Over the years, it has become apparent to me that people with multiple sclerosis (pwMS) seem to accept developing several comorbidities as if it is just part of having multiple sclerosis (MS). It is as if having MS and living with MS is so overwhelming that other medical problems tend to be ignored. Am I correct in my interpretation? Do pwMS suffer from medical inertia when recognising or identifying other medical problems? I suspect medical gaslighting may contribute to this problem in that many healthcare professionals (HCPs) often attribute symptoms to having MS when particular symptoms may be related to comorbidities or other medical problems.
One of these comorbidities is rectal bleeding. A few weeks ago, I saw a patient who had had intermittent rectal bleeding. He had been passing fresh blood when going to the toilet for several months. He wasn’t concerned about the bleeding as he had put it down to having haemorrhoids. This was despite no prior history of haemorrhoids and no current history of prolapsed haemorrhoids. He assumed he had haemorrhoids because he suffers from MS-related constipation and has to strain on passing stool. He only mentioned the bleeding to me because I asked him about his bowel habits and whether or not he had noticed any changes.
Yes, pwMS are more likely to have anorectal pathology due to chronic MS-related constipation, but you mustn’t assume this is normal and simply a part of having MS. Rectal bleeding is always abnormal, is not due to having MS and always needs to be investigated.
Common causes of rectal bleeding in pwMS
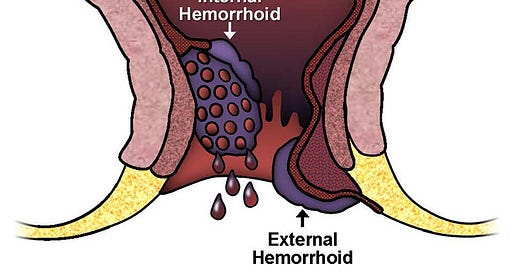
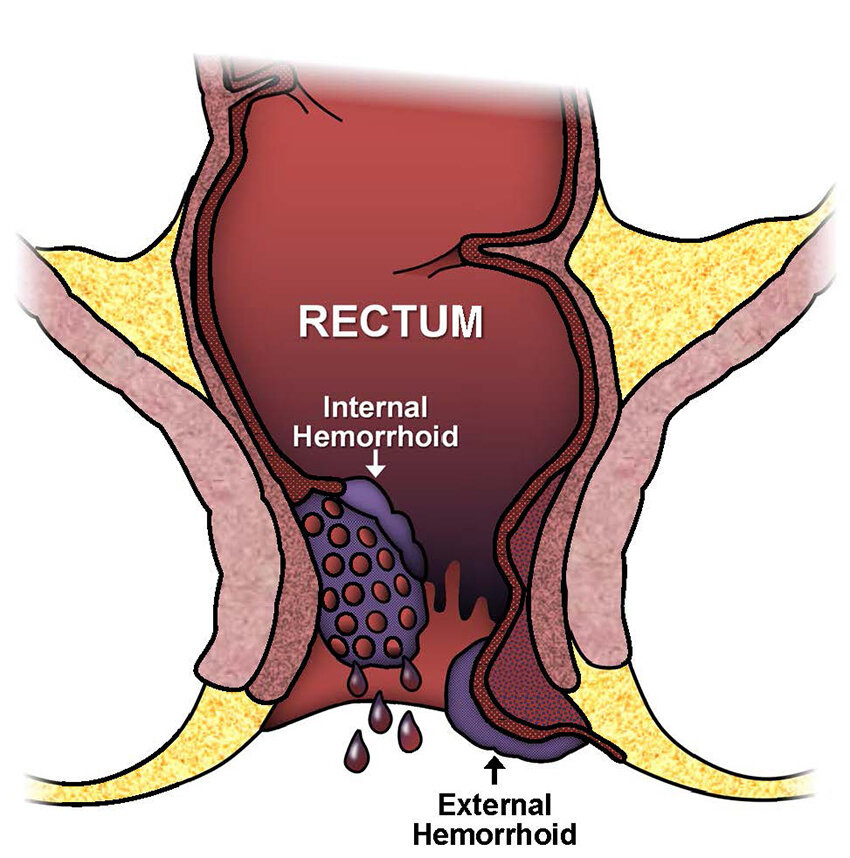
1. Constipation and haemorrhoids - constipation is one of the most prevalent gastrointestinal (GI) symptoms in pwMS. It is primarily due to decreased intestinal motility, reduced physical activity, pelvic floor dysfunction, poor diet and/or side effects of medications. Straining during bowel movements can lead to the development of haemorrhoids, which are swollen blood vessels in the lower rectum or anus, causing rectal bleeding.
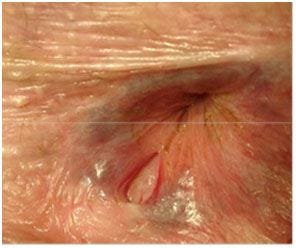
2. Anal fissures - anal fissures are another common cause of bleeding related to constipation. These small tears in the lining of the anus can occur when trying to pass hard or large stools, leading to painful bowel movements and rectal bleeding.
3. Medication side effects - certain medications used to manage MS symptoms or the disease itself can contribute to GI issues, including rectal bleeding. Drugs such as non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief can increase the risk of gastrointestinal complications like ulcers, gastrointestinal bleeding and rarely NSAID-related colitis.
4. Inflammatory bowel disease (IBD) - though not directly caused by MS, there is an association between autoimmune diseases like MS and conditions such as Crohn’s disease or ulcerative colitis, which fall under IBD. These conditions can cause inflammation of the gastrointestinal tract, leading to symptoms like diarrhoea, abdominal pain, and rectal bleeding.
5. Infections - infections of the GI tract or the anal area, which may be more common in individuals with compromised mobility or those on immunosuppressive treatment for MS, can lead to rectal bleeding. These might include bacterial, viral, or fungal infections affecting the intestines or anal area.
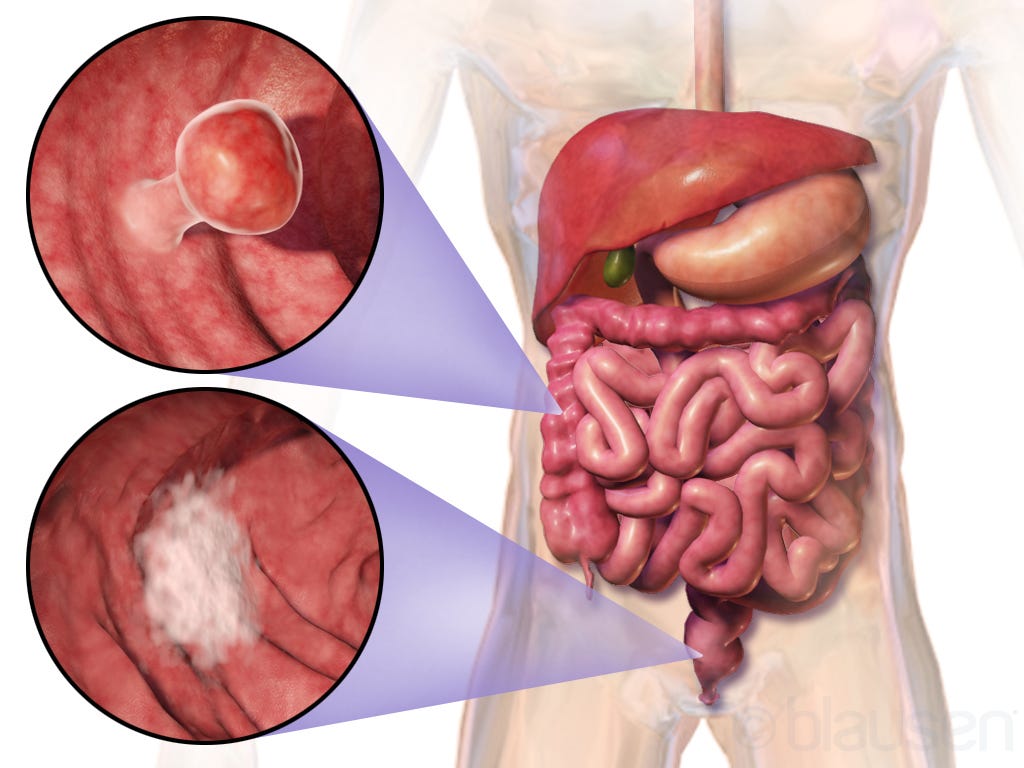
6. Polyps and anal cancer - rectal bleeding is often a harbinger of colonic and anorectal cancers. This is why anyone presenting with rectal bleeding needs to be examined.
7. Diverticular disease - colonic diverticular disease is a condition characterised by the formation of diverticula in the colon. Diverticula are small, bulging pouches that can form in the lining of the digestive system. While they can occur anywhere in the intestines, they are most commonly found in the large intestine or colon. The presence of these pouches themselves is known as diverticulosis. The condition is called diverticulitis when one or more pouches become inflamed or infected. The exact cause of diverticular disease is not fully understood, but it is believed to be associated with low-fiber diets. Fibre helps to soften stool and make it easier to pass, reducing pressure inside the digestive system. Without enough fibre, the colon has to exert more pressure to move small, hard stools, which can lead to the formation of diverticula. Other risk factors include ageing, obesity, smoking, lack of exercise, and certain medications like nonsteroidal anti-inflammatory drugs (NSAIDs).
8. Colonic telangiectasia - colonic telangiectasia, also known as angiodysplasia of the colon, refers to a condition characterised by the presence of small, dilated blood vessels in the colon. These vascular lesions are typically flat, red and can range in size. They are most commonly found in the right colon but can occur anywhere in the large intestine. Telangiectasias in the colon are a form of vascular ectasia, which means they are part of a group of conditions that involve the dilation of blood vessels. The exact cause of colonic telangiectasia is not completely understood, but it is believed to be related to the ageing process and the degeneration of blood vessels. Several factors may contribute to its development, including ageing, chronic constipation and cardiovascular disorders.
8. Rectal prolapse - rectal prolapse occurs when the rectum loses its normal attachments allowing it to stretch and protrude out through the anus. This condition can be distressing and often impacts the quality of life, leading to embarrassment and social isolation for those affected. Rectal prolapse is different from haemorrhoids, which are swollen blood vessels that line the anal canal. A partial prolapse (also known as mucosal prolapse) is when only the lining (mucosa) of the rectum protrudes from the anus. In comparison, complete prolapse is when the entire wall of the rectum protrudes from the anus. This prolapse may initially occur during bowel movements and retract afterwards, but over time, it may not. PwMS are at risk of rectal prolapse because several factors contributing to its development are common in pwMS. This includes chronic constipation or straining during bowel movements, which over time weaken the rectum’s support structures in the pelvic floor. Other risk factors included childbirth, ageing and possibly some medications that relax muscles. For example, it seems to commoner in habitual cannabis users. Symptoms of rectal prolapse can vary depending on the severity and include visible prolapse, rectal bleeding and mucus discharge, faecal incontinence, anal leakage, the inability to control bowel movements and the sensation of incomplete evacuation.
Identifying the cause of rectal bleeding in pwMS involves a detailed medical history, physical examination, and sometimes diagnostic procedures like colonoscopy or sigmoidoscopy. Treatment depends on the underlying cause and might include dietary management for constipation, medication adjustments, or specific treatments for conditions like haemorrhoids, anal fissures, IBD, etc.
It is crucial that if you are experiencing rectal bleeding, you consult a healthcare professional for appropriate diagnosis and management. It is critical to rule out any serious underlying conditions, in particular early cancer.
While multiple sclerosis itself does not cause rectal bleeding, its associated symptoms, the indirect effects of its management, and related autoimmune conditions can contribute to GI symptoms, including rectal bleeding. Understanding these connections emphasises the importance of comprehensive care in managing MS, highlighting the need for a multidisciplinary approach that includes monitoring and addressing gastrointestinal health.
I would be interested to hear if any of you have had rectal bleeding and how you approached it. Having MS may increase your risks of getting several comorbidities, but all of these comorbidities need to be managed on their own merits and not assumed to be just another part of having MS. And don’t accept being gaslit. If you have symptoms that you think are not related to your MS, make a fuss and get them investigated.
The patient I am referring to above was found to have early rectal cancer.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
X (Twitter) / LinkedIn / Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.












Share this post