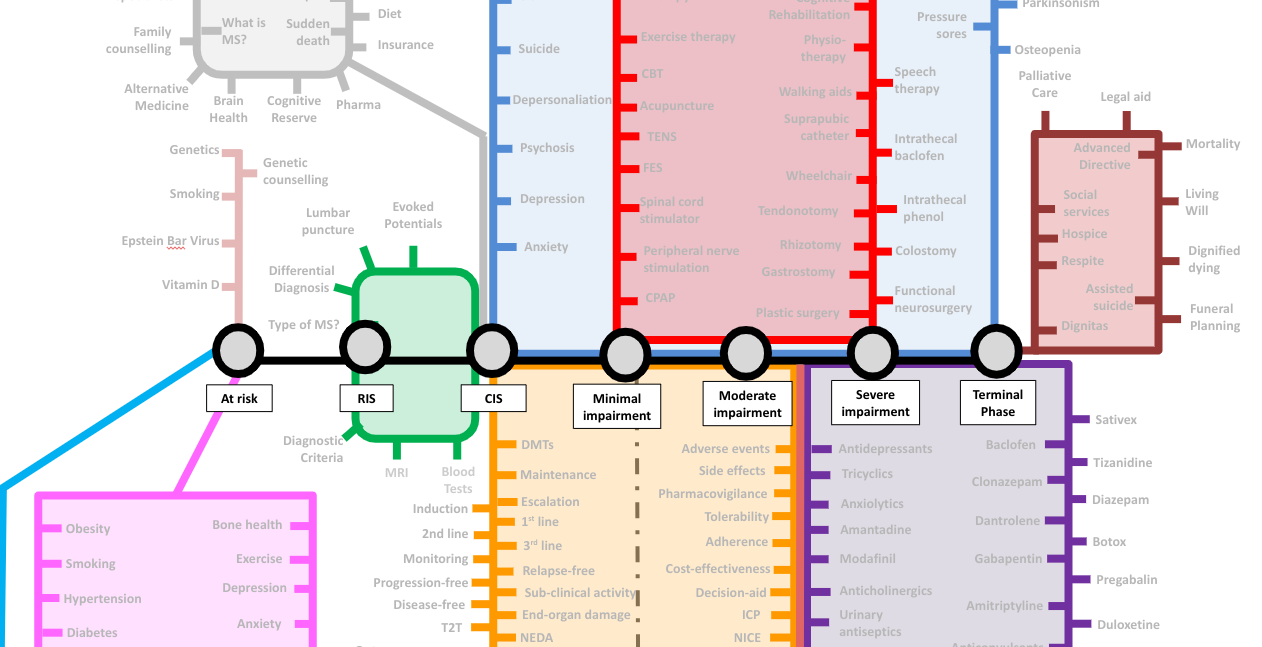
The needs of pwMS change over time. Someone who develops MS typically starts their journey as being at risk of getting MS. They then pass through asymptomatic, prodromal and diagnostic phases. Once diagnosed with MS, they go through the stages of no or minimal disability, moderate disability, severe disability and finally, the terminal stages of having MS. Please note that completing the journey is not inevitable. Many pwMS hop off when treated with high-efficacy DMTs, particularly early on, preventing them from becoming disabled. I have included a dashed grey line that leads to long-term remission and an MS cure. This line is still under construction as we don’t have enough data to claim we can cure MS.
As your needs along the MS journey change, the annual follow-up appointments must reflect this. Some HCPs want to create specific care pathways to manage all the problems pwMS complain about. However, care pathways can fragment MS care. For example, we may refer patients to see their local continence team or refer them to the spasticity clinic to consider a baclofen pump. A different team deals with these problems, and they justify a specific, well-defined care pathway. Having separate care pathways for multiple problems often increases healthcare utilisation and costs. This is why MS teams attempt to deal with most MS-related problems themselves or initially before more specialist input is required.
The following typically needs to be done at the annual follow-up appointment in no particular order:
Is your MS active?
Have you had any relapses in the last 12 months, and has your annual MRI scan shown any new lesions? This is important as it may make you eligible for starting, switching or escalating your disease-modifying therapy (DMT). This section of the follow-up consultation can be difficult if the patient is getting worse, i.e. has smouldering MS or intermittent symptoms that may or may not be due to a relapse.
Smouldering MS is very probably the norm in pwMS if it is looked for with neurological stress tests and more sensitive outcome measures. However, neither of these are part of routine clinical practice. The problem is a lack of evidence on how to manage smouldering MS, i.e. at present, we don’t know if escalating treatment in people with smouldering MS or PIRA (progression independent of relapse activity) makes any difference. This is likely to be the reason why clinicians don’t look for it. This will change in the future once we have treatments targeting smouldering MS.
Retrospective relapse assessments are also difficult. For example, somebody who had new symptoms since their last assessment but didn’t bring it to our attention then, and their symptoms have now resolved. Part of what defines a relapse are changes on examination, and if you can’t find any new clinical signs, it is very difficult to call a possible relapse a relapse. This may not be important if the monitoring MRI shows new lesions as this provides objective evidence of ongoing inflammatory MS disease activity. However, if the MRI shows no changes, an opportunity has been missed to document MS disease activity. Please be aware that about a quarter of relapses, as defined clinically, are not associated with new lesions on MRI. So, this issue is not trivial and occurs far too commonly in my clinical practice.
In the future, when regular blood neurofilament monitoring becomes routine, we may include biochemical evidence of relapse as part of the definition. This will be particularly powerful if we can do remote self-administered NFL measurements. I have predicted that biochemically-defined relapses will become the norm.
Are you stable or getting worse?
In our centre, we are asking patients to self-monitor to get them to engage with their own MS and to save time. We now expect our patients to complete the online web-EDSS, their own timed 25-foot walk and 9-hole peg test, and the online SDMT (symbol digit modality test). Some patients do more than this; for example, they record their walking or running times and produce activity monitoring data. In the future, this is likely to expand to include neurological stress tests and even home sleep monitoring using wearable technology. Most pwMS have a sleep disorder, which contributes to poor brain health and exacerbates fatigue. Getting people with MS to sleep better will improve many other MS symptoms.
Have all your pharmacovigilance and derisking activities been done?
This involves ensuring your blood tests are fine, that you have had your annual vaccines, and, if necessary, screening for malignancies. Please note that the blood tests and procedures required are unique to each class of DMTs; for example, if you are on natalizumab, this will include a 6-monthly JC virus antibody index and potentially a 4-monthly PML monitoring MRI.
Current medications?
Before a detailed symptom review, I like to review a list of current medications. This can be easy if you remember to take a list with you. Often, the medication review forms the basis of the consultation. It is not only the current list that is helpful but also any changes from the last visit and a review of dietary supplements. PwMS are increasingly using supplements on top of their prescribed medications to try and improve their outcome. It is remarkable how often supplements and alternative therapies hijack the annual visit. It is also incredible how many patients attend their follow-up appointments without an up-to-date list of their medications.
Family planning
Where appropriate, I ask patients about their plans to start or extend their families. This is highly relevant as this often interacts with DMTs and medications. This conversation may lead to a discussion about contraception. The family planning detour in itself can take many minutes to complete.
Do you have any symptomatic problems?
This list of symptoms you ask about and apply here depends on where you are on the MS train journey. There is little point in asking about spasticity and falls if a patient is not disabled and runs marathons. I always start with the bladder and bowel function and then proceed to sexual dysfunction. I then ask about mobility, i.e. walking distance, trips and falls. Even if a patient is not falling, they may be at risk of falls and need to be referred to a fall prevention programme and to have their bone health assessed. The latter involves having a DEXA or bone density scan and taking vitamin D supplements (4,000U per day). If you are osteopaenic or osteoporotic, you should also have been prescribed calcium.
I then move on to fatigue, sleep, nocturnal spasms, restless legs and pain. I then bring up the issue of mood and anxiety, which are common problems in pwMS. I always close this section with an open-ended question about other symptoms. On many occasions, I have to deal with symptoms that are not MS-related, for example, joint pain from arthritis. It is incredible how often non-MS-related symptoms are attributed to MS and are left to the MS team to sort out.
Brain Health
I try to address all the issues I have mentioned in the past that can impact brain health, including exercise, diet, comorbidities and other lifestyle factors such as alcohol, smoking and other substances and HRT (hormone replacement therapy). In an ideal world, I would love to be able to screen my patients for hypertension and the state of their metabolic health, but I don’t have time for this, and the management of these problems needs to be done by the general practitioner. It is pretty depressing that many of my patients who have comorbid hypertension or diabetes are not as engaged with managing their comorbidities as much as their MS. If you have hypertension or diabetes, you need to self-monitor your blood pressure and blood sugars and feedback the information to your GP.
Social Health and the Social Determinants of Health
More recently, I have started addressing modifiable social determinants of health. This includes questions about work, whether patients come out each month financially, loneliness and social isolation. We focus on social issues because we can now refer, or ask the GP to refer, patients for help using social prescribing, or we can simply sign-post people to community services.
Cognition
I don’t specifically ask about cognition because self-reporting cognitive problems is often unhelpful. I am unsure if you know that pwMS who complain of cognitive problems are more likely to be depressed and anxious than have significant cognitive impairment. I prefer to pick up clues from the consultation that cognition is an issue and try to deal with the consequences as best I can. For example, an occupational health assessment may be the most appropriate action if someone is not coping at work. Now that we are monitoring cognition with the online SDMT, it is noteworthy that some people with relatively low scores still manage very well at work. Therefore, bringing up cognitive issues in high-functioning patients is not necessarily appropriate.
Activities of Daily Living
In patients who are disabled, it is essential to ask about activities of daily living. Are they managing their self-care? Can they wash and dress themselves? Brush their teeth? What is the state of the oral hygiene? Do they have caries or gum disease that needs attention? Who is looking after their feet? Can they cut their toenails? Do they need a referral to a podiatrist? Can they wash, dry and brush their hair? Can they transfer themselves from the bed to the wheelchair and then to the toilet? If they are battling, do they have the necessary home adaptations? In almost every clinic, one or two of my patients must be seen by the community-based disability team because of these problems.
Social Care
For some patients, we need to address other social issues, i.e. Is the care package sufficient, and are they managing to get everything done when their carers come in? Sometimes, their carers are on such a tight schedule that they can’t even wait for their clients to complete a meal. This may result in a truncated feeding time. I have had rare patients who became malnourished as a result.
Bulbar function
Bulbar function refers to the functioning of structure innervated by nerves from the lower half of the brainstem (pons and medulla). In pwMS, who are more disabled, I always ask about swallowing problems and choking episodes. This frequently prompts a referral for a speech and language assessment. Similarly, if their speech is affected, they may need help with a communication aid.
Advanced Directives
In addition to the above, I often remind pwMS of the need to complete an advanced directive (a form or a living will). This needs to be done early in your disease when you have insight and can discuss the issues with your partner and family. Waiting until you have advanced MS is too late for an advanced directive.
Question time and trials
On top of the above, we are expected to give patients time to ask questions. This usually prompts questions about MS research and clinical trials. Discussing clinical trials takes time.
Would you be able to do all of the above in 15 minutes? No, which is why we often limit the consultation to a few big-ticket items. I am a big fan of asynchronous consultations using email or a portal that automates some of the above. This is why pwMS need to be more proactive about managing their MS.
The MS-Selfie Challenge
Please note that I have covered almost every issue above in earlier newsletters and podcasts. Despite this, I suspect some topics still need to be covered in more detail. This will happen over time, and the information will gradually be transferred to an MS-Selfie microsite and eventually end up in an MS-Selfie Self-Management guide.
Please keep in mind that this section on what needs to be done with scheduled follow-up assessments can never be comprehensive but is written to provide an overview of my attempt to manage MS holistically.
Have I missed anything that you think needs to be covered in your scheduled follow-up appointments? Please note I have written previously on this subject and the subject of preparing for your annual follow-up appointment, using ‘My MS Piorities’ and ‘Your MS Questionnaire’. This advice still holds (see ‘What are your priorities in relation to 'Your MS'?’; 4-Oct-2021).
Providing factual information like this can be tedious, so I prefer using case studies to teach MS self-management strategies. I suspect some of you will disagree with me on this.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
X (Twitter) / LinkedIn / Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.














Share this post