I have been running a campaign that #MS_is_1_not_2_or_3_diseases for sometime. This is based on the biology of MS and not what we see clinically. The pathology that underpins so-called progressive MS is the loss of axons, neurons and synapses. All three of these processes begin very early in the so-called asymptomatic stage of MS. What dictates whether or not we see the effects of these subtle changes depends on how much we stress the neurological system concerned and how much resilience, or reserve, this system has to handle the stress.
A good example is a patient of mine with MS who was a marathon runner. His first symptoms of MS was when he developed a dropped foot after running for about an hour at his typical marathon race pace. A year earlier he would only notice that symptom towards the end of the marathon. Does this marathon runner have SPMS? If he had not stressed his motor pathway with vigorous competitive exercise the issue of whether or not he has SPMS would not arise. In other words, the question of SPMS would only arise when his dropped foot would impact normal activities of daily living, for example walking, which may only occur in 10 years' time if he stops running.
This anecdote tells us that the diagnosis of SPMS is a moving target and depends on what system, or systems, MS has affected, how you use that system and how much reserve is left in that system to compensate for the damage. The study below shows how we can use a neurological stress test, for example, exercise-induced gait deterioration (foot drop), detected with gait analysis, in pwMS with minimal neurological disability and so-called ‘stable disease’ to monitor subtle neurological deficits from an early stage of MS. Essentially this is detecting progressive MS pathology early on in the course of the disease.
#ThinkCognition
We know progressive cognitive dysfunction is the driver of early unemployment in the so-called knowledge economy. Why aren’t these people with MS being labelled as having SPMS? That is because neurologists, first and foremost, view MS as a physically disabling disease rather than a cognitively disabling disease. This needs to change. Hence our ongoing #ThinkCognition campaign.
The diagnosis of SPMS is therefore in the eye of the beholder. In my eyes, progressive MS is present from the beginning of the disease. Trying to identify a point in time when you can be diagnosed with SPMS is futile and to discuss transitioning MS is a misnomer. Neurologists think we are smart when we classify our patients as having relapsing-remitting MS, relapsing SPMS, or non-relapsing SPMS. To be brutally honest this is a fallacy.
The problem the MS community faces is that we view MS through clinical and MRI spectacles and we don’t think about the biology of the disease. If we took a biological approach to MS all MS would be labelled as being inflammatory, all MS would probably be classified as being active and all MS would be progressive. Based on this thinking all MS needs to be treated with a combination therapy approach and treated holistically.
In the UK once you are labelled as having SPMS you are meant to stop DMTs and siponimod can only be offered to treat SPMS if the patient has ‘active-SPMS’, i.e. they have to have a recent relapse and/or MRI activity in the last 2-3 years. Even if a patient is labelled as having active-SPMS and start siponimod and they then have to stop taking it because of lack of efficacy, poor tolerance or an adverse event. The current Lublin classification system we use in trials and clinical practice is quite clear that once someone’s MS becomes secondary progressive they can move back to be relapsing-remitting.
Saying this I have many examples of my colleagues recategorising patients from being secondary progressive back to relapsing MS so that they can put them back on a DMT that is licensed for relapsing MS. I call this flip-flopping and it happens all the time in clinical practice. However, NHS England has put in place systems on its high-cost DMT database (blueteq) to prevent this from happening.
Could I suggest getting rid of these labels and letting the neurologist and the patient decide on what treatment they want?
I have tried to capture the thoughts above in our recent paper on Smouldering MS. Please read it as it explains why pwMS get worse despite being NEIDA (no evident inflammatory disease activity) and builds on my previous MS-Selfie Newsletter ‘Getting worse’ (2-Jul-2021).
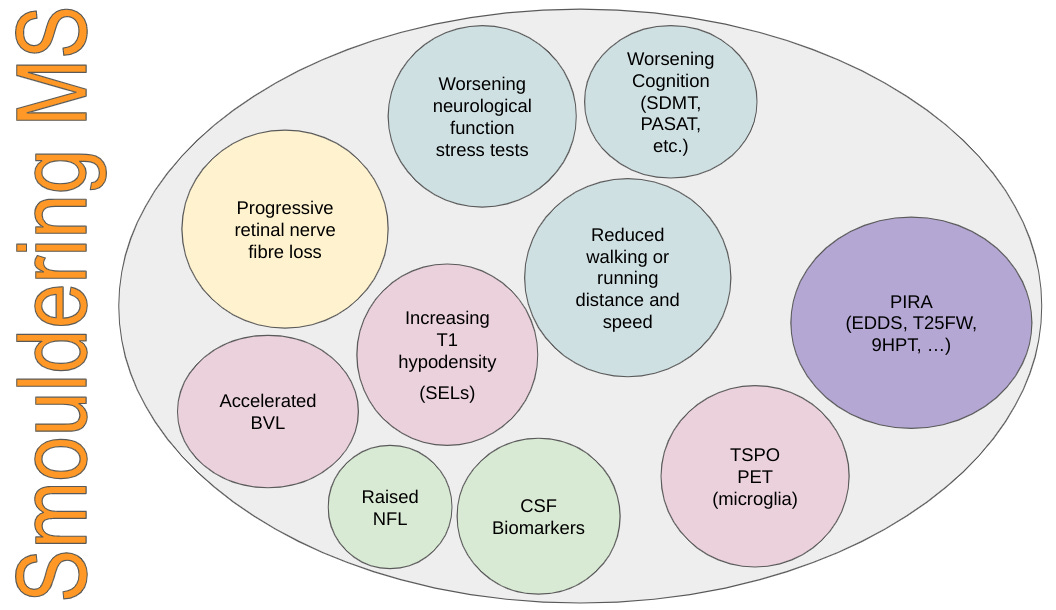
Since writing this paper I have been getting some pushback about the term smouldering MS. Some people don’t like the term and prefer the term PIRA (progression independent of relapses). The problem I have is that PIRA is a derivative of the EDSS from trials and doesn’t capture other components of the disease such as retinal nerve fibre loss, brain and grey matter volume loss, cognitive impairment, and worsening using neurological stress tests. Smouldering also refers to the pathology of the disease and processes that can be measured in the spinal fluid or blood. Smouldering MS is so much more than PIRA.
If you have the time I would appreciate it if you could VOTE on what term you prefer to describe smouldering MS or some other name?
Paper 1
Andreopoulou et al. Exercise-induced changes in gait kinematics in multiple sclerosis with minimal neurological disability. Mult Scler Relat Disord. 2021 Jan;47:102630.
Background: Exercise-induced gait deterioration is a frequently encountered symptom that limits ambulation throughout the clinical course, becoming more prominent with increasing neurological disability in people with MS (pwMS).
Objective: We attempted to objectively document exercise-induced gait changes in pwMS with minimal neurological disability and stable disease.
Methods: Gait kinematics and spatio-temporal parameters were recorded using 3D motion analysis before and after a 20-minute treadmill walk (Group A, n=15)/run (Group B, n=15) at a self-selected speed in pwMS and compared with healthy controls (n=15).
Results: Gait analysis revealed a significant decrease in peak ankle dorsiflexion in swing of the most affected leg, post-exercise task, in both Group A (EDSS 2.5-3.5) and Group B (EDSS 1-2.5) and not in healthy controls. Fourteen out of 30 MS participants showed an exercise-induced gait deterioration, based on minimal detectable change. Pre-exercise gait parameters in Group A showed a significantly higher peak dorsiflexion in swing with shorter step length and higher cadence, whereas Group B was comparable to healthy controls.
Conclusion: The detection of exercise-induced gait deterioration (foot drop) in pwMS with minimal neurological disability and stable disease indicates the potential of gait kinematics, before and after an exercise task, to monitor subtle neurological deficits from an early stage of MS.
Paper 2
Giovannoni et al. Smouldering multiple sclerosis: the 'real MS'. Review Ther Adv Neurol Disord. 2022 Jan 25;15:17562864211066751.
Using a philosophical approach or deductive reasoning, we challenge the dominant clinico-radiological worldview that defines multiple sclerosis (MS) as a focal inflammatory disease of the central nervous system (CNS). We provide a range of evidence to argue that the 'real MS' is in fact driven primarily by a smouldering pathological disease process. In natural history studies and clinical trials, relapses and focal activity revealed by magnetic resonance imaging (MRI) in MS patients on placebo or on disease-modifying therapies (DMTs) were found to be poor predictors of long-term disease evolution and were dissociated from disability outcomes. In addition, the progressive accumulation of disability in MS can occur independently of relapse activity from early in the disease course. This scenario is underpinned by a more diffuse smouldering pathological process that may affect the entire CNS. Many putative pathological drivers of smouldering MS can be potentially modified by specific therapeutic strategies, an approach that may have major implications for the management of MS patients. We hypothesise that therapeutically targeting a state of 'no evident inflammatory disease activity' (NEIDA) cannot sufficiently prevent disability accumulation in MS, meaning that treatment should also focus on other brain and spinal cord pathological processes contributing to the slow loss of neurological function. This should also be complemented with a holistic approach to the management of other systemic disease processes that have been shown to worsen MS outcomes.
Figure 3. The pathological drivers of smouldering MS. Apart from acute focal damage characterised by axonal transection and conduction block that occurs over days to weeks and causes relapse-associated worsening (RAW), there are delayed time-dependent processes that are responsible for smouldering MS. Demyelination and energy deficits are responsible for delayed worsening, which occurs over weeks to months. Whether this is dependent or independent of ongoing focal inflammation is a moot point. This is then followed by post-inflammatory neurodegenerative processes, which run their course over many years and include microglial and innate immune mediators, ongoing energy deficits, antibody-mediated damage, and possible viral infection. Finally, age-related neurodegenerative processes that are premature and accelerated are responsible for late-onset disability progression, which plays out over decades.
Subscriptions and donations
I am using the paid subscriptions to administer the MS-Selfie Newsletter and associated MS-Selfie microsite that is currently in development. If you are an active paying subscriber thank you, your contribution is much appreciated. At the request of several readers, I have now added the option of making a one-off donation as well. Funds from subscriptions and donations are being used to pay a professional medical writer to curate, rewrite and transfer the contents of the Newsletter onto a companion MS-Selfie microsite, which is being designed and maintained by a freelance web designer.
Thank you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.

















Share this post