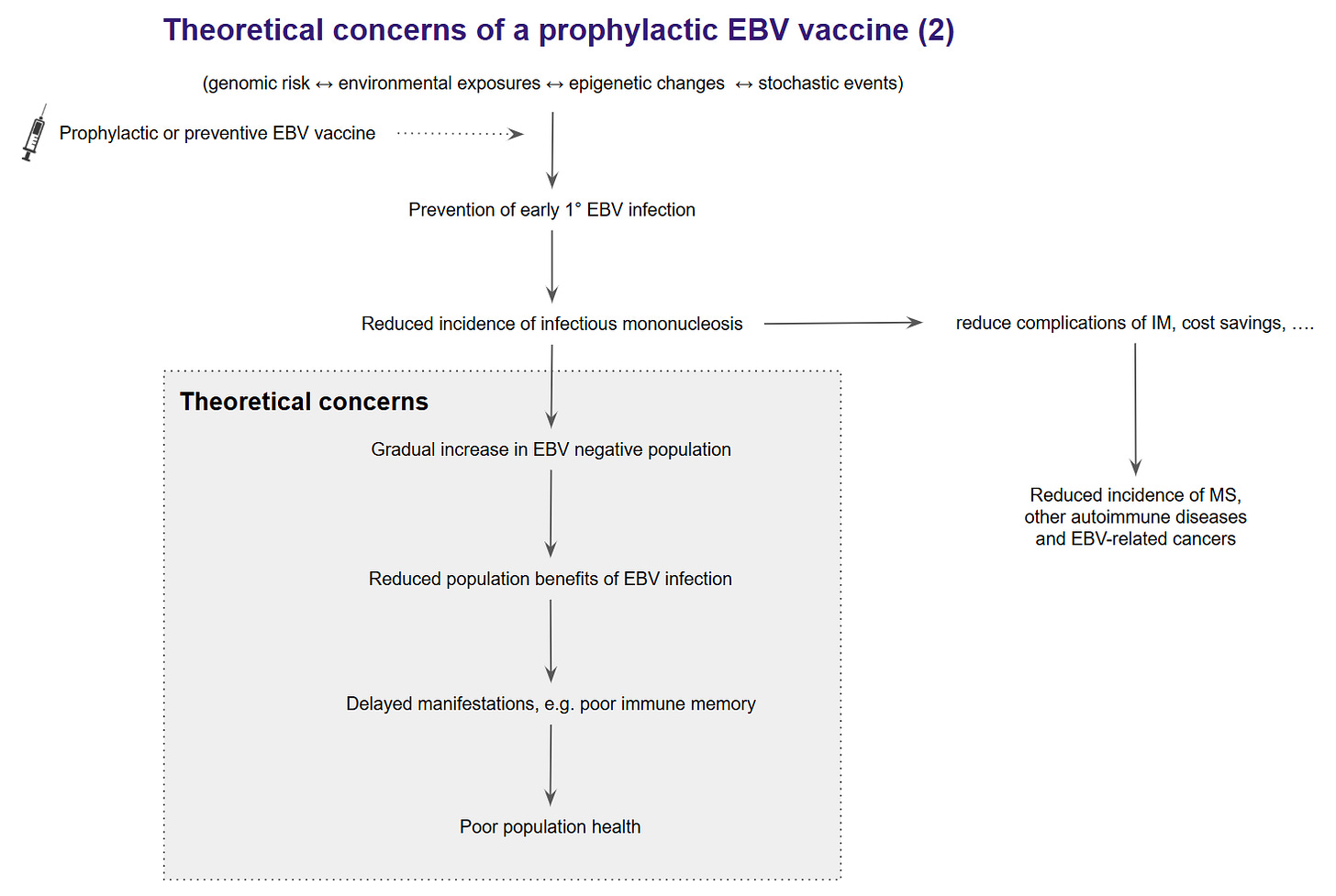
The current dogma that is emerging in the field of immunology and multiple sclerosis (MS) is that a prophylactic EBV vaccine will create an older population of individuals susceptible to later wild-type EBV infection as vaccine immunity wanes. Therefore, instead of reducing the risk of MS, the vaccine will increase the risk. I don’t necessarily agree with this position. The arguments supporting their claims are very nuanced and, at present, are not evidence-based. Yes, we need to have concerns and be prepared to address them once an EBV vaccine gets approved and adopted for general use. We cannot let a theoretical concern stop an essential experiment designed to prove or disprove that EBV is the cause of MS, other autoimmune diseases and several human cancers. Do you agree?
For more information on the EBV vaccine experiment, please read my newsletter, ‘Preventing multiple sclerosis by vaccination’ (22-Jan-2025).
The theory
The theoretical consideration that waning immunity to an EBV vaccine may increase the risk of MS is based on the observation that delayed EBV, particularly symptomatic EBV in the form of infectious mononucleosis (IM), is the main EBV-associated risk factor for developing MS. Delayed EBV infection remains a risk factor lifelong and doesn’t disappear after adolescence or early adulthood.
In the UK, the Health Improvement Network (THIN) Database uses data from the NHS as part of routine care. A recent analysis commissioned by the MS Society estimated that the lifetime risk of developing MS in the UK is approximately 1 in 330.
These risks could be refined further with better prediction calculators, including a history of IM, antibody titres to the ENBA complex or EBNA-1, other risk factors, and polygenic risk scores. However, EBV and IM are the most significant modifiable MS risk factors at a population level. We know that for EBV-negative individuals (5% of the adult population), the risk of developing MS is close to zero. For people who have EBV-associated IM, the lifetime risk of MS is approximately 1 in 100. For people who seroconvert to becoming EBV-positive without a history of IM, the risk is approximately 1 in 800. Therefore, in addition to preventing infection with EBV, preventing IM and potentially treating IM need to be explored as preventive MS strategies.
We don’t know how EBV causes MS and why the risks are higher in people who have symptomatic infection or IM compared to those who seroconvert asymptomatically. The hypothesis is that something happens from an immunological perspective during IM that triggers MS. Many immunologists think the overzealous immune response during IM dysregulates immune function, which leads to autoimmunity later on. Others feel that because of the poor control of the virus during IM, the immune system reacts to many more EBV antigens, making molecular mimicry more likely to occur. Another theory is that autoimmunity is bad luck due to rogue B-cells. During IM, more B-cells are infected with EBV due to higher and more prolonged EBV viral loads. This increases the chances of a B-cell being self-reactive, which then causes MS. The latter is a random event, and the chances are much higher in people with IM, which may explain why IM is associated with several autoimmune diseases. Finally, some think that IM is an epiphenomenon and that what predisposes someone to IM is the same phenomenon that increases one's risk of getting MS, i.e. IM is simply an association and is not in the causal pathway of MS. The latter hypothesis doesn’t explain why EBV seronegative people don’t get MS, nor does it explain the temporal sequence of needing to be infected with EBV before you develop MS. I rejected the last hypothesis years ago, however, what seems obvious to me doesn’t seem obvious to others. I often have to point out to colleagues that causation theory has eliminated that hypothesis.
The reason I am spending so much time explaining all of this to you is that if an EBV vaccine reduces your risk of getting IM, it may reduce your risk of getting MS. In other words, the vaccine doesn’t have to be sterilising. This is why it is essential to see if an EBV vaccine that reduces the incidence of IM but not necessarily wild-type EBV infection reduces the risk of getting MS. Unless we do the vaccine experiment, we will never know the answer.
The only EBV vaccine with efficacy data concerning IM is a monovalent (gp350) GSK EBV vaccine. This vaccine was shown to prevent IM in young adults (78% efficacy) but was found to be non-sterilising, as it did not prevent wild-type EBV infection. Subsequently, GSK licensed this vaccine to MedImmune, which sadly did not advance its development. Based on this experience and other early human studies, it is widely assumed that a component EBV vaccine is unlikely to create long-lasting sterilising immunity.
As with most vaccines, immunity fades with time, so vaccinated subjects may be at risk of delayed late wild-type infection. An argument against this is the experience with the prophylactic VZV childhood vaccine, which protects against delayed chickenpox or primary VZV infection. This protection is maintained and is not short-lived. A caveat is that the prophylactic VZV vaccine is a live-attenuated vaccine that is more likely to provide life-long sterilising immunity than a component vaccine. It is important to note that the live-attenuated VZV strain (Oka) can establish latent infection and reactivate to cause shingles in some individuals. However, this risk is substantially lower than with wild chickenpox infection. Similar experiences have been with other live-attenuated viral vaccines, i.e., smallpox, MMR and yellow fever.
One could argue for using a live-attenuated EBV vaccine. However, I am unaware of any efforts to develop one. I suspect this is due to the complexity of EBV and the difficulty of proving that an attenuated virus will not be oncogenic and induce delayed autoimmunity. Current EBV vaccines under development include subunit component and mRNA vaccines. To my knowledge, a viral vector vaccine using the modified vaccinia virus Ankara (MVA) has not been developed.
People don’t live in bubbles, so if you have some immunity to EBV from a vaccine, you will likely get exposed to wild-type EBV from day-to-day interactions with other people. Based on trial data, these exposures will likely cause asymptomatic EBV infection, which will give you lifelong protection against EBV infection unless you become immunocompromised. Therefore. I don’t think a non-sterilizing component EBV vaccine will create a large population of older adults susceptible to IM. I suspect most older people will become infected asymptomatically. We can test this in registry studies as we follow up cohorts of people vaccinated with an EBV vaccine to prevent IM.
Evolutionary biology
Some commentators feel that as more people are vaccinated against EBV, the vaccine will eventually eliminate EBV from the human population, which may have consequences for human biology. The theory is that EBV plays an essential positive role in human immunity. Again, this is theoretical and not evidence-based. When you study EBV-seronegative older adults, they don’t seem to have any problems with their immune function and general biology. Granted, older EBV-negative adults may benefit from the herd, i.e. they are protected by the surrounding EBV-seropositive subjects. We can potentially look at this by studying EBV seronegative older adults to see if they have some problems because they don’t have EBV. These people are hard to find, and recent data suggest that some seronegative subjects have T-cell responses to EBV and, hence, may not be genuinely EBV-negative.
Conversely, we could look for benefits that EBV may offer humans. We haven’t found any noticeable benefits of having EBV, only the abovementioned negatives. Is EBV a symbiont (positive benefits for itself and the host), or is it a parasite? I suspect EBV is a symbiont, and its benefits likely related to B-cell immunity will emerge with future research. I am incubating some ideas around this research theme. This, however, is not a reason not to do the necessary experiment and test an EBV vaccine to prevent IM and downstream events.
So, my message to the EBV vaccine naysayers or killjoys is that unless you can produce data, you should support the EBV vaccine experiments and consider what experiments you want to conduct to prove your point.
I know this newsletter is hardgoing. Please ask questions if you have any doubts.
The survey to explore your attitude toward an EBV vaccine is still open. If you have two minutes, please complete it.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.

















Share this post