I spend a large chunk of my clinic time helping sort out bladder problems. This is why there are so many newsletters on the topic. One of the treatments recommended to all patients with bladder problems is pelvic floor exercises (PFE). However, I have recently been asking patients if their continence advisors have formally instructed them on how to do PFE. Most patients respond by saying they were given an instruction sheet or referred to the NHS pelvic floor exercise online or other online resources. What is clear is how few people have been adhering to the PFE regimen; I would estimate this to be less than 20% and probably less than 10% of patients.
If you don’t know the answers to the following questions please continue to read the remainder of this newsletter.
Do you know how to do pelvic floor exercises and at what intensity?
Have you adhered to doing your PFEs?
Who should do PFE?
Should men do PFEs?
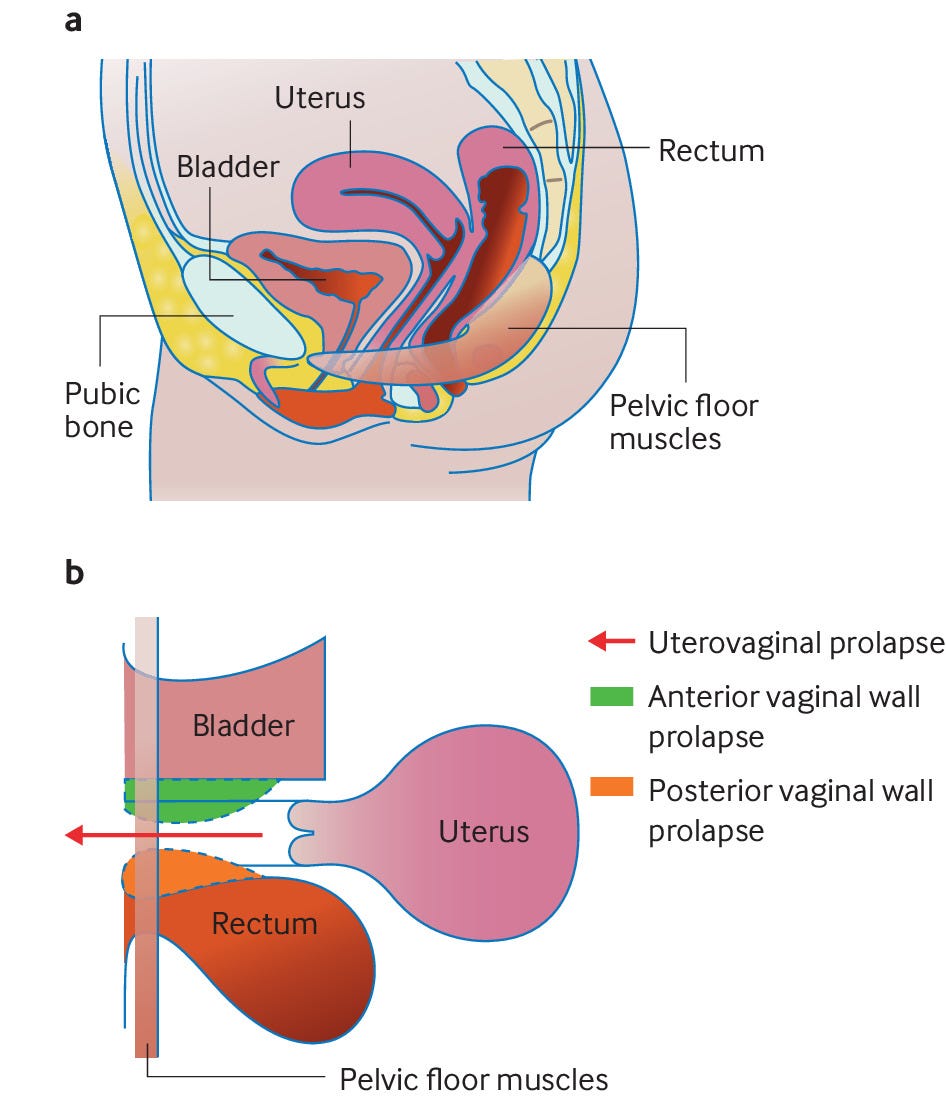
Anatomy
The pelvic floor consists of muscles and other tissues at the bottom of the pelvis. The muscles attach to the pelvic bones and sacrum. The pelvic floor supports the lower abdominal organs and is essential for maintaining bowel, bladder, and sexual function. The pelvic floor muscles have a constant tone at rest, i.e. they are tonically contracted. Voluntary and involuntary contraction and relaxation of the pelvic floor allow for normal bowel/anal, bladder and sexual function. For example, reflex muscle contraction in response to sudden increases in intra-abdominal pressure, for example, coughing or sneezing, maintain continence. Pelvic floor dysfunction cause symptoms such as urinary incontinence, voiding difficulty, pelvic organ prolapse, anal incontinence, evacuation difficulty, sexual dysfunction and pain.
Pelvic floor muscle training (PFMT)
PFMT, like all muscle training programmes, is designed to improve pelvic floor muscle strength, endurance, power, relaxation, or a combination of these. PFMT is typically unsupervised and self-administered. On the NHS, PFMT can be supervised by an HCP, typically a physiotherapist or a continence nurse. The National Institute for Health and Care Excellence (NICE) recommends PFMT to manage symptoms of pelvic floor dysfunction in women and that all women aged 12 and over should be encouraged to perform preventive exercises. When researching this piece, the last bit of information was new to me, but it makes sense. The pelvic floor is just another muscle, and strengthening it should help prevent pelvic floor dysfunction in the future. Therefore, I will add PFMT to my list of exercises for my MS prehabilitation programme.
PFMT is indicated mainly for urinary incontinence, pelvic organ prolapse and faecal incontinence. These are all problems associated with MS, and in many cases, MS is either the cause or contributes to these symptoms.
PFMT for women
The following is adapted from the BMJ’s ‘Pelvic floor muscle training: a practical guide’ (BMJ 2022; 378 doi: https://doi.org/10.1136/bmj-2022-070186).
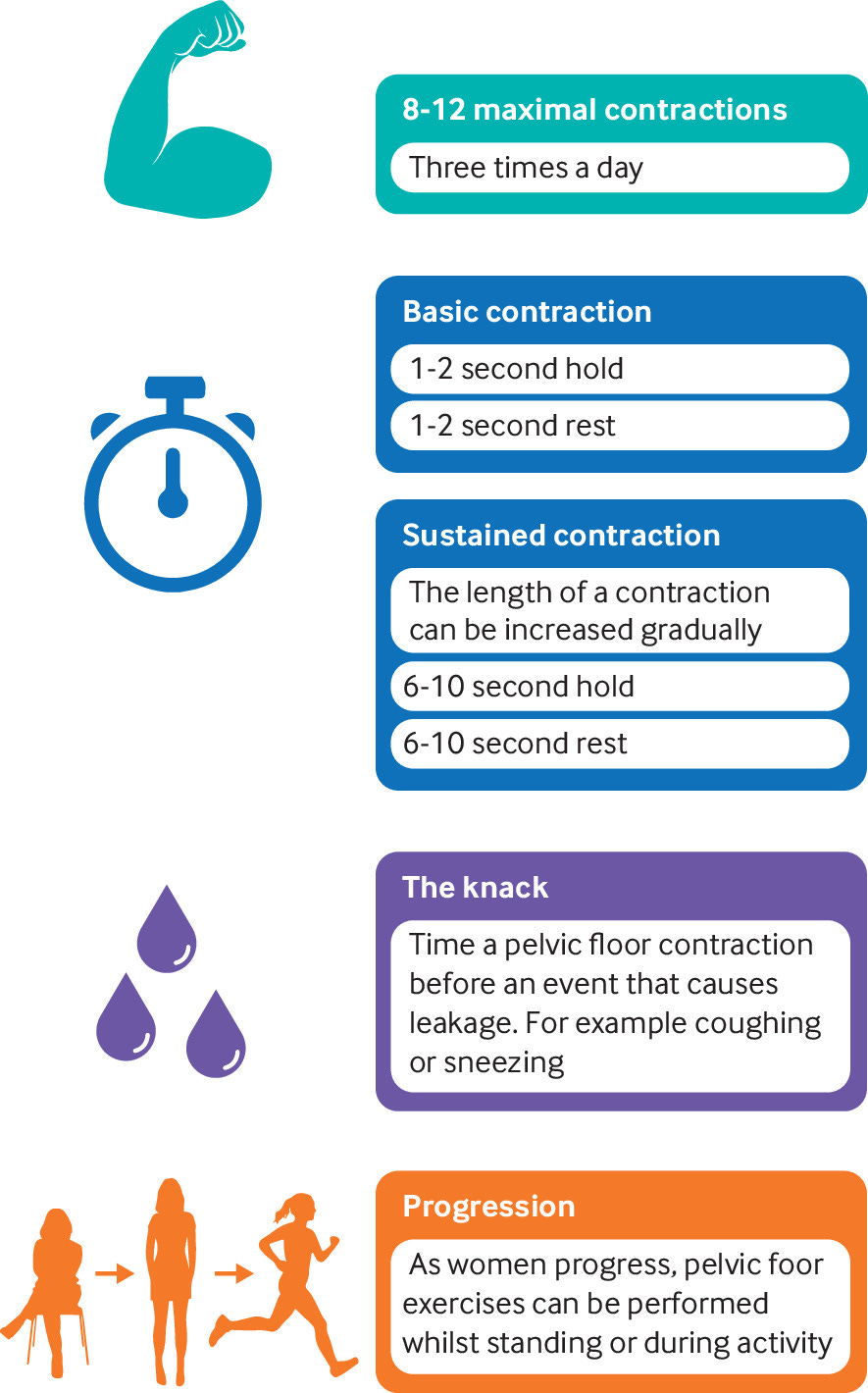
A self-administered programme should include basic voluntary contractions, which aim to improve pelvic floor muscle reaction to activities such as coughing, sneezing, exercise, and lifting, and sustained voluntary contractions, enhancing endurance. You need to sit comfortably with your knees slightly apart and contract the pelvic floor by lifting and tightening the muscles around the anus and vagina—as if to prevent the passage of gas and stop your urine flow. Once you can achieve PFMT seated, you can perform the exercises in a standing position and during activity. If you experience stress urinary incontinence, you can contract the pelvic floor in preparation for a leakage-provoking event called the “knack”. A basic voluntary contraction involves a hold of one to two seconds with the same rest time, while a sustained voluntary contraction should last between six and 10 seconds, again with the same rest time. Once you establish a baseline sustained contraction, the length of the sustained contraction should be increased gradually (to a maximum of 10 seconds).
The current recommendation is to do 8-12 maximal contractions three times a day.
Please be aware that approximately a quarter of women cannot perform a pelvic floor contraction on their first attempt with just verbal instruction, meaning a digital assessment of the pelvic floor is helpful to help you understand when you are contracting the muscles effectively. Therefore if your progress is minimal, please ask your MS team for a referral to a suitable HCP for a formal clinical assessment and a personalised, supervised PFMT programme.
Effective pelvic floor muscle contraction can be assessed using biofeedback devices, electrical stimulation, or vaginal cones prescribed by HCPs. You can purchase some of these devices, for example, weighted vaginal cones, online and some even come with Bluetooth-enabled apps.
Please note that various resources providing helpful instructions are available, for example, a patient education leaflet from the International Urogynecological Association (IUGA) and smartphone applications such as the Squeezy NHS pelvic floor app.
I would be interested to know which ones you have used and found helpful. Please be aware that the evidence that PFMT works is overwhelming, which is why you should start doing it regardless of whether or not you have pelvic floor dysfunction.
PFMT for men
Pelvic floor dysfunction can also occur in men, and PFMT is a recommended first-line conservative treatment measure. The following is from the Pelvic Obstetric & Gynaecology Physiotherapy guide for men.
Sit comfortably with your thighs, buttocks and tummy relaxed. Squeeze and lift the muscles from the front by either imagining you are trying to stop yourself from passing urine or trying to shorten or draw your penis up and inwards. Now try lifting the muscles from the back as if stopping the escape of wind. When you feel you have the hang of this, try lifting the front and back together. Don’t worry if you find it too difficult; after some practice, you will find the easiest and most comfortable method. This is a pelvic floor muscle contraction. To check that your pelvic floor muscles are working correctly: The evidence
Place your fingers on your perineum. You should feel the perineum lift upwards as you contract your muscles.
Stand in front of a mirror; when you do a pelvic floor muscle contraction, you should see the base of your penis draw inwards, and your testicles/ scrotum lift.
Try not to hold your breath while you contract your pelvic floor. You are more likely to breathe easily if you lift your pelvic floor on your out-breath. Do not actively clench your buttocks, but don’t be concerned if you simultaneously feel a tightening in your buttocks and/or lower abdomen. This is normal. If you cannot feel a definite tightening in the pelvic floor muscles, as with women, you should ask your MS Team to refer you for advice. On the NHS, the latter is typical via a urology service.
The Evidence
Kajbafvala et al. Pelvic floor muscle training in multiple sclerosis patients with lower urinary tract dysfunction: A systematic review and meta-analysis. Review Mult Scler Relat Disord. 2022 Mar;59:103559.
Background: Pelvic floor muscle training (PFMT) is a conservative treatment program for the management of lower urinary tract dysfunction (LUTD). This systematic review aimed to investigate the overall effectiveness of PFMT on LUTD in people with multiple sclerosis (MS).
Methods: Seven databases (PubMed/Medline, Scopus, PEDro, WOS, CINAHL, Cochrane, and Embase) were searched between 1990 and July 2019. We investigated urine leakage as our primary outcome. The secondary outcomes were neurogenic bladder symptoms measured by the overactive bladder questionnaire (OAB-V8 questionnaire) and the power/endurance of pelvic floor muscles.
Results: Fifteen studies were identified as eligible. Both urine leakage (standardized mean difference (SMD) = 0.50, 95% CI [-0.78, -0.23], and neurogenic bladder symptoms, SMD = -2.24, 95% CI [-4.44, -0.03] significantly decreased by PFMT in people with MS. PFMT increased the overall endurance and power of pelvic floor muscles moderately and significantly, SMD = 1.25, 95% CI [0.69, 1.81], and SMD = 0.64, 95% CI [0.24, 1.05], respectively.
Conclusions: Moderate to high-quality studies showed the overall efficacy of PFMT in decreasing urine leakage and neurogenic bladder symptoms and increasing endurance and power of pelvic floor muscles. MS patients with lower urinary tract symptoms could benefit from PFMT in the short term.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.













Share this post