Case study
Did stress trigger my latest relapse? Over the last 18 months, I have lost three close relatives and my job. I was made redundant during the second lock-down. I now live alone and spend most of my time thinking about the future, which looks very bleak. Three weeks ago I developed increasing weakness in my right leg associated with pins and needles down the front of the leg. My walking distance is now restricted to about 50m. My neurologist diagnosed me as having a relapse and prescribed high-dose oral steroids. Is there anything else I can do to prevent further relapses?

Prof G’s opinion
I often get asked whether or not stress can trigger MS relapses. I usually sit on the fence and quote an old meta-analysis that was published in the BMJ in 2004 (Mohr et al. BMJ. 2004 Mar 27;328(7442):731.) and the Israeli (Golan et al. Ann Neurol. 2008 Aug;64(2):143-8.) and Lebanese (Yamout et al. J Neurol Sci. 2010 Jan 15;288(1-2):42-4. ) war studies, which indicate that relapses and/or MRI activity are more likely to occur during periods of intense stress. However, the effect of stress on MS disease activity is quite small; maybe a 50% increase in the likelihood of relapse compared to periods not associated with stress. In addition, most of the studies above were done in the pre-DMT period and I suspect if you are on a DMT then the risk of stress triggering a relapse is much lower.
The above patient is on a platform therapy and I did recommend that she ask her neurologist to consider escalating her to a higher efficacy DMT. Being on a more effective therapy may give her more confidence about the future from an MS perspective.
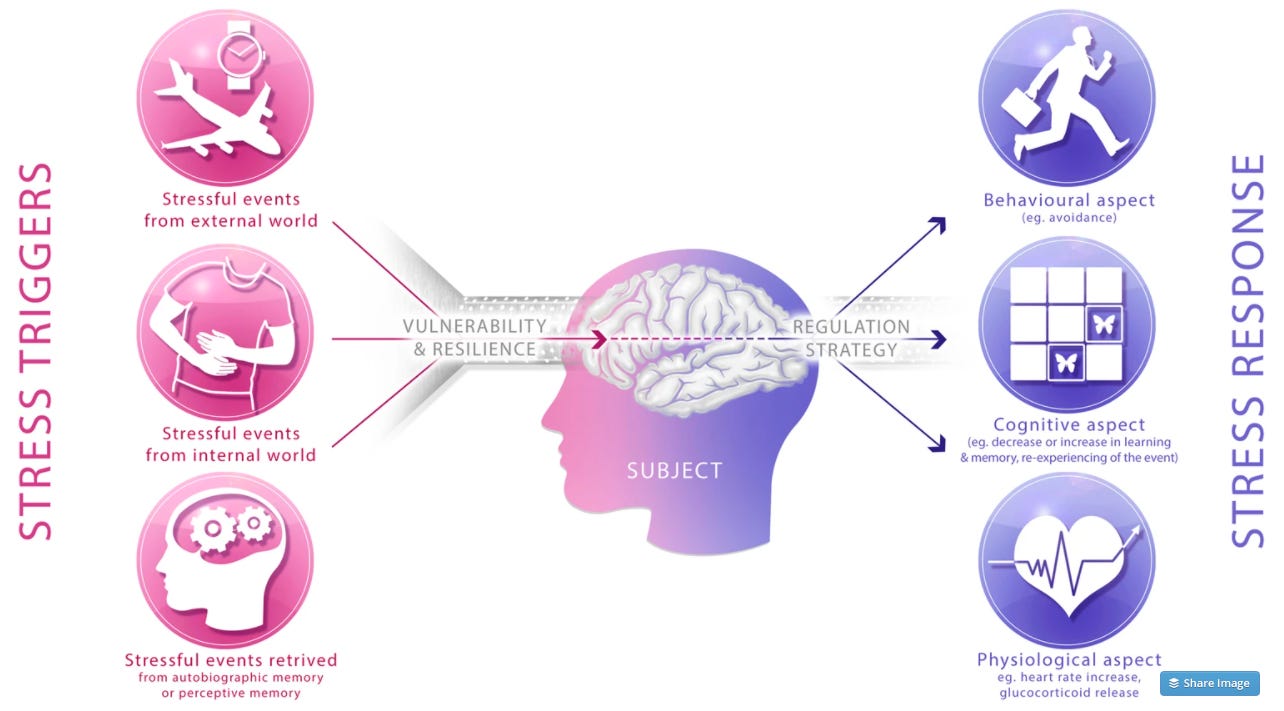
Please be aware that MS is not the only inflammatory disease that has been shown to be exacerbated by stress. Stress is not just a psychological phenomenon, it can be measured biologically. The stress response system is called the hypothalamic-pituitary-adrenal axis (HPA axis). After perceiving a stressor, an area in the brain called the hypothalamus sends a chemical message to the pituitary gland, which in turn produces a hormone called ACTH that travels via the blood and leads to stimulation of the adrenal glands to produce a stress hormone response. This leads to the secretion of adrenalin and cortisol. Adrenalin and cortisol then change the biology of every organ system in the body to optimise it to survive and get over the acute stress. However, If stress is chronic both these hormones have negative long-term effects on the body, including the immune system and in the patient above MS disease activity.
If stressful life events trigger relapses what can be done about it? Maybe pwMS could go a pre-emptive stress management course to give them the skills to counteract and manage stressful events, for example, CBT (cognitive behavioural therapy), mindfulness/meditation, yoga, exercise, talking therapy, counselling, etc.? The evidence base that any of these interventions make a big difference in preventing relapses and/or MRI activity in relation to stress is weak. Studying the impact of behavioural interventions on MS disease activity is always difficult. Just doing a power calculation to work out how many subjects you need to prove that a behavioural intervention, primarily designed to reduce stress, reduces relapses is a daunting task.
Despite this, there are compelling reasons for individuals to manage stress to improve their mental well-being and health. Please note that a life event or situation is only stressful if your brain interprets it as being stressful. For a situation to be stressful, you must feel it comprises novelty, unpredictability, is a threat to you or leaves you with a poor sense of control. The stress response in relation to a poor sense of control is how social determinants of health impact negatively on health outcomes. This poor woman who has lost her job and is now reliant on social support must feel she has no control over her future. She clearly needs additional help to deal with her loss of self-control.
Please note that stress is a personal reaction to a situation. What is novel or threatening to you may not be novel or threatening to someone else. Similarly, everyone deals with stress in different ways. Some people become withdrawn, others lash out, many develop anxiety and depression, sleeping and eating problems others misuse substances. Some people claim to thrive on stress. This is why there are no universal stress-management techniques and hence the need to personalise the management of stress.
Behavioural psychologists consider the stress response as being entirely appropriate from an evolutionary perspective to ensure our survival when we were hunter-gatherers. The stress response kept us alert and provided a survival advantage. Now that we live in an environment where existential threats to our lives are rare the stress response is maladaptive and causes long-term health problems.
I would be interested you hear if any of you have had any experiences with any stress management programmes you can share with us and this patient in particular? What worked and didn’t work for you? I know in the past many HCPs would often reach for the prescription pad and prescribe benzodiazepines (eg. diazepam or valium) to help with stress relief. Benzodiazepines only work for a short period of time and are highly addictive and HCPs now tend not to use them to manage stress. Saying that if the stressor is very acute the judicious use of anxiolytics can still be very helpful to manage an acute crisis.
Ukrainians with MS
My heart goes out to pwMS who are living in Ukraine. It is difficult to know what to say to them. I recall at the height of the Syrian crisis getting emails from desperate family members of pwMS living in refugee camps about the management of their MS. In general, refugees don’t have access to high-cost DMTs, which is one of the reasons I was promoting my essential list of DMTs to help manage their MS.
Not only will Ukrainian pwMS have concerns about the war and its impact on their lives, but they must be very concerned about how the war will disrupt their healthcare system and ultimately the management of their MS. I sincerely hope we in the UK and EU make an effort to ensure that Ukrainian people with chronic diseases such as MS don’t get neglected. I assume the aid charities, such as the Red Cross, have protocols in place to help people with chronic diseases in war zones. Does anyone know?
As a type this Newsletter I have a knot in my stomach when I think about the war in Ukraine and its consequences for the world. I think I need a stress management course myself.
Paper 1
Objective: To quantify the association between stressful life events and exacerbations of multiple sclerosis.
Data sources: PubMed, PsychInfo, and Psychological Abstracts searched for empirical papers from 1965 to February 2003 with terms “stress”, “trauma”, and “multiple sclerosis”.
Review methods: Three investigators independently reviewed papers for inclusion/exclusion criteria and extracted the relevant data, including methods, sample statistics, and outcomes.
Results: Of 20 studies identified, 14 were included. The meta-analysis showed a significant increase in the risk of exacerbation in multiple sclerosis after stressful life events, with a weighted average effect size of d = 0.53 (95% confidence interval 0.40 to 0.65), P < 0.0001. The studies were homogenous, Q = 16.62, P = 0.22, I2 = 21.8%. Neither sampling nor study methods had any effect on study outcomes.
Conclusions: There is a consistent association between stressful life events and subsequent exacerbation in multiple sclerosis. However, these data do not allow the linking of specific stressors to exacerbations nor should they be used to infer that pwMS are responsible for their exacerbations. Investigation of the psychological, neuroendocrine, and immune mediators of stressful life events on exacerbation may lead to new behavioural and pharmacological strategies targeting potential links between stress and exacerbation.
Paper 2
Objective: To assess the relationship between stress caused by the perils of rocket attacks on civilian centres in northern Israel during the 2006 war between Hezbollah and Israel and multiple sclerosis (MS) exacerbations.
Methods: Participants were 156 patients with relapsing-remitting MS. We compared the number of relapses during and after the war with similar time periods at the preceding year. Exposure to war events and resulting subjective stress were evaluated by means of structured interviews using questionnaires previously validated.
Results: During the 33 days of the war, there were 18 relapses among our patients, compared with 1 to 6 relapses in similar time periods over the 12 months before the war (p < 0.001-0.02). There was no increase in relapse rate during the 3 months that followed the war (p = 0.58). The percentage of patients reporting the experience of intense subjective stress during the hostilities was significantly greater among patients with wartime relapse compared with the rest of the patients (44 vs 20%). The proportion of patients reporting high levels of distress associated with exposure to rocket attacks, displacement from home, and perceived life threat was greater in relapsing patients compared with those in remission (67 vs 42%, p = 0.05; 33 vs 11%, p = 0.02; and 33 vs 15%, p = 0.08, respectively).
Interpretation: Our data suggest that civilian exposure to war stress is associated with an increased risk for MS relapse. These findings provide insight to stress-related risk factors associated with relapses of MS.
Paper 3
Objective: The relationship between stressful life events and multiple sclerosis (MS) exacerbations or radiological disease activity is at best controversial. The aim of this study is to examine the relationship between exposure to war-related events incurred during the July 2006 Israeli-Lebanese war and clinical relapses and MRI disease activity among Lebanese MS patients.
Methods: We studied a group of 216 patients with clinically definite relapsing-remitting MS (RRMS), on whom clinical data was available for the war period and for the preceding and following year(s). The number of relapses was determined during the war period and during similar periods over a 3-year span. All patients with brain MRI during the war period had their scans reviewed for evidence of disease activity as defined by the presence of gadolinium-enhancing (Gd+) lesions. A group of patients with brain MRI performed outside the war period was used for comparison.
Results: The total number of relapses during the war period (n=23) was significantly higher than during non-war periods (mean=8.4, SD=0.86) (p=0.006). Of the 18 patients with brain MRI during the war, 5/7 with relapses and 1/11 without relapses had Gd+ lesions (p=0.013). More patients had Gd+ lesions during the war period (33%) compared to controls (13%) (p=0.075).
Interpretation: Our study shows that exposure to war-related events is likely to lead to an increase in both clinical relapses and MRI disease activity in patients with MS.
Subscriptions
I am using the paid subscriptions to administer the MS-Selfie Newsletter and associated MS-Selfie microsite that is currently in development. If you are an active paying subscriber thank you, your contribution is much appreciated.
Funds from subscriptions are being used to pay a professional medical writer to curate, rewrite and transfer the contents of the Newsletter onto a companion MS-Selfie microsite, which is being designed and maintained by a freelance web designer.
If you find these Newsletters helpful and want the wider MS community to continue to have access to all content I would encourage you to become a paid subscriber.
Thank you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.












Share this post