Everyone is excited that licensed disease-modifying therapies (DMTs) reduce the risk of developing MS when started in patients with radiologically isolated syndrome (RIS). This has now been shown for DMF (dimethyl fumarate, Tecfidera) and teriflunomide (Aubagio). These trials have changed very little in my thinking about MS. I expected them to be positive. RIS is MS; therefore, if DMF and teriflunomide work in MS, they will work in RIS.
The concept that people with RIS do not have MS remains mainstream and is bizarre. MS is a biological disease and not a clinico-radiological construct, which is how we currently define the disease. If you think biologically, people with RIS have MS. If you biopsy their lesions, the pathologists will see the pathological hallmarks of MS. RIS is a misnomer and should be called asymptomatic MS.
Several KOLs (key opinion leaders) are concerned about creating a label of asymptomatic MS because not all will have a clinical event and develop MS; hence if we treated them, we would be over-treating MS and exposing them to the harms of DMTs (e.g. DMF or teriflunomide). They also argue that a diagnosis of MS is stigmatising and has implications beyond having a disease.
I am unsurprised that not all patients with RIS or asymptomatic MS go on to have a clinical event. At post-mortem, an estimated 25% of people with pathological features of the disease were never diagnosed in life. This means they had either never had symptoms or their symptoms were mild and/or atypical and never triggered a diagnostic work-up. Similarly, when you scan first-degree relatives or siblings of someone with MS, you find that about 10% have suspicious lesions compatible with demyelination. In twins, this is higher. However, only one in four of these siblings go on to have a clinical event to be diagnosed with CIS (clinically isolated syndrome) or MS. Therefore, a significant proportion of people who have biological MS don’t go on to develop relapsing or primary progressive MS. Could their immune systems be self-correcting or clearing the cause of MS; i.e. are they curing themselves of MS?
To explain this, I will use a counterfactual and claim that MS is due to a mutant virus, for example, a mutant strain of EBV (Epstein Bar virus). The mutant strain initiates the MS disease process. However, before the damage presents clinically, the immune system identifies the virus, mounts an immune attack and clears the virus. We have several analogies to back this up. It can happen with PML (progressive multifocal leukoencephalopathy). There are many spontaneous PML cures due to the immune system clearing the virus. Similarly, in oncology, tumours can spontaneously regress or disappear, presumably due to the immune system killing the tumour. These disappearing or vanishing tumours underpin immuno-oncology and the use of immunotherapy to treat cancer. This is why I am a big supporter of using EBV vaccines as immunotherapies in established MS. By boosting immunity to EBV with a vaccine, can we treat MS? Can we cure MS?
I posit that not all people with asymptomatic MS go on to have a clinical event because their immune systems are finding and clearing the virus that causes MS.
Are all these people with asymptomatic MS truly asymptomatic?
Unfortunately, not. You find neurological deficits when interrogating subjects with RIS using neurological stress tests. Approximately a quarter will have cognitive impairment in at least two domains, and many will have subtle deficits in fine motor function. Some will develop fatiguable weakness and gait problems when they exercise on a treadmill. Many will also have non-specific symptoms such as fatigue. The question is, how hard do you want to look for deficits? I have been referred several patients with a label of RIS. However, when I asked probing questions and examined these patients, most had symptoms and signs compatible with demyelinating lesions affecting a particular neuronal pathway.
Lost opportunity
It is a pity these RIS studies were not done with a safe IRT (immune reconstitution therapy) such as cladribine. I have argued that IRTs are the only realistic treatment strategy to offer people with MS a possible cure. Would it not be great to show that you can increase the chances of someone with RIS never developing further lesions or clinical signs despite not being on a treatment? In other words, can you cure biological MS? There is a strong rationale for moving the treatment of MS with IRT as early as possible in the disease course to maximise the treatment effect, to protect the brain and spinal cord and to try and prevent the processes that drive smoldering MS setting-up shop in the CNS causing smoldering pathology.
Some of you may know about the ORACLE study, where oral cladribine reduced the chances of someone presenting with CIS having a second attack (study 3 below). We presented the long-term follow-up results of these trial subjects at the AAN 2023 in Boston. Remarkably 53% of CIS patients treated with cladribine had not had another event on average 9.5 years after the end of the ORACLE study, i.e. close to 12 years after their initial event. In comparison, only 28% of subjects randomised to the placebo arm did not have an event. The billion-dollar question: ‘Did early treatment with oral cladribine cure most of these subjects with CIS?’.
I have been heavily criticised by my colleagues in the past for using the C-word and for daring to suggest that one day we may be able to cure someone who has MS. I think we may have already cured a cohort of pwMS who have had an early IRT (cladribine, alemtuzumab or AHSCT). My retort is, indeed, if our aim is not to cure MS, we should give up now. Do you agree? If we don’t define a cure and look for it, we will never find it.
Anti-CD40L (Frexalimab)
The discussion about an MS cure is very relevant right now. We will start testing a monoclonal antibody targeting anti-CD40 ligand, frexalimab, in phase 3 MS trials. The CD40-CD40L pathway, which I have discussed before, is critical in driving MS and autoimmune diseases in general. If MS is an autoimmune disease blocking this pathway may allow the immune system to reset itself and become tolerant once more to the antigens or proteins driving MS autoimmunity. From an immunological perspective, this will be like curing MS. If we can show frexalimab resets immune tolerance, i.e. reprograms the immune system, so as not to cause autoimmune disease, pwMS may not need to be treated with frexalimab long-term. The challenge is defining an immunological cure and then how we look for it in the clinical trials. Do any of you have any suggestions? I have already spent hundreds of hours thinking about this.
Stigmatisation
Finally, as for the point about MS being a stigmatising disease and that we should not be diagnosing someone with asymptomatic MS for this reason. Now that we have treatments for asymptomatic MS, this argument falls away. Knowing what we know about MS, who would want someone to continue to have their brain and spinal cord shredded by MS when we can prevent the damage from accumulating? In addition, the better we treat and manage MS, the less stigmatising the disease will become. If, in the near future, we show we can cure MS in 75% of patients with RIS using oral cladribine, but the cure rate drops to 50% when we start cladribine at the CIS stage and 25% at the relapsing-remitting or 10% at the primary progressive phase*. Who wouldn’t want to be labelled as having MS as early as possible? If I had RIS, I would want to be treated with two full courses of cladribine.
* please note that 10-15% of people with RIS will present with primary progressive MS, i.e. they don’t have events and hence get diagnosed much later.
If you are interested in reading about frexalimab, I cover it in my MS-Selfie Newsletter from the CMSC 2023 (‘Breaking news: we have a new therapeutic target in MS’, 31-May-2023).
Paper 1
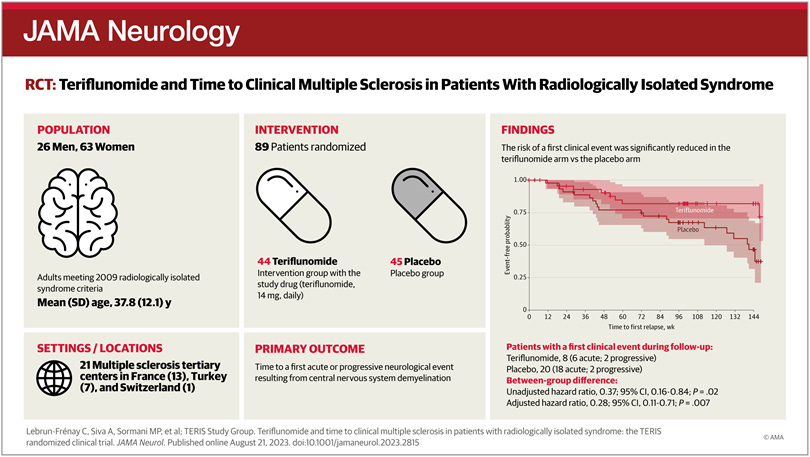
Importance: Radiologically isolated syndrome (RIS) represents the earliest detectable preclinical phase of multiple sclerosis (MS) punctuated by incidental magnetic resonance imaging (MRI) white matter anomalies within the central nervous system.
Objective: To determine the time to onset of symptoms consistent with MS.
Design, setting, and participants: From September 2017 to October 2022, this multicenter, double-blind, phase 3, randomized clinical trial investigated the efficacy of teriflunomide in delaying MS in individuals with RIS, with a 3-year follow-up. The setting included referral centers in France, Switzerland, and Turkey. Participants older than 18 years meeting 2009 RIS criteria were randomly assigned (1:1) to oral teriflunomide, 14 mg daily, or placebo up to week 96 or, optionally, to week 144.
Interventions: Clinical, MRI, and patient-reported outcomes (PROs) were collected at baseline and yearly until week 96, with an optional third year in the allocated arm if no symptoms have occurred.
Main outcomes: Primary analysis was performed in the intention-to-treat population, and safety was assessed accordingly. Secondary end points included MRI outcomes and PROs.
Results: Among 124 individuals assessed for eligibility, 35 were excluded for declining to participate, not meeting inclusion criteria, or loss of follow-up. Eighty-nine participants (mean [SD] age, 37.8 [12.1] years; 63 female [70.8%]) were enrolled (placebo, 45 [50.6%]; teriflunomide, 44 [49.4%]). Eighteen participants (placebo, 9 [50.0%]; teriflunomide, 9 [50.0%]) discontinued the study, resulting in a dropout rate of 20% for adverse events (3 [16.7%]), consent withdrawal (4 [22.2%]), loss to follow-up (5 [27.8%]), voluntary withdrawal (4 [22.2%]), pregnancy (1 [5.6%]), and study termination (1 [5.6%]). The time to the first clinical event was significantly extended in the teriflunomide arm compared with placebo, in both the unadjusted (hazard ratio [HR], 0.37; 95% CI, 0.16-0.84; P = .02) and adjusted (HR, 0.28; 95% CI, 0.11-0.71; P = .007) analysis. Secondary imaging end point outcomes including the comparison of the cumulative number of new or newly enlarging T2 lesions (rate ratio [RR], 0.57; 95% CI, 0.27-1.20; P = .14), new gadolinium-enhancing lesions (RR, 0.33; 95% CI, 0.09-1.17; P = .09), and the proportion of participants with new lesions (odds ratio, 0.72; 95% CI, 0.25-2.06; P = .54) were not significant.
Conclusion and relevance: Treatment with teriflunomide resulted in an unadjusted risk reduction of 63% and an adjusted risk reduction of 72%, relative to placebo, in preventing a first clinical demyelinating event. These data suggest a benefit to early treatment in the MS disease spectrum.
Trial registration: ClinicalTrials.gov Identifier: NCT03122652.
Paper 2
Objective: The radiologically isolated syndrome (RIS) represents the earliest detectable pre-clinical phase of multiple sclerosis (MS). This study evaluated the impact of therapeutic intervention in preventing first symptom manifestation at this stage in the disease spectrum.
Methods: We conducted a multi-center, randomized, double-blinded, placebo-controlled study involving people with RIS. Individuals without clinical symptoms typical of MS but with incidental brain MRI anomalies consistent with central nervous system (CNS) demyelination were included. Within 12 MS centers in the United States, participants were randomly assigned 1:1 to oral dimethyl fumarate (DMF) 240 mg twice daily or placebo. The primary endpoint was the time to onset of clinical symptoms attributable to a CNS demyelinating event within a follow-up period of 96 weeks. An intention-to-treat analysis was applied to all participating individuals in the primary and safety investigations. The study is registered at ClinicalTrials.gov, NCT02739542 (ARISE).
Results: Participants from 12 centers were recruited from March 9, 2016, to October 31, 2019, with 44 people randomized to dimethyl fumarate and 43 to placebo. Following DMF treatment, the risk of a first clinical demyelinating event during the 96-week study period was highly reduced in the unadjusted Cox proportional-hazards regression model (hazard ratio [HR] = 0.18, 95% confidence interval [CI] = 0.05-0.63, p = 0.007). More moderate adverse reactions were present in the DMF (34 [32%]) than placebo groups (19 [21%]) but severe events were similar (DMF, 3 [5%]; placebo, 4 [9%]).
Interpretation: This is the first randomized clinical trial demonstrating the benefit of a disease-modifying therapy in preventing a first acute clinical event in people with RIS. ANN NEUROL 2023;93:604-614.
Paper 3
Background: Patients who develop relapsing-remitting multiple sclerosis (MS) present with a first clinical demyelinating event. In this double-blind, multicentre, randomised, phase 3 study we investigated the effect of oral cladribine on conversion to clinically definite MS in patients with a first clinical demyelinating event, when given at the same doses shown to be effective in relapsing-remitting MS.
Methods: Between Oct 21, 2008, and Oct 11, 2010, we recruited patients aged 18-55 years, inclusive, from 160 hospitals, private clinics, or treatment centres in 34 countries. Eligible patients had a first clinical demyelinating event within 75 days before screening, at least two clinically silent lesions of at least 3 mm on a T2-weighted brain MRI scan, and an Expanded Disability Status Scale score of 5.0 or lower. Patients with a first clinical demyelinating event ≤75 days before screening were randomly assigned (1:1:1) to receive cladribine tablets at cumulative doses of 5.25 mg/kg or 3.5 mg/kg or placebo. Randomisation was done with a central web-based randomisation system and was stratified by geographic region. Masking was maintained using a two-physician model. The primary endpoint of this 96-week study was time to conversion to clinically definite MS according to the Poser criteria. This study is registered with ClinicalTrials.gov, number NCT00725985.
Findings: Of 903 participants assessed for eligibility, 616 patients received cladribine 5.25 mg/kg (n=204), cladribine 3.5 mg/kg (n=206), or placebo (n=206). At trial termination on Oct 25, 2011, cladribine was associated with a risk reduction versus placebo for time to conversion to clinically definite MS (hazard ratio [HR] for 5.25 mg/kg=0.38, 95% CI 0.25-0.58, p<0.0001; HR for 3.5 mg/kg=0.33, 0.21-0.51, p<0.0001). Adverse events were reported in 165 (81%) patients in the cladribine 5.25 mg/kg group, 168 (82%) patients in the cladribine 3.5 mg/kg group, and 162 (79%) patients in the placebo group. We noted no increase in risk of adverse events with active treatment versus placebo apart from lymphopenia, which was a severe event in 10 (5%) patients in the 5.25 mg/kg group and four (2%) patients in the 3.5 mg/kg group.
Interpretation: Both doses of cladribine significantly delayed MS diagnosis compared with placebo. The safety profile of cladribine was similar to that noted in a trial in patients with relapsing-remitting MS. Further research could clarify the potential effects of oral cladribine treatment in the early stages of MS.
Funding: Merck Serono SA Geneva, a subsidiary of Merck KGaA, Darmstadt, Germany.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite, which is now open to all readers. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription to subscribe. For active paying subscribers, thank you; your contribution is much appreciated. Because of the falloff in paying subscribers, I am considering returning to a paywall that will give paying subscribers six months of unlimited access to all newsletters. At the same time, free subscribers will have a wait to access the newsletters later, not as an email, but on the substack site.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your own healthcare professional, who will be able to help you.















Share this post