Metabolic health
The evidence linking poor metabolic health to poor health outcomes is overwhelming and needs to be part of the holistic management of MS. Or should we ignore it and leave it up to others to manage?
I have finally squeezed my marginal gains philosophy and infographic for the holistic management of MS into an editorial commentary on CNS resilience that will be coming out in the next issue of ‘Multiple Sclerosis and Related Disorders’.
The more I practice medicine and neurology, the more I realise that we must move away from reactive medicine diagnosing and treating ill health and disease to preventive medicine, where we try optimising our general health. This concept is not new. Michael Marmot, the doyen of social determinants of health, came to this realisation as a junior doctor in the 1970s. The NHS, the WHO and many other health organisations are now espousing this approach.
As you can see from my latest version of the infographic, the central theme focuses on anti-ageing, emphasising brain, metabolic and social health. I have already discussed brain and social health and many non-MS therapeutic targets in the right panel in previous MS-Selfie podcasts and newsletters.
However, I have not spent much air time on metabolic health, which neurologists tend to delegate to general practitioners, family doctors or physicians. I take it for granted that you know about metabolic health and have already optimised your metabolism. Am I may be wrong?
Metabolic Health
Metabolism is the great integrator of what happens between your genome, epigenome and metagenome (microbiome) and the micro and macro environments you reside in. Without metabolic health, you can’t optimise MS outcomes. Metabolic health refers to optimal functioning and balance of your body's metabolic processes. It encompasses glucose regulation, lipid metabolism, hormone levels, and energy production. You can consider yourself metabolically healthy when these processes work efficiently. Metabolic health is essential for overall well-being, reducing your risk of chronic diseases and optimising MS outcomes.
One of the critical aspects of metabolic health is glucose regulation. This involves your body's ability to control blood glucose levels within a normal range. If you are metabolically healthy, you will have stable blood glucose levels without glucose spikes and crashes, which can be a harbinger of impaired glucose tolerance (pre-diabetes) and diabetes.
Lipid metabolism is another crucial component of metabolic health. It involves the breakdown, absorption, and utilisation of fats. If you have good metabolic health, you should have a balanced lipid profile with appropriate cholesterol levels, triglycerides and their associated lipoproteins. This is important in preventing the development of comorbidities, in particular cardiovascular and cerebrovascular disease.
Hormones also play a vital role in metabolic health. Hormones are your body's chemical messengers to regulate metabolism, growth, and reproduction. For optimal metabolic health, you have to have well-balanced hormone levels. Stress, for example, increases your circulating cortisone levels, which is associated with significant metabolic changes that, over the long term, increase your chances of poor health outcomes. Poor social determinants of health cause chronic stress and raised cortisol levels, which are associated with and may cause poor health outcomes.
Energy production is a fundamental aspect of metabolic health. Your body needs to generate and utilise energy from your food efficiently. A metabolically healthy person has a well-regulated energy metabolism, where the body's cells effectively produce, store, and utilise power. A marker of this is how well you utilise oxygen. Your VO2 max measures this, i.e. a marker of your cardiorespiratory fitness.
Metabolic health is a comprehensive measure of how well your body's metabolic processes function. Stable blood sugar levels, balanced lipid metabolism, optimal hormone levels, and efficient energy production characterise it. Maintaining metabolic health can lower your risk of chronic diseases, promote overall well-being, and improve your long-term MS outcome.
So how do you optimise metabolic health? You can do this via metabolic reprogramming, exercise, improving sleep, diet, supplements, and medication.
Metabolic reprogramming
Metabolic reprogramming refers to altering cellular metabolism in response to certain stimuli or conditions. It involves changes in how your cells utilise nutrients and generate energy to support various cellular processes. This process is crucial in normal physiological functions and pathological conditions like cancer.
Metabolism is the set of chemical reactions that occur within your cells to maintain them. It involves the conversion of nutrients into energy and synthesising various molecules necessary for cell growth and function. Metabolic reprogramming occurs when there is a shift in the balance of these reactions, leading to changes in cellular metabolism.
An example of metabolic reprogramming is the Warburg effect observed in cancer cells. Cancer cells preferentially utilise glucose via glycolysis, unlike normal cells, which primarily rely on oxygen-dependent oxidative phosphorylation for energy production. Glycolysis is a less efficient process that does not require oxygen. This metabolic shift allows cancer cells to generate energy and essential building blocks for rapid cell proliferation.
Metabolic reprogramming can also occur in response to environmental cues, such as nutrient availability or oxygen levels. For example, cells can switch from glucose metabolism to alternative fuel sources like fatty or amino acids during limited nutrient supply. Calorie restriction, ketogenic diets and intermittent fasting cause the body to switch from using glucose to fat and protein and, at the same time, alter many metabolic pathways, some of which are anti-inflammatory and may improve MS.
Furthermore, metabolic reprogramming is not limited to energy metabolism alone. It also affects other metabolic pathways, such as amino acid and lipid metabolism. These changes influence cell signalling, gene expression, and cellular stress responses, ultimately impacting cell fate and function. The science behind metabolic reprogramming is compelling and has significant implications for various fields, including inflammation, cancer, metabolic disorders, and drug development. By deciphering the mechanisms underlying metabolic reprogramming, we can develop targeted therapies that selectively disrupt the altered metabolic pathways in diseases like MS. For example, the fumarates (dimethyl fumarate and diroximel fumarate), licensed MS DMTs, probably work via metabolic reprogramming.
Exercise also works via metabolic reprogramming and profoundly impacts metabolic health.
Exercise
Regular physical activity helps regulate and improve various aspects of metabolism, leading to numerous health benefits. I have always said exercise is the least prescribed and most underutilised MS DMT available.
One of the critical effects exercise has on metabolism is its ability to increase insulin sensitivity. Regular exercise helps enhance insulin sensitivity, allowing cells to use glucose and maintain stable blood sugar levels efficiently. Exercise also helps maintain a healthy body weight, closely linked to metabolic health. Physical activity burns calories and contributes to weight loss or maintenance when combined with diet. Excess body weight, particularly abdominal or visceral fat, is associated with metabolic disorders such as insulin resistance, high blood pressure, and dyslipidemia. By reducing body fat and promoting muscle mass, exercise helps improve these metabolic parameters, reducing the risk of metabolic diseases.
Exercise stimulates the production of certain hormones that influence metabolism. For example, physical activity increases the release of growth hormone, which helps regulate your body composition, bone density, and muscle mass. It also activates the secretion of endorphins, which positively impact mood and overall well-being.
Regular exercise has been shown to have a positive effect on lipid profile as well. It helps increase high-density lipoprotein (HDL) cholesterol levels, often called "good" cholesterol, which is protective in heart health. At the same time, exercise reduces levels of low-density lipoprotein (LDL) cholesterol, also known as "bad" cholesterol, which is associated with an increased risk of cardiovascular diseases.
Moreover, exercise has been found to impact mitochondrial function directly, the powerhouses of our cells responsible for energy production. Regular physical activity stimulates mitochondrial biogenesis, leading to an increased number and improved mitochondria function. This enhances the body's energy efficiency, promoting overall metabolic health.
There is debate about which exercise is best for someone with MS. Recent evidence suggests HIIT (high-intensity interval training) is superior to moderate aerobic exercise. I have discussed the pros and cons of the different forms of exercise in the following three MS-Selfie Newsletters.
Sleep
Sleep also plays a crucial role in maintaining and improving metabolic health. Numerous studies have shown a strong correlation between sleep duration and quality and metabolic disorders such as obesity, diabetes, and cardiovascular diseases.
One of the primary ways sleep improves metabolic health is by regulating appetite and food intake. Lack of sleep disrupts the balance of hormones involved in hunger and satiety, such as ghrelin and leptin. Ghrelin, also known as the "hunger hormone," increases appetite, while leptin, the "satiety hormone," signals fullness. When sleep-deprived, ghrelin levels rise, leading to increased hunger and cravings, while leptin levels decrease, making it harder to feel satisfied. This imbalance often leads to overeating and weight gain.
In addition to appetite regulation, sleep also influences glucose metabolism. Lack of sleep affects insulin sensitivity. Sleep deprivation can decrease insulin sensitivity, making it harder for cells to respond to insulin signals and causing higher blood sugar levels. Over time, this can contribute to developing insulin resistance and type 2 diabetes.
Moreover, sleep deprivation has been linked to increased inflammation in the body. Chronic inflammation is associated with a higher risk of metabolic disorders, as it disrupts normal metabolic processes. Sleep helps to reduce inflammation and promote a healthier metabolic environment.
Furthermore, sleep deprivation can disrupt the circadian rhythm, the body's internal clock that regulates various physiological processes, including metabolism. Irregular or inadequate sleep patterns disrupt the circadian rhythm, leading to dysregulation of metabolic pathways and an increased risk of metabolic disorders.
Overall, sufficient and quality sleep is essential for optimal metabolic health. It helps regulate appetite, control blood sugar levels, reduce inflammation, and maintain a healthy circadian rhythm. By prioritising sleep and practising good sleep hygiene, pwMS can significantly improve their metabolic health and reduce the risk of metabolic disorders.
I have discussed MS sleep in the MS-Selfie Newsletter ‘Are you sleep-deprived?’ (18-Aug-2021).
Diet
Diet plays a crucial role in improving metabolic health. Making conscious choices about what you eat can positively impact your metabolism and improve overall health. Here are some ways in which diet can improve metabolic health. There is no single ‘MS Diet’ that is suitable for everyone. Diet needs to be individualised. If you haven’t done so, please read these two MS-Selfie Newsletters on diet.
Microbiota
The gut microbiota, also known as the gut flora, refers to the trillions of microorganisms in our digestive system. These microorganisms are crucial in maintaining our overall metabolic health. Numerous studies have shown that the composition and diversity of the gut microbiota can significantly impact our metabolism and influence the development of metabolic disorders.
The gut microbiota aids digestion and absorption of nutrients from our diet. It helps break down complex carbohydrates, fibres, and other indigestible substances our enzymes cannot process. In return, the gut microbiota produces short-chain fatty acids (SCFAs) as a byproduct, which serve as an energy source for our intestinal cells and have various metabolic benefits.
One of the critical ways the gut microbiota affects metabolic health is through its influence on energy balance. Certain species of gut bacteria have been found to extract more energy from the food we consume, leading to increased calorie absorption and potentially contributing to weight gain. Conversely, other bacteria may promote energy expenditure and assist in weight regulation. Alterations in the gut microbiota composition have been linked to obesity and metabolic disorders such as insulin resistance and type 2 diabetes.
Moreover, the gut microbiota plays a crucial role in regulating inflammation and immune responses. Chronic low-grade inflammation is a hallmark of metabolic disorders. Imbalances in the gut microbiota can affect intestinal function, potentially allowing harmful substances to enter the bloodstream and triggering immune responses. This chronic inflammation can disrupt insulin signalling and promote insulin resistance, contributing to the development of metabolic syndrome.
Additionally, the gut microbiota has been found to influence the production and regulation of hormones involved in appetite control and glucose metabolism. Specific gut bacteria can produce molecules interacting with the gut-brain axis, affecting our food cravings, satiety signals, and overall energy balance. Dysregulation of these hormonal pathways can lead to overeating, weight gain, and metabolic dysfunction.
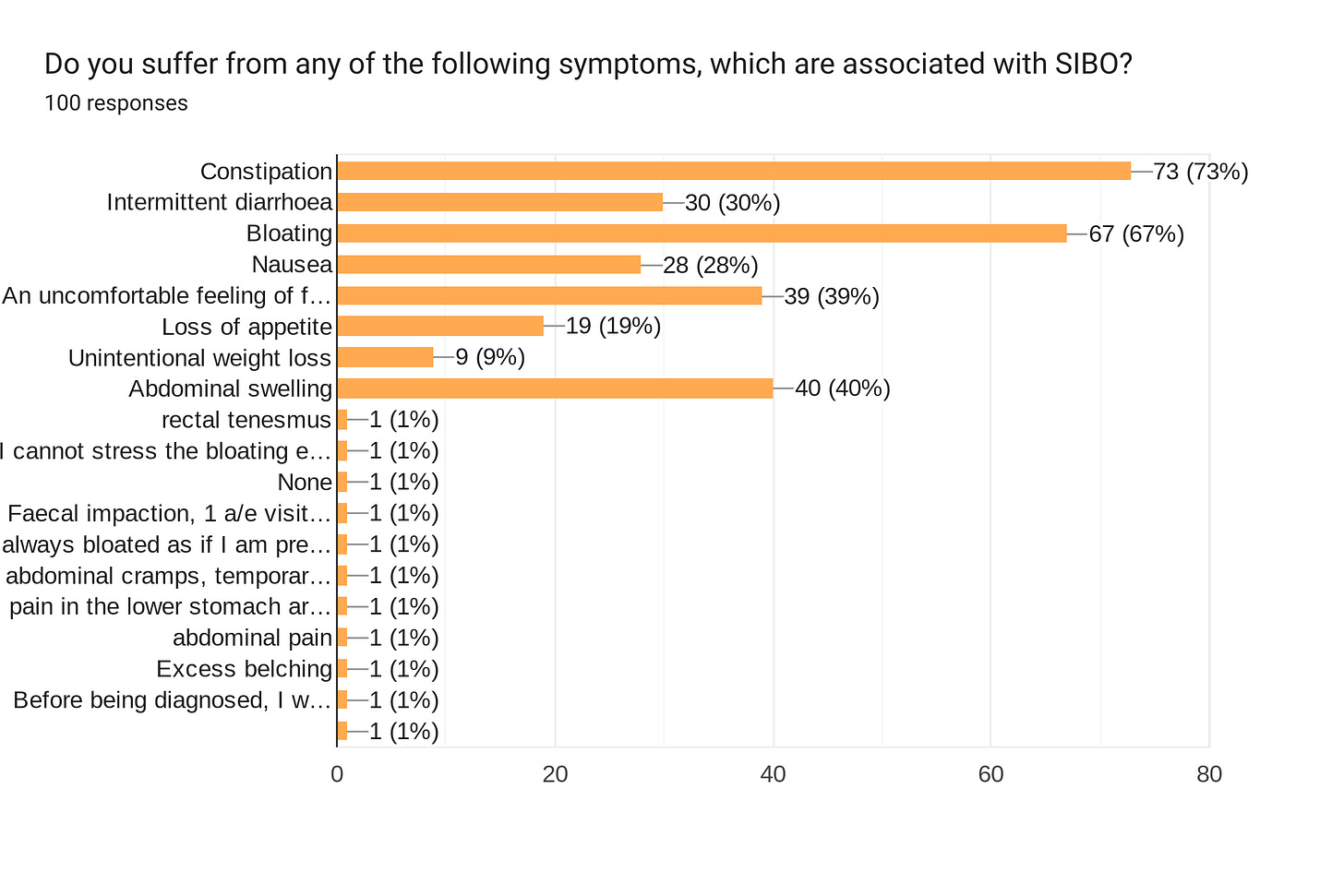
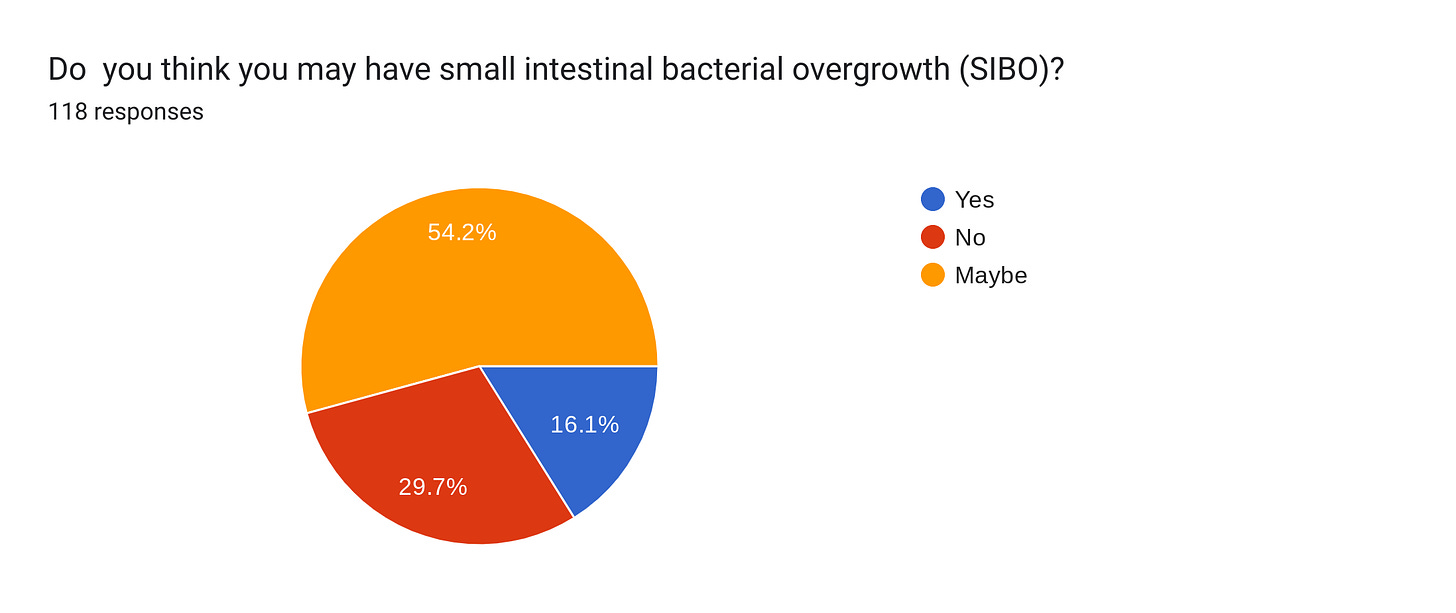
Maintaining a healthy and diverse gut microbiota through a balanced fibre-rich diet is essential for metabolic health. In the future, prebiotics and probiotics may help improve metabolic health and reduce the risk of metabolic disorders. Further research in this field is necessary to understand how gut microbiota affects metabolism, and MS. I recently did an MS-Selfie newsletter on gut health and included a survey. From the survey results, this gut health is another issue neglected in MS.
Most of you have bowel problems, with over 70% having symptoms suggestive of small intestinal bacterial overgrowth. We must do something about this in our MS practice to optimise gut and metabolic health and MS outcomes. Are you surprised by these results?
The SIBO survey is still open. For more information, please read the following newsletter.
Medications, supplements and procedures
Several medications have been found to promote metabolic health. Metformin, which is prescribed for the treatment of type 2 diabetes, is the most commonly prescribed. Metformin promotes remyelination in older animals and is currently being investigated in MS in several clinical trials. Other exciting medications include glucagon-like peptide-1 (GLP-1) receptor agonists (e.g. semaglutide), licensed for diabetes and obesity. They will almost certainly make their way into MS. In patients who are obese bariatric surgery not only results in weight loss but also improves metabolic health. I have seen this happen with a few of my patients.
Medications used to treat high cholesterol levels, such as statins, have also been show to benefit metabolism and may work as anti-inflammatories. Statins work by inhibiting the enzyme responsible for cholesterol production in the liver. In addition to lowering cholesterol levels, statins have been found to improve insulin sensitivity and reduce inflammation, contributing to better metabolic health. A phase 2 trial has shown that high-dose simvastatin may work in MS, prompting a significant phase 3 trial in the UK.
Another area is nutraceuticals, which can help reprogramme your metabolism. At present, it is hard to make firm recommendations. I have recently discussed this in an MS-Selfie Newsletter, which may be worth reading. From a scientific perspective, short-chain fatty acids that are either antioxidants or mimic ketosis are the most exciting for MS, i.e. alpha lipoic, propionic and butyric acid.
I would like to know how many of you actively try to improve your metabolic health as part of your MS management and how many have had this discussed with you by your MS team. The evidence linking poor metabolic health to poor health outcomes is overwhelming and needs to be part of the holistic management of MS. Or should we ignore it and leave it up to GPs or family doctors to manage?
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.









Not sure it is up to a particular health care pro in general. Three years ago before my recent series of relapse that resulted in a 18 month rollercoaster to get a diagnosis I had a vo2 max of 66 as a 45 year old male and resting heart of 42. As I started my first relapse that effected my physical health presenting to three different gps that my health wasn’t right and detailed evidence as a keen cyclist able to demonstrate issues in my right ankle through the pedal stroke they just thought I was crazy! Clonus identified on later inspection. And I was over reacting and obsessive about my body. Was an extremely keen cyclist. Now vo2 of 33 and unable to ride a bicycle and limited to walking about 1 mile. To know my heart rate over the years was described as neurotic by a thoracic consultant - just go out on your bike she said unbeknown to her or I that I was having my 3rd relapse 15 months. So to sum up, HCP need to recognise the value of wearable tech and not dismiss it! As if the largest company in the world would equip their Watch with a gimmick hr and Sat oxygen monitors! I demanded a referral to a neurologist privately from the 4 th gp as previously the rheumatologist I was recommended, agreed with the 3rd doctor that it was in my head! Which was in right ball park just needed to toss the net wider and just go with the central nervous system catch all. Sorry rant over. I guess I self managed my health and when I needed a professional was let down a bit. Even when going private. 😞
A really interesting read. My bowel is a constant Yo-yo of constipation and frequent pooping. I turned down the latest migraine injectables as it can cause constipation and a few folk were hospitalised in the trials. A Dr who called me to discuss my reasons did not really get it. How miserable bowel dysfunction is.
I have a healthy diet and fast for 15 hours most nights. I get the exercise I can but if I miss the window of opportunity earlier in the day I have no energy.
I’ve often wondered about child hood trauma/ abuse flooding the developing brain with cortisol’s and setting some of us up for diseases such as MS. I know many MSers won’t have had these experiences and it’s a very sensitive subject, but being in fight/ flight or freeze on a regular basis has to be bad for our physical developing bodies.