I attended a meeting last week where a KOL (key opinion leader) in the field of multiple sclerosis (MS) made the point that relapses and focal MRI activity (Gd-enhancing and new or enlarging T2 lesions) are MS, i.e. they are the disease and that suppressing relapses and MRI activity is what we aim to achieve with our disease-modifying therapies (DMTs). Do you agree?
I have spent the better part of a decade coming to the opposite conclusion that relapses and focal MRI activity are not the disease. They represent the immune system’s response to what is causing MS and that the real MS is smouldering MS.
If relapses and focal MRI activity were MS, then:
Baseline relapse rates and MRI activity should be predictive of outcome
Changes in disease activity over time are predictive of outcome
Changes in disease activity due to DMTs should predict the outcome
These three criteria are called the Prentice criteria and are philosophical approaches to defining a surrogate outcome measure. Unfortunately, relapses and focal MRI activity don’t fulfil the Prentice criteria; therefore, they can’t be the disease by definition.
1. Baseline relapse rates and MRI activity should be predictive of outcome
In relapse-onset MS, the relapse rate and MRI activity in the first 2-5 years do predict the outcome. However, this does not hold up for people with primary progressive MS (pwPPMS). It could be argued that people with pwPPMS have had the disease longer by the time they present and get diagnosed; hence, the rule still holds that early activity is the disease and predicts the outcome. Unfortunately, we don’t have long-term follow-up data on very early PPMS or RIS-PPMS.
2. Changes in disease activity over time are predictive of outcome
Outside the initial 5-year window, the data on relapse rates and MRI activity predicting clinical outcomes is weak. This is one of the paradoxes in the field of MS and has been referred to in the past as the MRI-clinical paradox. If MRI activity was MS, it should predict the outcome regardless of where you are in the course of the disease.
3. Changes in disease activity due to DMTs should predict the outcome
This is where evidence against MS disease activity being MS is most substantial. It is clear from clinical trials that if you are on a DMT, then MS disease activity on therapy is a poor prognostic sign. However, the outcome is not predicted if you are on a placebo or no treatment. If MS is focal inflammatory disease activity, then it should predict outcome regardless of what treatment you are on. From a philosophical perspective, this point is critical and tells us that focal inflammation (relapses and MRI activity) cannot be MS. It is remarkable how many people don’t appreciate this point and ignore it.
Here are some examples to illustrate this point.
Ocrelizumab exposure
The observation that pwMS with increasing ocrelizumab exposure do better despite a ceiling effect on relapses and MRI activity tells us that something is happening beyond focal inflammation. It has been shown that following the administration of ocrelizumab 600 mg every 6 months, serum concentrations of the drug are higher among subjects weighing <60 kg and lower among subjects weighing >90 kg, compared to subjects weighing 60-90 kg. This dose effect can be seen in levels of B-cell depletion but is not reflected in the reduction of relapses or focal lesions on MRI, as all levels of ocrelizumab exposures were associated with almost complete suppression of focal inflammatory disease activity. However, a dose effect is observed, with more significant prevention of disability progression in people with both relapsing and PPMS with higher levels of peripheral B-cell depletion.
This tells us that there is a disconnect between the pathological processes driving focal inflammation and those responsible for non-relapsing disability progression or smouldering MS. Based on these observations, we are now testing high-dose ocrelizumab (1200 mg or 1800 mg vs. 600 mg every 6 months) in two clinical trials (ClinicalTrials.gov Identifiers: NCT04117529 and NCT04548999). The hypothesis is that higher ocrelizumab exposure can target peripheral deep-tissue B-cells and CNS-resident B-cells, which drive smouldering MS beyond focal inflammatory events.
Ofatumumab vs. Teriflunomide
Ofatumumab, a fully humanised monoclonal anti-CD20 therapy, is superior to teriflunomide in suppressing relapses and focal inflammatory MRI activity but is no better than teriflunomide at slowing the rate of brain atrophy over 2 years. Despite its relatively modest impact on focal inflammation, teriflunomide’s effect on end-organ damage or smouldering MS is the same as that of ofatumumab.
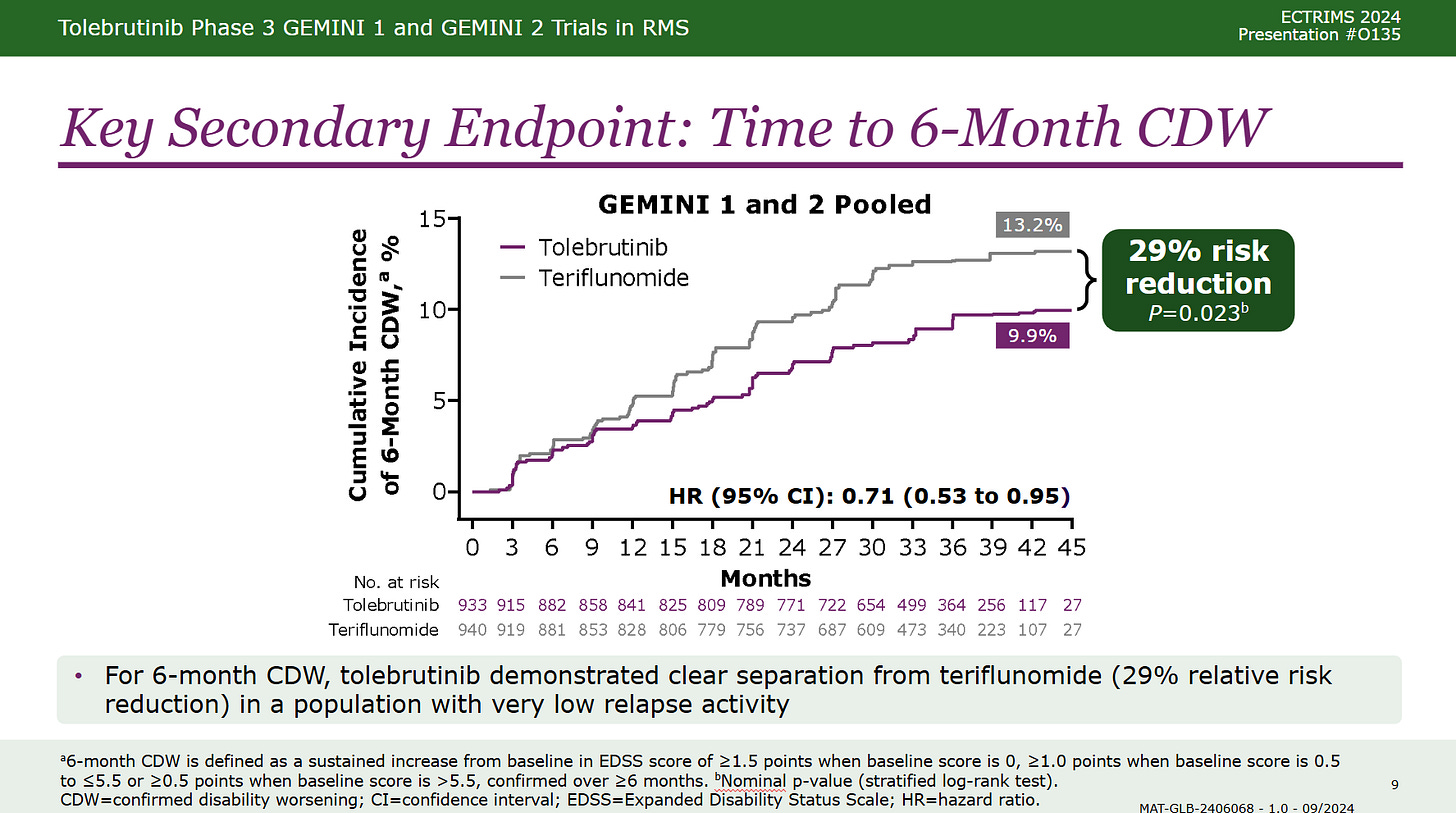
Tolebrutinib vs. Teriflunomide or Placebo
More recently are the lessons from the Tolebrutinib phase 3 trials. Tolebrutinib is a second-generation BTK inhibitor (BTKi) with a dual mode of action. It inhibits BTK in B-cells and is an anti-inflammatory therapy. In both the relapsing and non-relapsing progressive MS trials, it had a relatively modest impact on relapses and focal MRI activity. In the relapsing trials (Gemini 1 & 2), tolebrutinib was not superior to teriflunomide in suppressing relapse activity, i.e. the relapse rates were similar, and it was inferior to teriflunomide in suppressing Gd-enhancing lesions.
Teriflunomide was superior to tolebrutinib in suppressing Gd-enhancing lesions but had a similar effect on new T2 lesions. This could be referred to as a Gd-enhancing-T1/T2-lesion paradox, implying that new Gd-enhancing lesions are less likely to form chronic T2 lesions in subjects treated with tolebrutinib. This indicates that tolebrutinib is changing the biology of how MS lesions evolve; i.e. it is doing something to the acute Gd-enhancing lesions that makes it less likely to leave a scar or new T2 lesion. Based on these preliminary observations, I suspect that in addition to fewer T2 lesions, tolebrutinib will also suppress the development of paramagnetic rim (PRLs) and slowly expanding lesions (SELs), both associated with worse MS outcomes.
However, despite being inferior to teriflunomide in suppressing focal inflammatory activity, tolebrutinib was superior to it when it came to disability progression., i.e. it has an impact on smouldering MS-associated worsening (SAW) but not relapses.
Tolebrutinib, therefore, dissociates relapses from disability progression and ‘proves’, yes proves, that these two processes are likely to be independent of each other with the caveat that relapses can be associated with some disability progression called relapse-associated worsening or RAW.
This treatment effect on smouldering MS was seen in the relapsing (Gemini 1&2 trials) and non-relapsing SPMS trials (Hercules trial). Subjects in the Hercules trial were also more likely to have significant disability improvement, with a trend in the relapsing or Gemini trials. The disability improvement data is critical and tells us that something is happening centrally to promote recovery of function in subjects on tolebrutinib.
Based on these observations, I don’t know how anyone can claim that focal MS disease activity is MS. My interpretation is that focal MRI activity is simply the immune system’s response to the cause of the disease. The real MS is in the tissue against which the immune system may or may not react. I call this the field hypothesis of MS.
The field hypothesis
If you have an MS relapse or attack in one particular area of the brain or spinal cord, you are more likely to have subsequent attacks in this area. Something locally in a specific anatomical area triggers recurrent attacks in the same site.
What underlies the field effect? One explanation is that the area damaged by the initial attack is more likely to trigger autoimmune responses in the future due to the local up-regulation of so-called second, or danger, signals. The latter occurs in response to the factor produced as part of the initial inflammatory event. For T-cells to become activated, they need an antigen-specific signal via the T-cell receptor and an additional signal via co-stimulation.
The obvious question is what triggers relapses in the field or CNS. Possibly a virus, like an isolated seed or flower in a wheat field? Why do I say this? Firstly, when pwMS were treated with interferon-gamma, a cytokine that stimulates immune responses, they relapsed. The interesting thing about these interferon-gamma-induced relapses is that they occurred in sites previously affected by MS. When I discussed this observation with the late Hillel Panitch, who was the principal investigator on the gamma-interferon trial, he thought that this observation was fundamental and was telling us something important about MS.
Another observation that supports the abnormal field hypothesis is the rebound post-natalizumab. This suggests that whilst you keep T and B cells out of the nervous system with natalizumab, the field (brain and spinal cord) becomes more abnormal. When you let these cells back in, they detect the abnormal field and run amok, trying to clear the field of the offending agent. This happens with IRIS (immune reconstitution inflammatory syndrome) and PML. When natalizumab is washed out, the immune system finds the JC virus and tries to clear it by initiating an inflammatory process. Some of us think that rebound post-natalizumab is a form of IRIS in response to the virus that causes MS.
Another observation comes from serial MRI studies showing subtle changes in the normal-appearing white matter many weeks or months before a gadolinium-enhancing lesion appears. This suggests that the primary pathology in the nervous system takes weeks or months to trigger a focal inflammatory lesion. The challenge for us all is to find out what this field abnormality is. The best chance we have of doing this is to study the brains of pwMS on natalizumab. To do this, we will need someone with MS to die whilst on natalizumab treatment and to donate their brain to a unit with the necessary techniques to look for viruses. The viral load is likely to be higher in the absence of inflammation. This is why it is so crucial for pwMS to donate their brains for medical research.
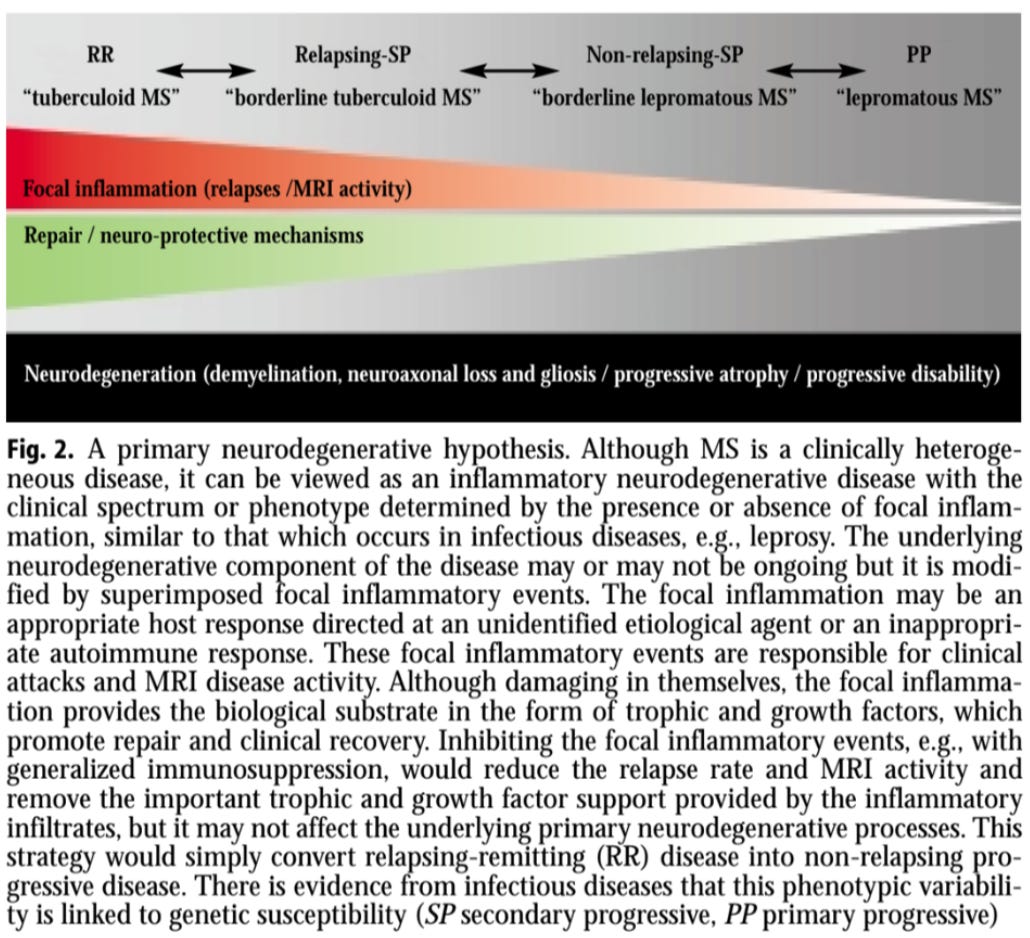
MS clinical phenotype is determined by the immune response
I have argued that MS is one disease, not two, three, or four, and the immune response to the cause determines the clinical phenotype. Inflammation-driven clinical phenotypes are not a new concept and have been well-studied in infectious diseases such as leprosy, TB, hepatitis B, and leishmaniasis… This is why I often use the leprosy analogy when I refer to MS.
Leprosy is an infectious disease caused by a bacterium with a well-defined set of antigens that can be used to interrogate the adaptive immune systems’ responses to antigens. Depending on the immune response, you get a different clinical picture. If you have a brisk inflammatory response, you get tuberculoid leprosy, which presents with inflamed lesions. On the other side of the spectrum, you get lepromatous leprosy, which is more of a smouldering disease with low-grade inflammation. Between these two extremes, you get a grey zone called borderline subtypes. Interestingly, people can convert from having lepromatous to tuberculoid leprosy if they shift their immune response to a so-called type 1 immune response driven by interferon-gamma. The following is a diagram I drew over 20 years ago describing this hypothesis.
Primary progressive MS is lepromatous MS, and relapsing-remitting MS is tuberculoid MS. SPMS is in the middle and is borderline MS. Interestingly, gamma interferon seems to have the same effect on MS as on leprosy, driving lepromatous MS (PPMS) to become tuberculoid or relapsing MS.
The only way to prove the leprosy theory of MS is to have the organism that causes MS in hand and study the immune response to the agent using immunological techniques applied to leprosy.
Conclusions
I know many of the issues discussed above are repetitions, but the concepts, which I think are relatively straightforward, don’t seem to be getting through. When a colleague says that relapses and MRI activity are MS, my heart sinks. Do these concepts make sense to you?
If you need hard-core science, I suggest you read our two papers on smouldering MS below.
Paper 1 - relapses tend to occur in the same site
BACKGROUND AND PURPOSE: MS is a chronic inflammatory disorder of the central nervous system characterized by acute episodes of neurological dysfunction thought to reflect focal areas of demyelination occurring in clinically eloquent areas. These symptomatic relapses are generally considered to be random clinical events occurring without discernible pattern. The hypothesis that relapses may follow a predetermined sequence and may provide insights into underlying pathological processes was investigated.
METHODS: Employing prospective clinical database data from 1482 MSers who had experienced one or more consecutive relapses were analysed. Using regression analysis, site and symptom of index event were compared with those of first relapse.
RESULTS: It is demonstrated that following disease ignition subsequent relapses may not be random events but dependent on characteristics of the index event. All anatomical sites were more likely to be affected in the first relapse if that site had been involved in the index event with a similar association observed when comparing by symptoms.
CONCLUSION: These findings have importance in understanding the evolution of the disease and predicting individual disease progression and may aid with patient counselling and management.
Paper 2 - International consensus on smouldering MS
Despite therapeutic suppression of relapses, multiple sclerosis (MS) patients often experience subtle deterioration, which extends beyond the definition of "progression independent of relapsing activity." We propose the concept of smouldering-associated-worsening (SAW), encompassing physical and cognitive symptoms, resulting from smouldering pathological processes, which remain unmet therapeutic targets. We provide a consensus-based framework of possible pathological substrates and manifestations of smouldering MS, and we discuss clinical, radiological, and serum/cerebrospinal fluid biomarkers for potentially monitoring SAW. Finally, we share considerations for optimizing disease surveillance and implications for clinical trials to promote the integration of smouldering MS into routine practice and future research efforts.
Paper 3 - Smouldering MS, the ‘Real MS’
Using a philosophical approach or deductive reasoning, we challenge the dominant clinico-radiological worldview that defines multiple sclerosis (MS) as a focal inflammatory disease of the central nervous system (CNS). We provide a range of evidence to argue that the 'real MS' is in fact driven primarily by a smouldering pathological disease process. In natural history studies and clinical trials, relapses and focal activity revealed by magnetic resonance imaging (MRI) in MS patients on placebo or on disease-modifying therapies (DMTs) were found to be poor predictors of long-term disease evolution and were dissociated from disability outcomes. In addition, the progressive accumulation of disability in MS can occur independently of relapse activity from early in the disease course. This scenario is underpinned by a more diffuse smouldering pathological process that may affect the entire CNS. Many putative pathological drivers of smouldering MS can be potentially modified by specific therapeutic strategies, an approach that may have major implications for the management of MS patients. We hypothesise that therapeutically targeting a state of 'no evident inflammatory disease activity' (NEIDA) cannot sufficiently prevent disability accumulation in MS, meaning that treatment should also focus on other brain and spinal cord pathological processes contributing to the slow loss of neurological function. This should also be complemented with a holistic approach to the management of other systemic disease processes that have been shown to worsen MS outcomes.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
BlueSky Social / LinkedIn / Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.














Share this post