If you have MS and have been treated with an immunosuppressive disease-modifying therapy (DMT), was HPV (human papillomavirus) infection and/or vaccination discussed with you before starting the DMT?
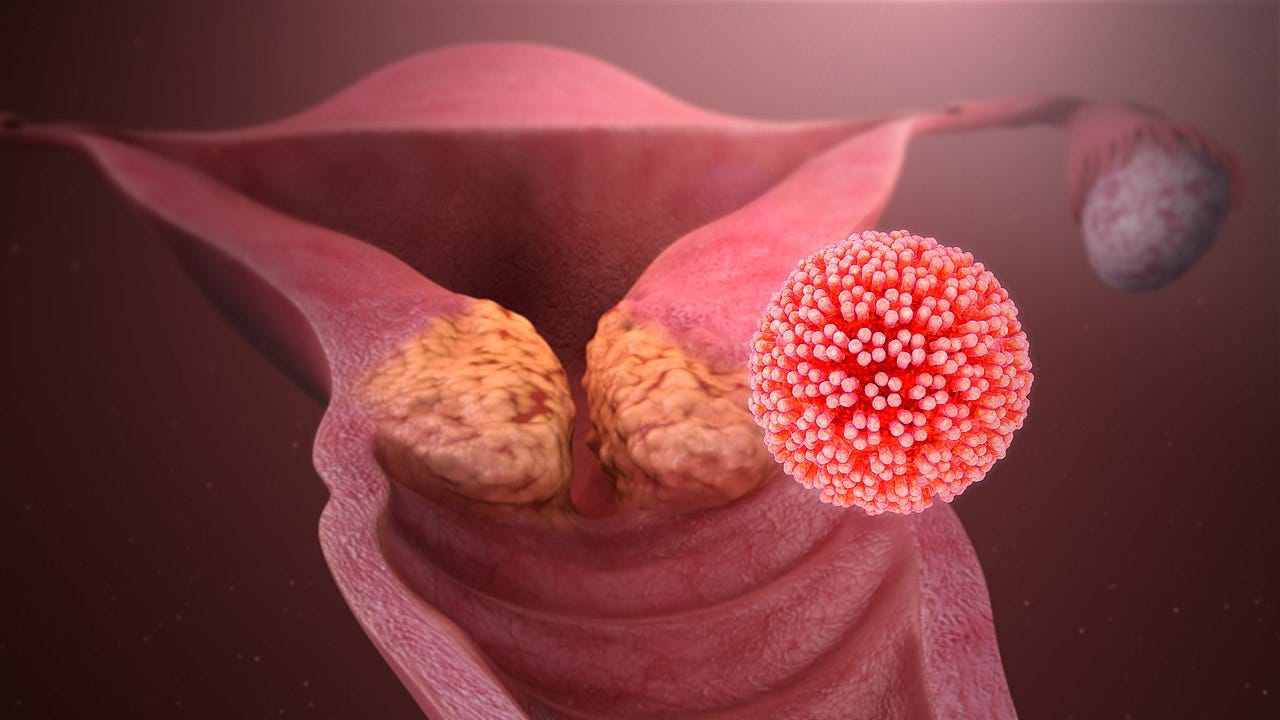
Before we start female patients on an immunosuppressive DMT, we check to see if they had a recent cervical smear or vaginal swab PCR to exclude active HPV (human papillomavirus) infection. This is to prevent them from developing CIN (cervical intraepithelial neoplasia) and cervical cancer. As I write this, I realise we are not extending this concern to men. Yes, men who have sex with men and anal sex are at risk of developing HPV-associated anal and penile cancer. Should we be asking them to have anal HPV screening? A quick search shows there is currently no approved test for HPV in men nor a national screening programme. However, several private sexual health clinics offer this service to men.
What happens after initiating immunosuppressive therapy? Unless in a clinical trial, we leave it up to the patient and general practitioners to make sure women continue to have regular HPV screening. The problem is that this may not be enough, as the adherence rates with repeated cervical screening are poor. I am not surprised, as women find the procedure of having a cervical smear unpleasant. If you are one of these women, please take note of the Australian study below that shows women with MS on moderate-to-high efficacy DMTs are 3.8x more likely to have a cervical abnormality detected on cervical screening tests than women not exposed to moderate-to-high efficacy DMTs.
The message is clear that chronic immunosuppression increases your risk of chronic HPV infection and, hence, your risk of developing CIN and cervical cancer. I assume this risk will apply to the other HPV-associated cancers that we are currently not screened for, i.e. anal, oropharyngeal, oesophageal, penile and vulvar cancer.
Is there anything else that can be done about HPV?
Yes, vaccination.
I counsel all my patients on HPV vaccination. Since September 2008, the HPV vaccine has been offered to all girls in school year 8 (12-13 years). From September 2019, it has also been offered to year eight boys. The uptake of the HPV vaccine has dropped significantly and is currently at ~80%. This means 1 in 5 eligible people for the vaccine are unvaccinated.
If you missed your vaccination at school, try to get it as soon as possible. Contact your GP practice to arrange an appointment. In the UK, you can receive the HPV vaccine on the NHS until your 25th birthday.
However, things have changed since the initial rollout of the school HPV vaccination programme, which uses the quadrivalent vaccine Gardasil-4. We now have the polyvalent or Gardasil-9 vaccine, which covers most of the cancer-causing strains of the virus (>95%) compared to only about 67% protection with the older vaccine. If I have been vaccinated with the older quadrivalent vaccine, you can extend your coverage by receiving Gardasil-9. However, you would need to do this privately.
Even if you are already on an immunosuppressive DMT, it is worth considering upgrading or having the HPV vaccine. I say this because there has been a surge in older women getting cervical cancer from being exposed to HPV in later life. This is because sexual mores have changed, and older women are now more likely to have multiple sexual partners and unprotected sex than in the past, both risk factors for HPV infection. Dating apps are driving this behaviour change and have been linked to a mini epidemic of sexually transmitted diseases in older people.
The UK has moved to a single-dose schedule for the routine adolescent and men who have sex with men programme who come forward before their 25th birthday and a two-dose schedule for people between 25 and 45. However, for those over 45 and immunosuppressed individuals, a three-dose schedule is recommended.
For the two-dose schedule, the second dose should ideally be given 6-24 months after the initial dose. For the three-dose schedule, the second dose must be given at least a month after the initial dose and the third between 6 and 12 months.
For more detailed information, please see Chapter 18a in the green book on human papillomavirus (HPV).
Should I delay starting DMTs to have the vaccine?
There is no simple answer to this question. You have to balance the risks and benefits of having the vaccine against the risks of under-treated or untreated MS. If you are starting an immune reconstitution therapy (IRT), i.e. cladribine, alemtuzumab or AHSCT, I would suggest going ahead and starting the IRT and delaying the vaccine until you have reconstituted your immune system. Delaying starting an IRT to have the vaccine does not make immunological sense in that the memory responses you have just made to the vaccine could get depleted and, depending on the intensity of the immunodepletion, may not recover. For maintenance DMTs, particularly the S1P modulators, fumarates, and anti-CD20s, you should delay starting treatment to get the vaccine or at least the first two doses. Booster vaccine responses have been shown to occur whilst on these therapies. Please note that these vaccine studies have tended to look only at antibody responses and not T-cell responses. It is now clear that even if you don’t mount a good antibody response to, for example, the COVID-19 vaccines on anti-CD20 therapies (rituximab, ocrelizumab, ofatumumab, ublituximab), you still have detectable T-cell responses.
To get an idea of the awareness of HPV infection and vaccination and MS DMTs, I would appreciate it if you could complete this short survey. It will take less than 5 minutes to complete, and the information will let us know if we need to take a more proactive approach to this topic. Thanks.
Other cancer screening
Please be aware that the UK has two other routine cancer screening programmes: bowel and breast cancer screening. The screening programme for prostate cancer was stopped in the UK because the PSA test is not reliable enough. However, men over 50 can request a PSA test via their GP. Depending on individual risk factors, including genetic risks, you may be eligible for lung, skin, ovarian, and other cancer screening in some parts of the UK.
If any issues this newsletter raises are relevant, please share your thoughts. Thank you.
Paper
Background and objectives: The impact of immunomodulatory therapies on the risk of cervical pre-cancer and invasive cancer development is important for the health and safety of women with multiple sclerosis (wwMS). We investigate the risk of cervical abnormalities in wwMS treated with disease-modifying therapies (DMTs).
Methods: This is a multicenter cohort study with data collected from 1998 to 2019 in Victoria, Australia. Data linkage was performed using matching records from the MSBase Registry, the National Human Papillomavirus (HPV) Vaccination Program Register, and the Victorian Cervical Cytology Register. The primary outcome was the detection of any type of cervical abnormality as determined by cytology or histology. Survival methods were used to assess the time to cervical abnormality detection on cervical screening tests (CSTs). Crude and adjusted Cox proportional hazards models were used to determine time to and magnitude of association of DMTs with the risk of cervical abnormality. In a sensitivity analysis, we constructed standardized survival curves averaged over the same set of covariates to determine the commensurate population-average (marginal) causal effects.
Results: We included 248 wwMS. The incidence of abnormal CSTs was lower (p < 0.001) for women not exposed to moderate-high-efficacy therapy (10.2 per 1,000 patient-years [95% confidence interval (CI) 5.5-14.9]), compared with those exposed (36.6 per 1,000 patient-years [95% CI 21.7-51.6]). Exposure to higher efficacy treatment was associated with a 3.79-fold increased hazard (95% CI 2.02-7.08, p < 0.001) of developing a cervical abnormality relative to those not exposed. When adjusted for vaccination status, smoking, hormonal contraceptive use, and socioeconomic status, the risk remained elevated at 3.79 (95% CI 1.99-7.21, p < 0.001). Marginal hazard ratios declined over time, ranging from 3.90 (95% CI 2.09-7.27) at 20 years of age to 2.06 (95% CI 1.14-3.73) at 70 years of age.
Discussion: A greater than three-and-a-half-fold increased risk of cervical abnormalities was found after exposure to moderate-high-efficacy DMTs. This risk persisted despite adjusting for HPV vaccination status, hormonal contraception use, smoking, and socioeconomic status. If confirmed in future studies, we would advocate for wwMS exposed to moderate-high-efficacy DMTs to be treated in line with immune-deficient paradigm in cervical screening and HPV vaccination programs.
Classification of evidence: This study provides Class III evidence that highly active MS therapy compared with less active therapy increases the risk of developing cervical abnormalities among women with MS.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
X (Twitter) / LinkedIn / Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.














Share this post