Being a neurologist, who sees people with multiple sclerosis (pwMS), a clinical scientist, who studies the disease, and someone who is prepared to put his head above the parapet makes it hard not to disappoint people.
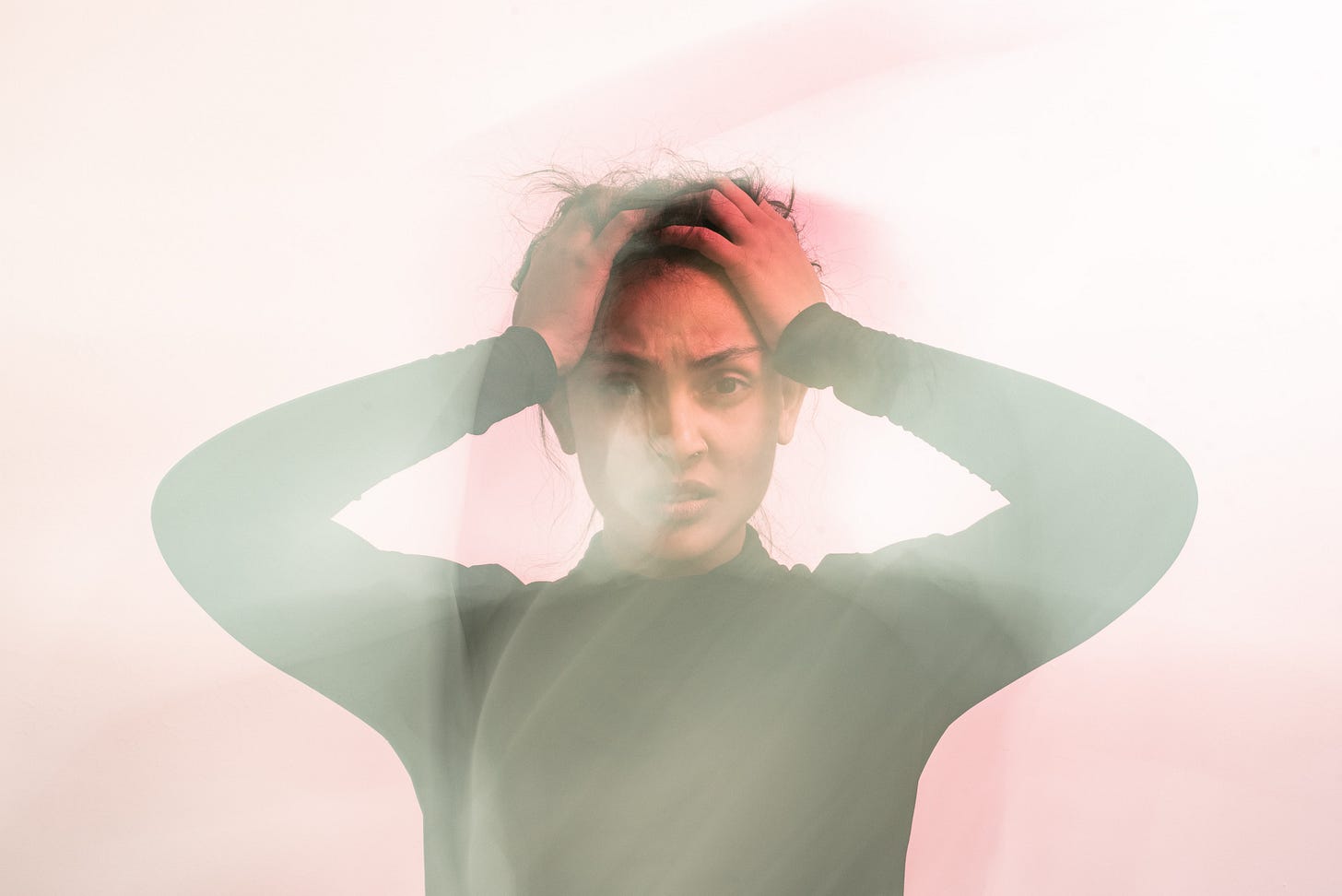
One of the issues that I underestimated in the past is the psychological impact that MS has on you, your family, your partner and your friends. This is compounded by disappointment when science and medicine, which promises so much, fail to deliver. This is particularly acute for people with relapse-onset MS when you realise that you have likely transitioned into the so-called secondary progressive phase of the disease and you realise that the disease-modifying therapies are not working as well as they should. Sadly, we the MS community have made secondary progressive MS another disease, which is much worse than relapsing-remitting MS.
In my medical sociology course at medical school, we learnt about Helen Kübler-Ross’s five stages of grief, best known by the acronym DABDA (Denial, Anger, Bargaining, Depression and Acceptance). For those of you with the relapse-onset variety of MS, not only do you have to go through these stages when you are diagnosed with having MS, but you go through these again when you enter the secondary progressive phase of the disease.
Sadly, MS has been made into a double-disease, which hits you twice!
The realisation that the DMTs are failing you leads to the re-emergence of grief and the five emotional stages that go with it. The anger is more often than not directed at the medical team for being impotent to stop the disease; exposing unrealistic expectations, which were created to give you hope. As a result of being an outspoken critic of therapeutic nihilism and therapeutic inertia, which blights of our profession, a proponent of early effective treatment and a disciple for the active and holistic management of MS, I tend to take more flak than most.
MS is a very personal disease and each pwMS has their own story to tell. Researchers, in general, seem to forget this and simply think of pwMS as a population of people with a disease. PwMS are not a population, but a group of individuals with their own hopes, fears and anxieties. Healthcare professionals understand this and this is why MS can’t be managed by an algorithm or care pathway and is the reason why the practice of neurology remains an art and not a science.
As a pwMS, you need to know about these stages of grief and recognise your emotional reactions to the diagnosis and realisation that you have transitioned to the progressive phase of the disease. The truth is our therapies for progressive MS at best slow down disease progression and do not halt worsening and rarely reverse disability.
It is important to be aware that if you have symptoms that are impacting your quality of life we may be able to help. You would be amazed what a difference effective symptomatic treatments can make to your quality of life. Simply, giving you back some control over your bladder and bowel function, improving your sleep, treating your anxiety, etc., can be the difference between wanting to live or not.
At the insistence of one of my patients, I have added an additional emotion or an A onto DABDA, ie. DABDAA. The extra A is for anxiety. The uncertainty that comes with a diagnosis of MS is unprecedented. What does the future hold for me? Will I be able to go to University, do a PhD, apply for that job and pursue my career? Will I be able to find a life partner, get married have a family? Will I be able to afford to have children? Will my partner leave me when I become disabled? Will I be able to continue working and earn enough money to support my family? Will be well enough to walk my daughter down the aisle on her wedding day? Will I still be around to see my grandchildren grow up? These are just a few of the questions people with MS ask me. It is little wonder pwMS are anxious.
If you need help coping with anxiety or any of the other emotions mentioned above please speak to your medical team.
D - denial
A - anger
B - bargaining
D - depression
A - acceptance
A - anxiety
Case study
I recently saw a patient for a second opinion. She was unable to tolerate dimethyl fumarate (Tecfidera) and has stopped taking her medication about 6 months ago. She was fully functional and apart from mild sensory symptoms, fatigue and intermittent ‘brain fog’ she felt ‘okay’. She was reluctant to start another DMT. She subsequently had an annual MRI that showed at least four new lesions with one large lesion that was enhancing in the parietal lobe. Despite being recommended to start on a more effective DMT she chose to wait and see what would happen over the next few months. Her diligent MS clinical nurse specialist didn’t like the wait and see attitude and recommended she saw me for a second opinion.
It was clear when the patient came into the room that she was very anxious and rapidly become clear she had not come to terms with having MS. She was clearly in denial and had not accepted having MS. I, therefore, went back to basics and discussed the emotional reactions and uncertainties that are triggered when someone is diagnosed with MS. I explained that the psychological impact that MS was having on her, and her family, was being underestimated. It was also clear that this young woman had no idea of how to deal with the uncertainty associated with having a potentially disabling disease.
As I was explaining to her about Helen Kübler-Ross’s stages of grief she started crying. She immediately related to these emotional stages. By the end of the consultation, she was willing to accept that she had active MS. I explained to her the risks associated with untreated MS and why I thought it was important for her to start a DMT. I provide her with the link to our ‘Brain Health: Time Matters‘ policy document so that she could read about the principles underpinning the contemporary treatment of MS. We also provided her with information on two DMTs that she would be eligible for and we have arranged to see her and her partner in 2-4 weeks time to discuss the option of her starting treatment. I also recommended that she should be referred for CBT and mindfulness therapy to help her come to terms with her MS and to treat her anxiety. She was surprisingly receptive to these psychological therapies.
It was clear that this patient left my consulting rooms a little less anxious than when she walked in. What the consultation taught me is that denial is a very strong emotion and unless you tackle it head-on it often impedes rational decision making about MS treatments.
I suspect most of you who are reading this Newsletter are beyond the diagnostic phase and the emotion of denial. If you are not, or if you, your partner or other family members have persistent anxiety, can you please arrange to see your neurologist or MS nurse specialist so you can discuss things in more detail. There are many treatment options we can offer you to help cope and come to terms with the diagnosis of MS.
I would be interested to hear about your own experiences and if you relate to these emotional stages.
Subscriptions/Donations
I have now changed the funding model of MS-Selfie. Access to MS-Selfie and the microsite, which is been worked on by a medical writer and web designer, will be free to all readers. I am relying on your generosity as paying subscribers and future paying subscribers to support the site for everyone. So if you value these Newsletters and Case studies please consider becoming a paying subscriber and I would like to thank those of you who have become paying subscribers already; your support is much appreciated. I am also planning to launch an online course or programme to help skill-up people with MS about the disease and to teach them how to self-manage their MS. Funds raised by subscriptions will also be used for this course.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.














Share this post