Case study
A few months ago, I saw a patient in her mid-forties for a second opinion. She had been diagnosed with primary progressive MS after presenting with a progressive right foot drop that had gotten worse over the last four years, and the weakness had now spread to the left leg and had started to affect her right hand. She also had bladder and bowel problems and sexual dysfunction. On history, she mentioned that about 18 years ago, she had an episode of facial muscle twitching that involved her eyelid and cheek. She described it as a rippling feeling, which lasted about a week before stopping. As the facial twitching resolved spontaneously, her GP did not do any investigations. Since then, she has had intermittent twitching of the eye muscles.
On history, it sounds as if this lady had facial myokymia, and this was likely her first manifestation of multiple sclerosis.
Prof G’s opinion
Should I give her the benefit of the doubt and change her diagnosis from primary progressive to secondary progressive? In the past, George Ebers used to call this single-attack progressive MS. He said it was an MS phenotype that bridged relapse-onset disease and primary progressive MS. Labelling this patient as either primary progressive or secondary progressive has consequences for her treatment. If she comes back from having her MRI scan and lumbar puncture, which I have ordered, and is shown to have active disease, i.e. new lesions or raised spinal fluid neurofilament levels, she would be eligible for ocrelizumab if she has PPMS and siponimod if she has SPMS. I discussed this with her, and she asked if we could not change her diagnosis as she would rather be offered ocrelizumab.
This case illustrates our problem with dividing MS into different subtypes based on the clinical phenotype rather than simply having one disease.
If you were this lady, would you rather be labelled as having PPMS or SPMS or, for that matter, just MS?
The sad thing about this lady is she should have had her facial myokymia investigated 18+ years ago and, if possible, diagnosed with MS then. She may have been eligible for treatment, which could potentially have delayed or prevented the progressive phase of her disease. Time really is brain and/or spinal cord.
Myokymia
Most people experience myokymia at some point in their lives. It is characterised by involuntary, spontaneous, and rapid contractions of a small group of muscles, causing visible twitching or trembling. Myokymia is usually harmless and temporary. However, it can be quite bothersome for those who experience it. Myokymia occurs when a nerve fibre supplying one motor unit fires or discharges spontaneously. Factors such as stress, fatigue, caffeine consumption, exercise, dehydration, and eye strain have been known to trigger or exacerbate myokymic episodes. While the condition can affect any muscle group, it is most commonly observed in the eyelids, resulting in eyelid twitching. I am sure many of you have experienced this. It is my observation that people with MS are much more susceptible to myokymia. I suspect as a result of small MS lesions affecting the motor nerves as they leave the brain stem and spinal cord. Yes, you can get focal myokymia affecting almost any muscle in the body.
The twitching or trembling associated with myokymia can vary in intensity, duration, and frequency. It may be barely noticeable in some cases, while it can be quite prominent and disruptive in others. Although myokymia can be annoying, it is generally not a cause for concern unless it persists for an extended period or is accompanied by other concerning symptoms.
Myokymia typically resolves on its own without the need for medical intervention. However, a few self-care measures can help alleviate the symptoms and reduce the frequency of episodes. These include getting enough rest and sleep, managing stress levels through relaxation techniques or exercise, limiting caffeine intake, and practising good eye hygiene, such as taking breaks from screens and ensuring proper lighting. In rare cases where myokymia persists or significantly interferes with daily life, it may require treatment. Myokymia generally responds to a group of drugs called sodium channel blockers, for example, carbamazepine, oxcarbazepine and lamotrigine.
It is crucial to differentiate myokymia from other more sinister disorders, particularly fibrillations from motor neurone disease or ALS (amyotrophic lateral sclerosis). Patients rarely feel fibrillations because they result in the contraction of a single or only a few muscle fibres rather than the larger muscle units muscle. Myokymia tends to be more rapid and involves a particular area. Myokymia can be the presenting symptom in multiple sclerosis or occur as part of a relapse. The lesions causing myokymia tend to be in the anterior root exit zone where the motor fibres leave the brain stem or spinal cord.
The issue of motor neurone disease (MND) should not be ignored. I have seen at least five patients with MS who have also developed MND. Data suggests that pwMS are at higher risk of developing MND (see paper one below). This is why if you have muscle twitching, you should ask your neurologist to take a look at it next time you see them. Muscle twitching is often transient, so I recommend recording it on your smartphone to show it to your neurologist when you next see them.
As in this patient, facial myokymia was likely the initial presenting symptom of their MS. As it was transient and not investigated, this patient missed out on being diagnosed and treated early for their MS. Has this happened to any of you?
In conclusion, myokymia is a common and generally harmless condition characterized by involuntary muscle twitching or trembling. While it can be annoying, it usually resolves on its own and can be managed through self-care measures. If the symptoms persist or worsen, it is advisable to consult a healthcare professional for further evaluation and guidance.
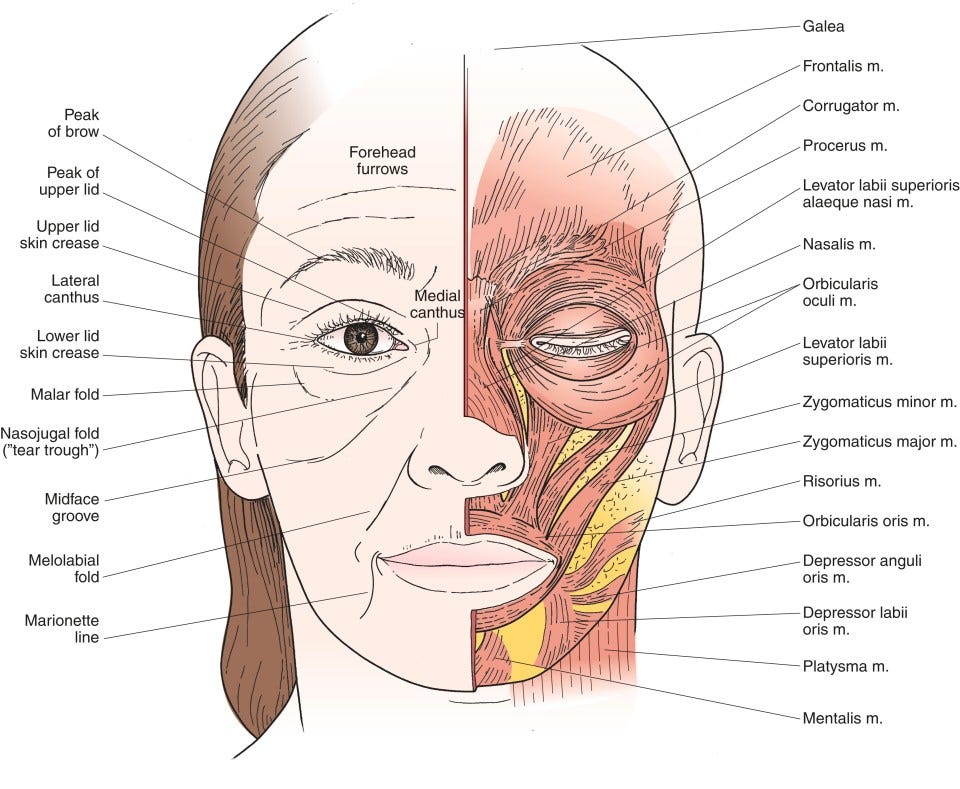
Please be aware that MS commonly affects the face. In addition to facial myokymia MS can cause facial or Bell’s palsy and hemifacial spasms. I would be interested to know how many of you had facial involvement from your MS and if it was misdiagnosed initially.
Paper 1: MS and MND
Objective: To study whether the risk of amyotrophic lateral sclerosis (ALS) is increased in people with prior autoimmune disease.
Methods: An all-England hospital record-linkage dataset spanning 1999-2011 was used. Cohorts were constructed of people with each of a range of autoimmune diseases; the incidence of ALS in each disease cohort was compared with the incidence of ALS in a cohort of individuals without prior admission for the autoimmune disease.
Results: There were significantly more cases than expected of ALS associated with a prior diagnosis of asthma, celiac disease, younger-onset diabetes (younger than 30 years), multiple sclerosis, myasthenia gravis, myxedema, polymyositis, Sjögren syndrome, systemic lupus erythematosus, and ulcerative colitis.
Conclusions: Autoimmune disease associations with ALS raise the possibility of shared genetic or environmental risk factors.
Paper 2: MS and facial Involvement
Background: Multiple sclerosis (MS) can present with facial symptoms and signs, such as facial palsy, myokymia, and hemifacial spasm. Considering the importance of early diagnosis, treatment, and exclusion of causes other than MS, we aimed to assess the prevalence of these disorders in patients with MS.
Methods: MS patients who were referred to the Isfahan MS clinic from March 2021 to March 2022 were observed for facial presentations of the disease. A checklist of patients' baseline characteristics and disease features were then completed through patient interview and medical files.
Results: Of the total of 2260 MS patients who were assessed, 3.27% had facial palsy, 1.28% had myokymia, and 0.84% presented with hemifacial spasm. The mean age of facial symptom onset was 30.74, 29.07, and 31.37 years, respectively. No relationship was found between the type of facial presentation and factors such as age, gender, subtype of MS, affected side of face, and time of presentation.
Conclusion: On the grounds that facial disorders can be the first presentation of MS, patients with atypical features of other common facial diseases such as Bell's palsy should therefore be carefully assessed and followed for any clues pertaining to the diagnosis of MS.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.













Share this post