Case study
I saw a patient with possible MS a year or two ago. He had been told that he couldn't have MS because he only had one lesion on his MRI, which was equivocal. However, when I took a history and examined this patient, he had evidence of dissemination in time and space. He had had a previous episode of facial weakness that had been put down to Bell’s palsy several years ago. The Bell’s palsy had been considered to be unrelated to his current problems. More recently, he had an episode of vertigo and unsteadiness of gait, which was diagnosed as possible vestibular neuronitis. This was followed by an episode of numbness and clumsiness in his left hand.
When I examined him, he had jerky eye movements (nystagmus), facial asymmetry due to mild residual weakness from his so-called Bell’s palsy and mild weakness and loss of sensation in his left hand. These signs were likely due to three separate lesions or at least two lesions (dissemination in space), which also had disseminated in time. The latter was based on a clear gap between these three episodes.
I looked at his MRI, and apart from a definite MRI lesion in his brainstem, the remainder of his MRI did not show any other clear lesions. However, the white matter in his brain did look dirty (possible diffuse pathology), and his spinal imaging had not included cuts through the cord (axial images), which in my opinion, was a suboptimal scan.
Prof G’s opinion
Contrary to what his initial neurologist had told him, I thought he likely had MS. I then suggested a lumbar puncture, repeat imaging and evoked potentials as part of the extended work-up. The patient declined and then complained, arguing that I contradicted his initial neurologist's diagnosis. How could I suggest a diagnosis of possible MS with only one equivocal lesion on MRI?
In this context the clinical history and examination trump the MRI. Although uncommon, you can have MS and a normal or near-normal MRI. However, this is uncommon. Most neurologists feel reluctant to diagnose MS with a normal MRI. I suspect his initial neurologist had considered a diagnosis of MS but had settled on a diagnosis of CIS, which allows them to wait and see what happens. The latter is called watchful waiting and is commonly used in neurology, where time is often the best diagnostician.
This issue of a normal MRI or MRI that is not typical of MS is very topical because of a recent case reported by the BBC (6-Oct-2022) of a patient who turned out to have MS that was not diagnosed sooner. The ombudsman who investigated this case found that he had suffered "significant injustice" after a neurologist failed to diagnose him with MS. The patient said he felt doctors did not believe him. Reading between the lines, this patient is likely to have suffered medical gaslighting.
For more information on medical gaslighting in MS, please see the following two newsletters:
Multiple sclerosis is a biological disease and the diagnostic criteria don’t necessarily require an abnormal MRI, i.e. you can show dissemination in time and space clinically. An MRI, however, is mandatory in this situation, not necessarily to help diagnose MS but to exclude MS mimics.
It transpires that this patient had been told because he had CIS he was at increased risk of developing MS in the future. He had then sought a second opinion in the hope that I was going to say he didn’t have CIS or MS.
The diagnosis of MS remains clinical and is underpinned by the need to show (1) dissemination in time (typically new activity four weeks apart or the presence of locally produced oligoclonal IgG bands in the spinal fluid) and (2) dissemination in space (symptoms and/or signs affecting two different pathways in the CNS) and (3) the exclusion of other possible diagnoses. It is clear that based on these criteria, you don't necessarily need to have visible or specific MRI lesions to diagnose MS. However, neurologists feel uncomfortable making a diagnosis of MS or CIS if there are no visible lesions on MRI. In other words, from a practical and clinical perspective, MS has become a MACROscopic or MRIscopic disease. Therein lies the rub.
MS is characterised pathologically by multifocal inflammatory lesions that cause demyelination and variable degrees of axonal loss. Please note I have dropped using the term white matter. MS is a white and grey matter disease with more than half the lesion burden in the largely MRI-lesion-invisible grey matter component (see study below). Even in the white matter, where it is easier to see lesions, the resolution of an MRI scan is down to about 3-4 mm. Many more MS lesions are found pathologically than seen on MRI or with the naked eye at post-mortem. Therefore, particularly early on in the course of the disease, there will be a small number of people with MS with one or no lesions who have MS.
A very small lesion in a strategic pathway can cause typical symptoms and signs, but when you investigate many of these patients with an MRI scan, you see no obvious lesion in the expected area. This happens more often than not with a so-called internuclear ophthalmoplegia (INO), a very specific eye movement problem that presents with double vision on looking to the left or right. This is an example of a microscopic lesion causing an MS attack. This is why we shouldn't be using MRI to confirm or make a relapse diagnosis in pwMS.
The study below, which is rapidly becoming a citation classic in the field of MS, shows you with elegant infographics how large the lesion burden is in MRI-invisible areas using our standard clinical sequences. More than half the MS disease burden occurs in regions that are MRI invisible.
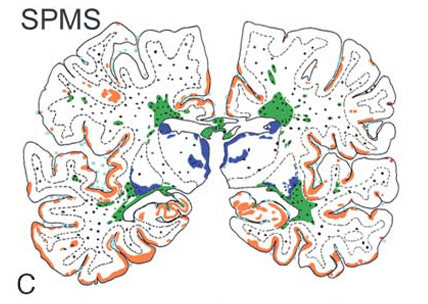
Focal demyelinated plaques in white matter, which are the hallmark of multiple sclerosis pathology, only partially explain the patient's clinical deficits. We thus analysed global brain pathology in multiple sclerosis, focusing on the normal-appearing white matter (NAWM) and the cortex. Autopsy tissue from 52 multiple sclerosis patients (acute, relapsing-remitting, primary and secondary progressive multiple sclerosis) and from 30 controls was analysed using quantitative morphological techniques. New and active focal inflammatory demyelinating lesions in the white matter were mainly present in patients with acute and relapsing multiple sclerosis, while diffuse injury of the NAWM and cortical demyelination were characteristic hallmarks of primary and secondary progressive multiple sclerosis. Cortical demyelination and injury of the NAWM, reflected by diffuse axonal injury with profound microglia activation, occurred on the background of a global inflammatory response in the whole brain and meninges. There was only a marginal correlation between focal lesion load in the white matter and diffuse white matter injury, or cortical pathology, respectively. Our data suggest that multiple sclerosis starts as a focal inflammatory disease of the CNS, which gives rise to circumscribed demyelinated plaques in the white matter. With chronicity, diffuse inflammation accumulates throughout the whole brain, and is associated with slowly progressive axonal injury in the NAWM and cortical demyelination.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription, please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.














Share this post