Reflections of an ageing MS expert
Innovation and the resultant changes from its adoption always seem slow when you judge them year to year. But not so when you look back over a decade or more.
Shortly after I arrived in London in 1993, the pivotal interferon-beta-1b relapsing-remitting MS trial results were announced; the rest is history. Interferon-beta was not the first therapy to be shown to modify the course of multiple sclerosis (MS), but it became the first licensed treatment, which changed everything.
The reception of the interferon-beta was a muted affair, at least from a UK perspective. Senior academics questioned its value and felt spending the money on physiotherapists would be a better use of scarce NHS resources. One senior academic was even concerned that interferon-beta would affect ongoing MS natural history studies. Yes, the mid-nineties and naughties were extraordinary times with MS experts pitted against the neurology establishment that thought MS therapies were not good value for money. Sadly MS neurology in the UK still has a reputation for being ultraconservative and resistant to change.
What is happening in MS seems to be playing out in the field of Alzheimer’s disease (AD). Since the FDA licensed lecanemab (Leqembi) for early AD (FDA, 6-July-2023), the naysayers are already saying it is too expensive and the effects too small to justify its use. I'm afraid I have to disagree! We should be celebrating the fact that we now have effective therapies for AD. As with MS, lecanemab will usher in the beginning of a golden age in the treatment and, hopefully, the prevention of dementia.
Interferon-beta catalysed a remarkable era in the treatment of MS. The clinical course of MS has been transformed beyond recognition. Trainees working in the field of MS don’t see what I have seen. When I was a senior registrar, we always had several inpatients with MS. These patients were in the hospital to manage a relapse, to have a diagnostic work-up, or to sort out complications of having MS, for example, managing pressure sores. Nowadays, it is uncommon to have a patient with MS on the neurology wards because our current DMTs are so effective at managing the disease, and we have excellent management pathways designed to keep patients out of the hospital.
The commonest reason for someone with MS to be in the hospital is that their initial presentation, typically a brainstem or spinal cord attack, requires admission for a diagnostic work-up and treatment. Interestingly many of these patients come via our stroke pathway. The other common reasons for pwMS to be admitted are those with more advanced MS who come via A&E due to MS-related complications, for example, urinary tract or lower respiratory tract infections, falls with fractures and head injuries, faecal impaction, pressure sores and attempted suicides. These are all grim but are becoming less common with the wider adoption of treating MS early and effectively and using higher-efficacy DMTs first-line.
Off-label DMTs
Some good news. In 2014 I took a 6-month sabbatical and travelled the world to see how MS was managed globally. I visited MS centres in the US, Canada, Europe, Australia, South America, India and South Africa. It was India and South Africa that shocked me the most. Unless you were wealthy and had private healthcare insurance, your MS was essentially left to run its natural course. This prompted me to start what I called an essential off-label DMT list. The list consisted of drugs that were not licensed to treat MS but had a sufficient evidence base to give neurologists the confidence that they would work. And combing these therapies with a treat-2-target approach of no evident inflammatory disease activity, most pwMS in resource-poor environments could have their managed relatively effectively.
Prof G’s Essential Off-label DMT list
Azathioprine
Cladribine
Cyclophosphamide
Fludarabine
Leflunomide
Methotrexate
Mitoxantrone
Rituximab
AHSCT
Did the essential off-label DMT list change things? Almost certainly. When I visited India earlier this year, one of the leading MS neurologists thanked me for nudging the Indian neurologists to start using off-label rituximab. In 2014, less than 2% of pwMS in India were on DMTs. At the 2023 MS meeting in Mumbai, I was told that the figure was now around 30%.
In 2015 the MSIF (Multiple Sclerosis International Federation) asked me to present the rationale behind my essential off-label DMT list to their members at their annual meeting in London. The presentation went down well and dove-tailed with the MSIF’s campaign for improving access to MS DMTs worldwide. This subsequently led to the MSIF Off-Label Treatments (MOLT) initiative and two submissions to the WHO to get MS DMTs onto the WHO List of Essential Medicines.
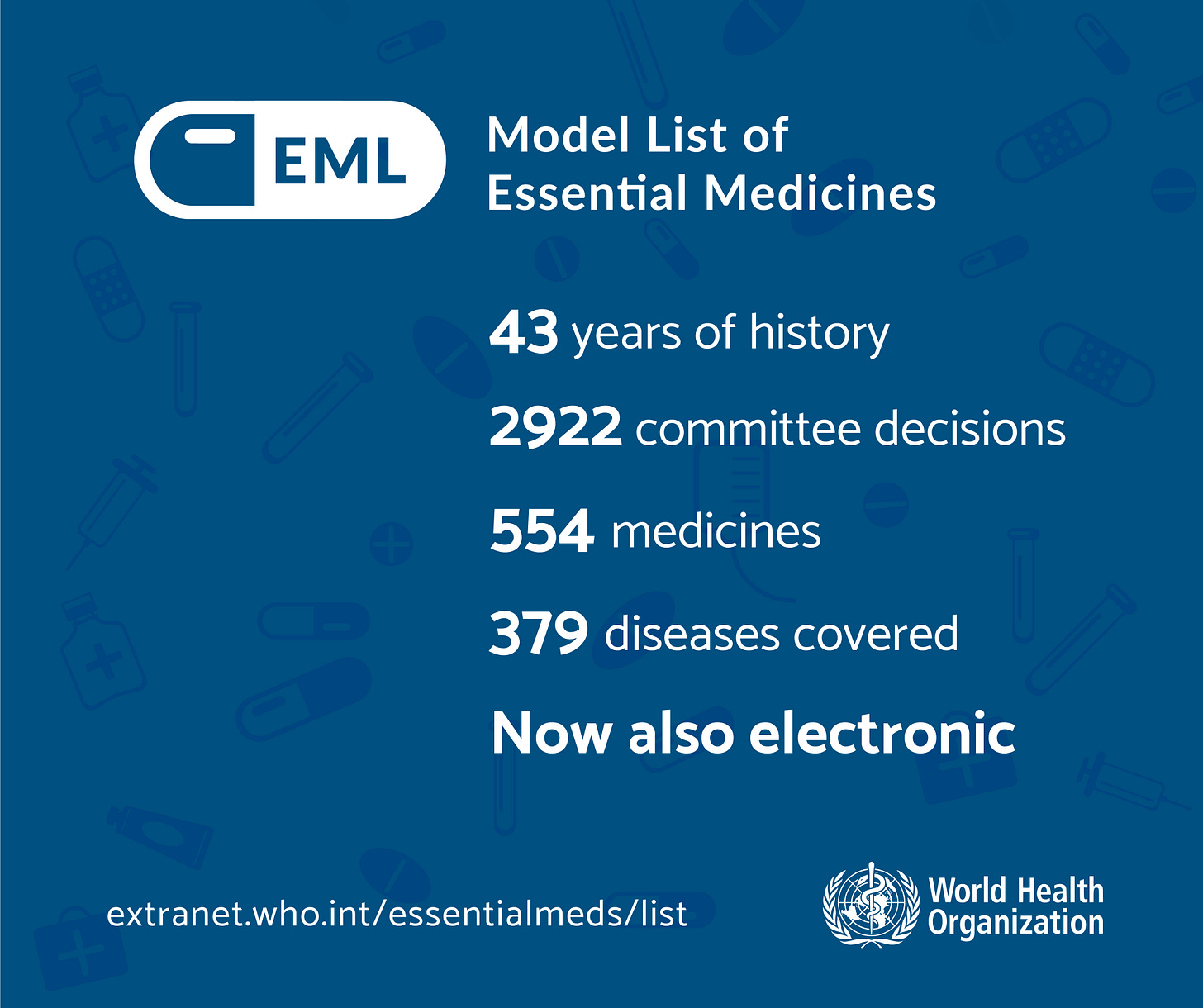
The first submission failed, which included glatiramer acetate, fingolimod, and ocrelizumab (see paper one below). It failed because we were given the wrong advice and didn’t consider the cost. However, we were not disheartened, and the MSIF resubmitted a much more considered application last year that included cladribine, glatiramer acetate and rituximab. The good news is that the WHO green-lighted these three drugs last week, and they are now on the EML for treating MS.
PRESS RELEASE: “WHO endorses landmark public health decisions on Essential Medicines for Multiple Sclerosis” (26-July-2023)
As a result of my accident in November 2020 and the need for rehabilitation, I had to resign from the MOLT group and the Cochrane review panel of rituximab. I, therefore, didn’t play an active role in this submission. However, I can’t stress how important this decision to include three drugs in the WHO’s EML is for the global MS community.
Firstly, the WHO now acknowledges that MS and its treatment is a problem at a global level. Secondly, low- and low-middle-income countries will now have to recognise that MS is a treatable condition, and they will hopefully be forced to include the diagnosis and management of MS as part of their healthcare plans. We could argue about the merits of the three DMTs on the list. However, there is a good rationale behind each one.
Glatiramer acetate (GA) was chosen because of its safety profile, no need for monitoring and good track record during pregnancy. The problem with GA is that it is a complex therapy with high manufacturing requirements; for example, each batch should ideally be tested in animals, so generic or biosimilar GA is not cheap. A cold chain must also be maintained, which may make GA’s storage and distribution problematic in certain healthcare environments.
Cladribine was chosen because it is a tablet, it has a good safety profile, has low monitoring requirements and the fact that it is an IRT (immune reconstitution therapy) and is given as short courses with the majority of treated patients going into long-term remission. I am aware that a patent still protects oral cladribine, but when the patent expires, being a small molecule, the price will plummet. In the interim, the parenteral formulation can be used IV or subcutaneously, or it can even be taken orally as is done for oncology (Karlsson et al. Br J Haematol. 2002 Mar;116(3):538-48.).
I suspect rituximab will prove the most controversial MS DMT on the WHO’s EML. Although widely used, we still don’t know the optimal dose. For more information on the dosing of anti-CD20 therapies, please my MS-Selfie Newsletter “Are we ready for adaptive ocrelizumab dosing?” (02-Jan-2022) and “Should I switch from ocrelizumab to ofatumumab?” (18-April-2023). Rituximab also requires a cold chain and many healthcare logistics to deliver. There is also the issue around anti-drug antibodies (ADAs); assays for ADAs are difficult to access in resource-poor settings. Finally, rituximab is a biological therapy with relatively high costs. Even in India, where rituximab is now widely adopted as a treatment for MS, the costs are a hurdle for many pwMS starting on treatment. Hopefully, once ocrelizumab comes off-patent and biosimilars enter the market, the WHO will have the sense to replace rituximab with ocrelizumab. The evidence base for ocrelizumab for relapsing and primary progressive MS is superior to rituximab. ADAs are much less of a problem on ocrelizumab, and the effective dose of ocrelizumab is relatively well established.
MS stakeholders in resource-poor environments can now use the WHO’s EML to demand better care for pwMS. This is why we as an MS community should celebrate the news and thank the MSIF for all its hard work in getting MS on the WHO’s agenda. Do you agree?
Paper 1 - WHO rejection
Introduction: The World Health Organization (WHO) publishes a biennial Essential Medicines List (EML) to assist governments in low-resource settings to prioritize their spending on medicines. Currently, no medicines on the EML have a multiple sclerosis (MS) indication. Multiple Sclerosis International Federation (MSIF) prepared an application for inclusion of MS disease-modifying therapies (DMTs) for the 2019 EML together with the regional Committees for Treatment and Research in Multiple Sclerosis (TRIMS) and the World Federation of Neurology.
Rationale: The MSIF taskforce categorized 15 DMTs according to their efficacy and risk profiles to ensure the ability to treat as many different clinical scenarios as possible. Three DMTs were selected: glatiramer acetate, fingolimod, and ocrelizumab.
Outcome: The WHO Expert Committee did not recommend the addition of any of the DMTs to the EML. They acknowledged the public health burden of MS, the need for effective and affordable MS medications, and the high volume of letters received in support of the application but requested a revised application.
Discussion: Despite the negative outcome, the repeated recognition of MS as a global public health burden is sending a powerful message to governments globally that a range of affordable and good quality medications need to be available to health systems and people affected by MS.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your own healthcare professional, who will be able to help you.