Gaslighting: an institutional problem
Gaslighting is simply another form of abuse or discriminatory behaviour no different from sexism, racism or ageism. This is why I am so shocked with the survey results.
Before reading this Newsletter, can you please read the last one on ‘Medical Gaslighting’ (22-Aug-2022) and complete the associated survey if you have not done so already?
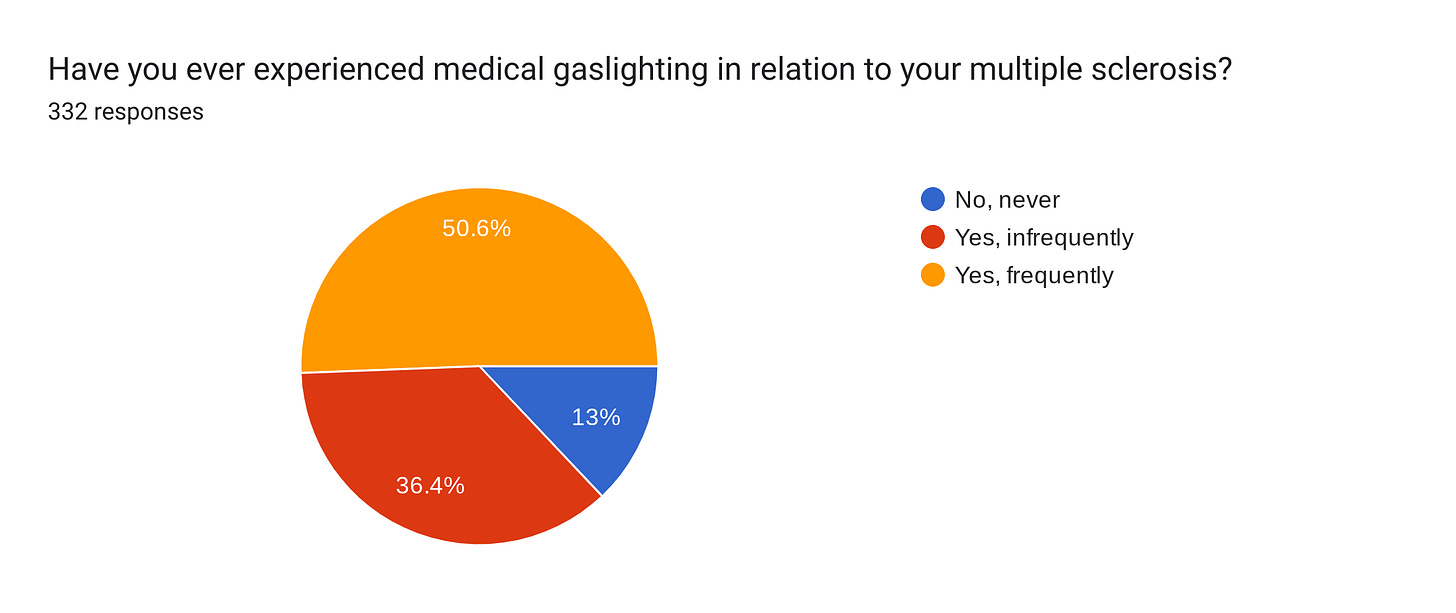
I was horrified and shocked by the interim analysis of the survey. The vast majority of you report being gaslighted, i.e. having had your (1) symptoms or concerns dismissed or ignored without cause, (2) feeling as if your healthcare provider is blaming you or (3) you have had your symptoms written off as being normal without explanation.
Women with MS are slightly more affected by medical gaslighting than men, and it is not related to age (data so far). The latter was surprising, as I would have thought it could be generational.
Medical gaslighting happens at all stages of the disease, but a common theme is ignoring or misinterpreting symptoms before the diagnosis of MS. I am aware that this is a common problem, which has been seen in other surveys.
On reflection, I am sure I am guilty of medical gaslighting as well. In some cases, it may even be deliberate. I have many patients who come to me with pages of problems, and I simply don’t have the time to deal with all their complaints. So time, or more correctly, lack of time, is one reason for medical gaslighting. Another is a lack of knowledge or experience and not being able to admit you don’t know. However, the most worrying reason is the power dynamic, with HCPs wanting to be in control or remain in control. I think I am old enough for the latter not to matter; clinical wisdom is related to experience and age.
You may or may not have realised that MS-Selfie as an initiative tries to address this power dynamic by giving you useful information to self-manage your MS or at least ask the right questions.
The recent New York Times (NYT) article on medical gaslighting is excellent and tells you to look out for it and makes the point that it can be subtle. The following are red flags:
Your HCP continually interrupts you, doesn’t allow you to elaborate and doesn’t appear to be an engaged listener.
Your HCP minimises or downplays your symptoms, for example, questioning whether you have pain.
Your HCP refuses to discuss your symptoms.
Your HCP will not order key investigations to rule out or confirm a diagnosis.
You feel that your HCP is being rude, condescending or belittling.
Your symptoms are blamed on a mental problem, but you are not provided with a mental health referral or screened for such a problem.
I suspect safety netting may be misinterpreted as gaslighting. Safety netting describes activities within the consultation with the HCP and at healthcare systems levels (diagnostic and treatment algorithms) to avoid over-investigation and overdiagnosis. Many symptoms are non-specific, and because of uncertainty, the HCP and the patient adopt a wait-and-see approach with clear instructions on how to identify the need to seek further medical help if their condition fails to improve, changes, or if they have ongoing concerns about the problem. Safety netting is considered good clinical practice. A recent BMJ article on safety-netting makes the following points:
Aggressively treating or investigating all patients with early undifferentiated illness is poor medical practice and can be harmful
Time is an important diagnostic tool but it creates a period of uncertainty and risk for patients with serious underlying conditions
Safety-netting can help mitigate this risk, and a traffic light framework provides a structure for delivering safety-netting advice
The point about safety netting is that it needs to be done as a part of a shared-decision making process, and therefore it shouldn't be interpreted as gaslighting.
So what can you do to advocate for yourself? The NYT article suggests the following:
Keep detailed notes and records; patient-held notes transform consultations and force you to become a partner in your healthcare.
Record the consultation. Many HCPs don’t like this but say you need to listen to the conversation again to make sure you don’t forget things or miss out on important information. You will be surprised how this changes the HCP’s behaviour.
Ask questions. Then ask some more. And don’t be fobbed off; if you are unsatisfied with the answer, ask the question again.
Take a person with you to the consultation for support. Having a witness has a similar effect to recording the consultation or documenting it with notes.
Focus on your most pressing issues, i.e. prioritise your time with your HCP. The consultation needs to be a two-way discussion. If your HCP is pressed for time, say you understand, but you would like to prioritise the following issues today. By doing this, you frame the limits of the consultation. Also, don’t expect the HCP to have all the answers at their fingertips, but do expect them to come back later with the answer.
Try and pin down the next steps for your problem, i.e. investigations, treatment, etc. Ask where the action point is, i.e. if the MRI shows this, how will that change my management? How soon will I get to switch treatments? …
If you’re still being ignored, what are your options?
Get a second opinion and ask to switch to a new HCP
Look to support groups or forums. Many of the MS charities have helplines you can use to discuss these issues.
Appeal to a higher authority; the person above your HCP, i.e. their line manager. In the NHS, we have a very simple procedure for patients to complain or question their care. It is called PALS (The Patient Advice and Liaison Service).
Abuse, manipulation, gaslighting, and delaying a diagnosis are potentially reportable events which HCPs need to know about. This is why, rather than suffer in silence, make your healthcare system aware of the problem.
Healthcare systems and the professions
The startling finding is that neurologists were the most frequent offenders (76%), followed by family doctors or GPs (50%), MS nurse specialists (34%) and then a long list of other HCPs. What differentiates the worst performers is that they have to take a history and possibly do an examination before interpreting symptoms and signs.
Some of the personal stories you have left behind reveal to me how pervasive and serious the problem is and indicate that the medical profession is not only arrogant but has a culture of not listening and ignoring patients. Many of you explain how medical gaslighting has affected your MS management and mental health. I wish I could apologise on behalf of my profession. I am trying to understand why this is such a problem in MS, although it may be more ubiquitous than we realise, and I am trying to think of ways to address this issue, so it doesn’t happen in the future. If you have any ideas, please share them; MS-Selfie is meant to be a two-way street so we can learn from each other.
We need to include medical gaslighting as part of the medical curriculum so that HCPs know it as part of their training. It is critically important to get HCPs to buy into the model of patients being equal partners in diagnosing and managing their disease. The paternalistic or older patronising healthcare model where the HCP knows what is best and not the patient is out-moded.
So, in summary, it boils down to education, education and more education. Once the survey closes next week, I will analyse the data to submit it to an MS meeting and potentially write it up as a paper. This can act as a catalyst to make MS HCPs more mindful of their practice. I also think we as professionals need to call out gaslighting when we see it happening. Gaslighting is simply another form of abuse or discriminatory behaviour no different from sexism, racism or ageism. The question is whether or not it is deliberate or an institutional problem, i.e. it is part of the dominant medical culture. I suspect the latter. This is why we will need a wider campaign to tackle the problem with clearly defined carrots (incentives/rewards) and sticks (disincentives/ punishment) to change our behaviour.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.







You asked for feedback on what could improve the situation, this is one hugely important one (I think) coming at it from a system design perspective: Often patients don’t have the right language to adequately describe what is happening to them, and this is a barrier to good care. For example, someone who doesn’t know what vertigo is, may describe this as simply “dizziness” which is quite non-descriptive, nor does it screen whether or not it is 24/7 constant, or provoked by head movement. Rarely do GPs, the first line of contact, or even neurologists, take the time to help probe a patient to better (or more accurately) articulate their symptoms (and patients may have not had the time to introspect carefully, self-examine, and think to describe them better).
In essence, physicians are taught to think about symptoms in very specific terms, and can fail to remember patients can’t always arrive at the right descriptions on their own, making it harder to get adequate care and taking many visits. A large communication gap also exists as well as a time issue.
An easy way around this, that doesn’t eat up physician’s time, is to develop electronic waiting room surveys (on a tablet) that ask the patient why they are here today, providing questions to help discern and describe their symptoms with greater specificity. E.g., if “dizziness” is the reason for the visit (key word of what is input), the app gives differentiating questions to determine what kind of dizziness, when it occurs: e.g., “Is it light headedness? Is there a sensation of motion (vertigo)? When standing up? When standing for long periods of time? Is it made worse with motion? On head turns? Is it constant or episodic (with definition/examples)? Etc.” The doctor reviews this data, it serves as a time, education, and communication bridge between doctors and patients, where there’s a huge gap. Can also help to teach patients to be more self aware, synthesize observations about, and better communicate their issues to health providers.
This could be powerful diagnostic aid, to help busy doctors, but they’d have to be well designed, and they could include algorithms for referral etc, especially when a symptom is reported that is beyond a generalist or other’s skill set. In short, some of the fallibility of humans, and human situations, can be carefully addressed and augmented with technology. This could help remove some tendency towards dismissiveness and bias, perhaps. A diagnostic aid such as this can also help level the playing field between new and experienced physicians, and perhaps even between generalists and specialists, at least in terms of better recognizing and knowing when to refer for specialized problems, and who the most relevant specialist is likely to be in “fuzzier” problems. I shouldn’t have had to figure this out on my own as a patient, so I could “calibrate” my language accordingly, and request the most relevant tests and specialist from physicians, but sadly, I’m 3/3 for having to do this on diagnoses I basically figured out myself, before I could get a physician to refer, test, or treat as needed. That’s not good.
I’ve experienced this my entire adult life by many doctors. It’s very frustrating and difficult to get second opinions at times so you’re stuck.
I do find all the information your provide to help me better self advocate for myself. I’m so thankful for your outreach to all of us!