A question from one of the readers
Can you please explain why you think primary progressive multiple sclerosis (PPMS) is not different to relapsing-remitting MS (RRMS) or secondary progressive MS (SPMS)? And what has sliced salami got to do with the classification of MS?

Prof G’s Response
I may be repeating myself, but it needs to be said over and over again. A lot of people simply accept that (1) PPMS is non-inflammatory, (2) that people with PPMS don’t have relapses and (3) PPMS is a different disease from relapse-onset MS.
Dogma 1: PPMS in non-inflammatory – WRONG!
A pathology study done at the Institute of Neurology (Queen Square) when I was doing my PhD clearly showed, beyond doubt, that PPMS is inflammatory, albeit at a slightly lower level than SPMS. The dogma has crept in because we tend to view MS through the spectacles of an MRI; pwPPMS have fewer focal lesions on MRI. This, however, does not mean that there is no inflammation; focal inflammation is simply occurring at a level below the detection level of the MRI.
What an MRI sees about focal lesions is simply the tip of the iceberg. The PPMS iceberg simply looks different, with less above the surface. In addition, pwMS have oligoclonal IgG in their CSF. If they were not inflammatory, you would expect these OCBs to be absent or disappear.
Background: The dynamics of primary progressive multiple sclerosis differ from those of the more common secondary progressive form. The observation by MRI that the frequency of enhancement with gadolinium-DTPA, a marker for blood-brain barrier dysfunction, is significantly less in the primary progressive form has led to the hypothesis that inflammation is less intense in this group.
Aims: To test this, we have studied postmortem material from 9 cases judged from a retrospective analysis of case notes to show clear clinical evidence of either primary progressive or secondary progressive disease.
Methods: 578 lesions were analysed.
Results: There was significantly more inflammation in secondary progressive multiple sclerosis (as judged by the frequency of perivascular cuffing and cellularity of the parenchyma) than in primary progressive disease.
Conclusions: These observations have implications for therapeutic strategies in progressive multiple sclerosis.
Dogma 2: pwPPMS don’t have relapses – WRONG!
In almost all PPMS trials done to date, a proportion, albeit a small proportion, of pwPPMS go on to have relapses. For example, in the Rituximab trial in PPMS (Olympus Trial), 11 out of 439 (2.5%) study subjects had a relapse during 96 weeks. In the Ocrelizumab (ORATORIO) study, protocol-defined relapses were reported for 11% of subjects in the placebo group and 5% of subjects in the ocrelizumab group.
Similarly, about 5% of study subjects in the glatiramer acetate PPMS (PROMISE) trial had relapses. Unfortunately, the exact number of relapses is not reported in the main manuscript. What is reported is MRI activity; 14% of 938 study subjects had Gd-enhancing lesions on MRI during the study. The latter is the MRI equivalent of relapses.
Based on these data, can we say that PPMS is non-relapsing?
Dogma 3: PPMS is a different disease to SPMS – WRONG!
Did you know that it is not uncommon in siblings pairs with MS for one to have relapse onset disease and the other to have PPMS? The figure from the UK sibling study is 23% (please see the article and table below). This indicates to me that relapse onset and PPMS are the same disease.
(33.7+27) / (84+68.3+33.7+39.3+27+9.7) x 100 = 23%
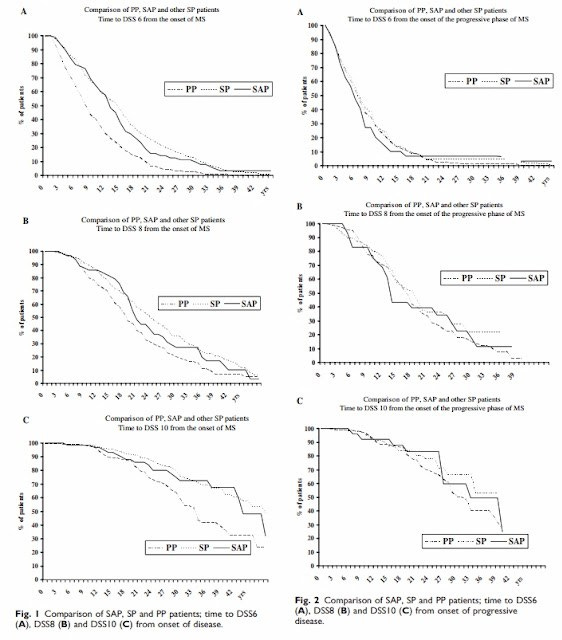
Other arguments favouring PPMS and SPMS being the same disease relate to genetic and natural history studies. People with PPMS and relapse-onset MSers have the same genetic background. Once people with relapse-onset MS enter the so-called clinical phase of SPMS, they progress at the same rate as pwPPMS.
What is different is that PPMS has an age of onset ten years later than relapse onset disease, i.e. ~39 years of age vs 30 years of age. This tells me that pwPPM simply miss out on the relapsing phase of the disease, i.e. they don’t have a sentinel event, a lesion in an eloquent pathway that brings them to the healthcare professional's attention. When you ask neuroradiologists to tell you the difference between relapse-onset MS and PPMS, they can’t differentiate them, which mirrors the pathology.
Interestingly, when you follow up people with radiologically-isolated syndrome or asymptomatic MS, about 85% develop RRMS and 15% PPMS mirroring what we see in patients with symptomatic MS. This latter observation is a powerful argument that MS is one disease.
The one difference that can’t be explained is that females predominate in relapse-onset disease, with a sex ratio of females to males of at least two-to-one or higher. In PPMS, the sex ratio is roughly one-to-one. This difference in the sex ratio may relate to the effect of female and/or male hormones on inflammation, but this is not known at present. When you look at epidemiological studies, it looks as if the incidence of PPMS is staying relatively constant with the incidence of relapse-onset disease increasing, manifesting in the changing sex ratio with more women getting MS than men. This is something that still needs to be adequately explained.
For the reasons above, there is a strong argument for trials on combined populations of progressive MS. We should combine PPMS and SPMS populations into one study. I know this is a controversial topic, particularly in the eyes of the regulators, but it needs serious debate. If we don’t do this, treatments will continue to be licensed for one subtype of progressive MS and not the other clinical subtype until additional trials are done. This is not in the interest of pwMS. Additional trials cost money and time. Time is not something people with progressive MS have on their side. Fiver years in the life of someone with progressive MS may be the difference between using a walking stick and becoming bed-bound.
When you go back to the basics and philosophical principles of classifying and defining diseases in medicine, you realise that dividing MS into three separate diseases or categories has no biological underpinnings. The only reason MS is now considered to be three, possibly four, diseases is that in 1988 the Chiron Corporation and Berlex Laboratories managed to get the Food and Drug Administration to accept that MS was an orphan disease. To be an orphan disease, fewer than 200,000 people have to be affected by the disease in the USA. The only way this was possible in the late 1980s was to salami slice up MS into relapsing-remitting, secondary progressive and primary progressive MS. Later, the entity of clinically isolated syndrome was added as a fourth entity. The mess we now find ourselves in, namely, trying to justify the clinical subtypes, has happened because we took a non-biological or pharmaceutical big business worldview of MS and not a biological view.
#MS_is_1_and_not_2_or_3_diseases
I also don’t think we should use the term progressive to describe MS anymore. Progression is a misnomer affecting how we classify and manage MS, but more on this topic another time.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.