Case study
I am someone who is immunosuppressed, after being treated with rituximab for non-Hodgkins lymphoma (NHL) in 2012, I have had both COVID-19 vaccinations and a booster, but have produced zero antibodies after them.
I was particularly interested in the ZOE podcast on 28th November - "How are COVID vaccines working in the immunocompromised?" which you took part in.
Specifically, as a 57-year-old man who is by and large still shielding, I noted your comments that your colleagues in the US are administering Ronapreve on a drive-through basis.
As someone in the UK, how can I be prescribed Ronapreve on a preventative basis, rather than waiting to get COVID and having the drug administered as treatment?
If it can be administered so freely in the US, could I buy some, go there and get to the back of the drive-through queue?
Any assistance you might be able to give about accessing Ronapreve, in the UK / US or via the NHS? I would be delighted to receive it.
Prof G’s opinion
Although this person does not have MS his situation is very similar to many people with MS (pwMS) who are on anti-CD20 therapies (ocrelizumab, ofatumumab or rituximab) or S1P-modulators (fingolimod, siponimod, ozanimod or ponesimod) and have not seroconverted after three doses of a COVID-19 vaccine.
Would knowing you had an anti-SARS-CoV-2 T-cell response make a difference? I suspect not, because we don’t know if having a T-cell response against SARS-CoV-2 in this situation is protective against symptomatic and severe infection and death.
To be brutally honest, I suspect not. Firstly, we know that antibody responses, in particular IgA responses, are required to prevent infection with SARS-CoV-2. Please note IgA are the type of antibodies that are secreted onto mucosal services and function to prevent the coronavirus from binding to its receptors and entering the cell. Secondly, we have had several patients on anti-CD20 therapy, who have been vaccinated, failed to seroconvert, who have unfortunately gone on to develop severe COVID-19 requiring admission to hospital. Tragically one of our patients died.
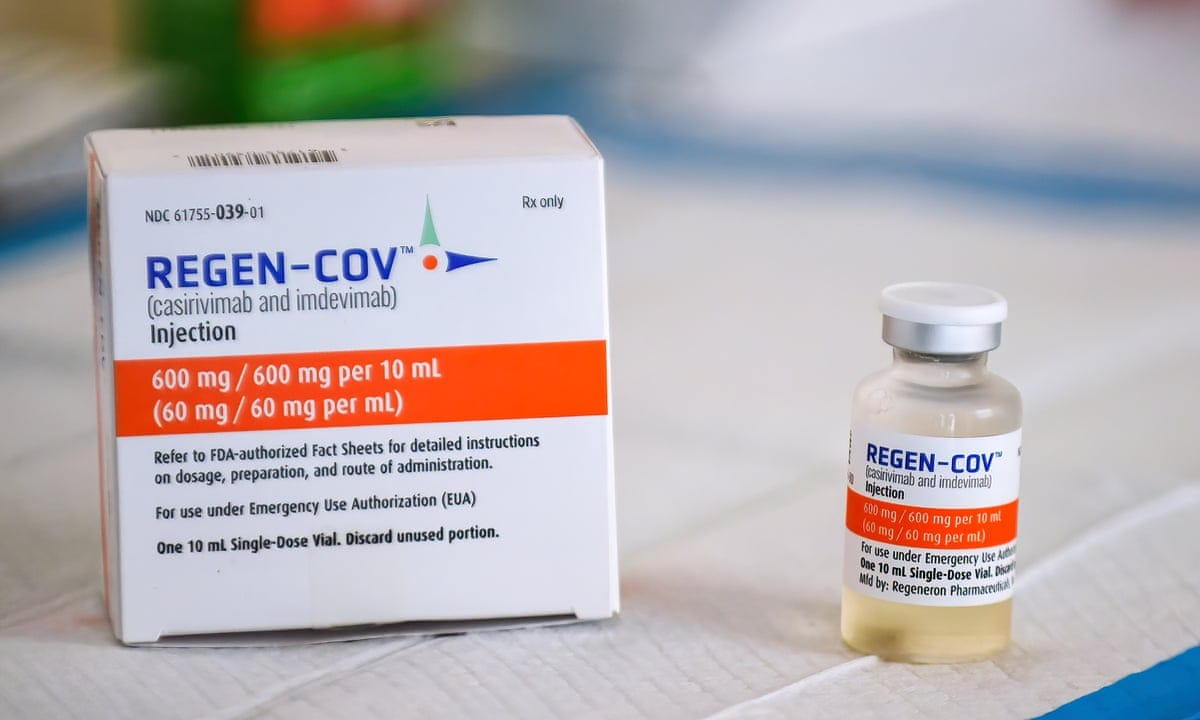
The good news is that we now have licensed specific treatments on the NHS to treat COVID-19. The first treatment is the pair of monoclonals casirivimab and imdevimab (also called Ronapreve, REGEN-COV or REGEN-COV2). The only people who really benefit from Ronapreve are those who are seronegative when treated with casirivimab and imdevimab compared to usual care. NICE, therefore, recommends Ronapreve to hospitalised seronegative COVID-19 patients aged 12 and over. Please note in our hospital COVID-19 has to be confirmed with a positive antigen test and not just a PCR assay. I suspect this to make sure only patients with high viral loads and who are actively infected get treated. Please note a positive SARS-CoV-2 PCR test does not necessarily tell you that you have active viral replication, whereas an antigen test does.
The other issues are availability. I am aware that globally there are limited supplies of Ronapreve and in the UK availability may not be universal yet. I am aware that most large centres have a supply of Ronapreve, but I would be surprised if all small hospitals had a ready supply of the drug. What I do know is that Ronapreve is not available on the NHS as prophylactic therapy, because of the recent NICE guidance and supply issues. This is despite it being licensed by the MHRA as both a prophylactic and treatment of acute COVID-19.
Just to say I am aware that Ronapreve has had a slow roll-out in the UK, which has been covered in the press. As with all new treatments, adoption can be slow in the NHS. For example, one of my patients who is been treated with ocrelizumab was admitted with COVID-19 last Sunday to her local district general hospital and only received Ronapreve, yesterday. This was on day 5 of her admission to the hospital with significant deterioration in her lung function and increasing oxygen requirements. The latter is despite us notifying her medical team of the need to consider her for Ronapreve on Monday. Maybe the message to the respiratory clinicians is that in the same way time that time is brain for MS, time is lung in COVID pneumonia.
Although Ronapreve is available in the US there is also a shortage and a federal programme is in place to ration access to the drug. So yes, the drug is available in the US but it is not something that is widely available. Most US neurologists I have spoken to are not using it prophylactically, but as a treatment when their patients develop COVID-19.
Other treatments
Please note the treatment of COVID-19 is rapidly evolving. In some countries regdanvimab (Regkirona) a single monoclonal is available and a longer-acting cocktail of tixagevimab and cilgavimab (AZD7442) from Astra-Zeneca is currently being fast-tracked through the regulators.
Molnupiravir (Lagevrio) from Merck is now available for the treatment of mild to moderate COVID-19 in adults with a positive SARS-COV-2 diagnostic test and who have at least one risk factor for developing severe illness. Pfizer has also announced strikingly positive results for their SARS-CoV-2 oral protease inhibitor referred to as PF-07321332 (Paxlovid), which is 89% effective in reducing COVID-19 hospitalisation and death. PF-07321332 is co-administered with a low dose of a drug called ritonavir, which slows down its metabolism, or breakdown. The ritonavir allows PF-07321332 to remain active in the body for longer periods of time at higher concentrations to help combat the coronavirus.
So, in summary, prophylactic monoclonal antibody therapies are not available on the NHS and you will not be able to access them via the private sector either. The latter applies to the UK and the USA, due to the global shortage and rationing of the drug. However, with the rapidly evolving therapeutic landscape, you are likely to have access to at least one or possibly two oral antivirals within weeks to months. I am aware that the UK Government has bought a large supply of molnupiravir (Lagevrio).
In the event of you needing to be admitted to the hospital, I would urge you to go to a large teaching hospital armed with the information that you are (1) immunocompromised, (2) anti-SARS-CoV-2 spike antibody-negative despite being vaccinated and (3) if you have confirmed infection (positive antigen test) then you are eligible for Ronapreve treatment.
Please be aware that the shelf-life of these monoclonal antibody therapies is limited in that they are designed to target specific areas of the spike protein. With time these antibody therapies will likely select for mutant or escape variants. The latter is inevitable (evolutionary certainty), which is why we need ongoing drug and vaccine development against SARS-CoV-2.
Vaccine booster
I note you have had three doses of a COVID-19 vaccine. As you are immunocompromised you should be able to get the booster dose counted as being part of your primary vaccination and hence will be eligible for a booster dose from month 5 after your third dose. When you do have your next booster I would try and have the Moderna RNA vaccine that has a much better seroconversion rate with higher titres that wane more slowly. Saying this if you can’t have a Moderna vaccine the Pfizer-BionTech should be sufficient.
Prehabilitation
As always you should be doing everything you can to maximise your general health. I call the latter prehabilitation and I discuss this in an earlier MS-Selfie Newsletter (Prehabilitation the ultimate in self-help. 5-July-2021).
Social Responsibility
Finally, as you live in the UK don’t you believe in the NHS and its founding principles, i.e. equitable care and free at the point of access? If there is such a shortage of Ronapreve in the UK and globally every dose that is currently been given prophylactically, which may not be needed, is one less potentially life-saving dose for someone with COVID-19. I suppose this is the difference between being a socialist and neoliberal. Do you agree?
Subscriptions
If you are a subscriber thank you. The subscriptions are essential for making this initiative viable long-term. The idea is to use the subscriptions to hire the necessary staff to curate the information on a standalone MS-Selfie website and to potentially produce a series of self-help guides. Please note if you can’t afford to subscribe and have MS and want access to all the case studies please drop me an email and I will give you a complimentary subscription. I have made this case study accessible to all readers as the topic is so important to your general health.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.












Share this post