Can natalizumab be used to prove that EBV is the driver of MS disease activity?
Natalizumab works by blocking the trafficking of immune cells into the central nervous system (CNS). The current dogma states that these immune cells are what actually causes MS and by preventing them from getting into the CNS you stop MS.
The other hypothesis, which is the one that I favour, is that MS is caused by EBV and it is the replication of EBV in the CNS that causes MS. EBV lies dormant in B-cells and it is the infected B-cells that then carry EBV into the CNS; i.e the ‘Trojan Horse’ hypothesis. Natalizumab works by preventing EBV-infected B-cells from getting into the CNS and hence keeps MS at bay.
When you stop natalizumab and allow these EBV-infected B-cells to traffic back into the CNS you get rebound MS disease activity. Rebound disease activity, in the form of relapses and/or MRI activity, occurs in over 50% of pwMS when they stop natalizumab. Although rebound is usually mild, it can rarely cause severe disease. Tragically two patients died from a catastrophic relapses and their brains were studied post-mortem were was packed full of EBV virus and was associated with a prominent immune response against the virus (papers 1a & 1b below).
I am aware that two swallows do not make a summer, but there is other evidence that active EBV infection drives focal MS disease activity. Another paper from Francesca Aloisi’s laboratory shows that a large number of CD8+ or cytotoxic T-cells in the brains of pwMS are EBV-specific targeting EBV proteins from both the latent and lytic phase of the EBV life-cycle (paper 2 below). This study suggests that natalizumab works by blocking EBV-infected B-cells delivering the virus to the CNS and the lymphocytes that respond to the virus and cause the damage. By blocking this cascade natalizumab stops new lesions from forming.
Another piece of the jigsaw puzzle comes from the observation that natalizumab-associated rebound is prevented by depleting B-cells with an anti-CD20 therapy such as rituximab or ocrelizumab. Anti-CD20 therapies are known to reduce EBV viral loads and are actually used to treat EBV-associated lymphomas and lymphoproliferative diseases. So why don’t we replace an anti-CD20 therapy with an antiviral drug targeting EBV instead? This strategy will at least leave the immune system and B-cells intact.
In fact, this experiment may have been tried already with teriflunomide. Yes, teriflunomide and related drugs from the class of dihydroorotate dehydrogenase inhibitors (DHODHi) work against EBV. We have shown in a small study that they reduce EBV viral shedding in the saliva of pwMS. Teriflunomide has also been shown to reduce natalizumab rebound, but not completely (paper 3 below). The observation that it was not 100% effective could be explained by the fact that teriflunomide penetrates the CNS poorly. I suspect an EBV antiviral drug may need to work in both the peripheral and CNS.
Experimental clinical trials
Because of these observations, we want to set up a trial platform to use natalizumab rebound to test EBV antivirals as potential treatments for MS. This is where we need your help. If you are on natalizumab would you be willing to participate in a clinical trial to see if an EBV antiviral can prevent rebound disease activity?
The following are two trial designs to test new EBV antivirals.
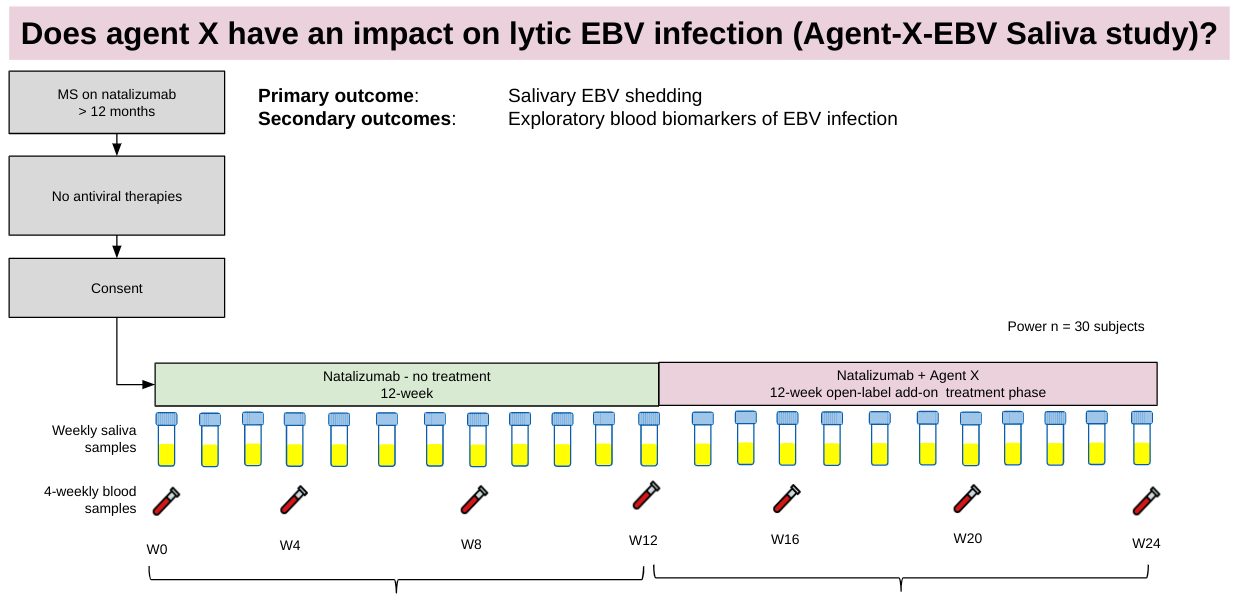
EBV Saliva Study
The first trial is simply to test whether or not new antivirals work against lytic EBV infection, i.e. can drug or agent X reduce or prevent EBV shedding in your saliva. In this first study, you stay on natalizumab and it requires you to simply collect weekly saliva samples for 24 weeks and have blood samples taken whenever you come up for your natalizumab infusions (4 or 6 weekly).
The first 12 weeks is the control period. We know that during a 12-week period about 40-45% of pwMS will shed EBV in their saliva. In the second 12 weeks, you will be given agent X which is a putative EBV antiviral. If it works against EBV then it should stop or reduce EBV shedding in saliva. By comparing the results from the active treatment phase with the control phase we can get a pretty good idea of how effective the antiviral is against EBV.
You may be aware that we are testing famciclovir using this trial design in our centre. This is called our FamV study and I would like to thank all our patients for participating. It is much appreciated.
EBV Natalizumab Rebound Study
If we show famciclovir or agent X is effective against EBV infection we then want to test it to see if it can prevent natalizumab rebound.
This study randomises pwMS who have been on natalizumab for at least 12 months to placebo or active drug (famciclovir or agent X) and will use MRI in months 2, 3, and 4 to look for any rebound disease activity on MRI (Gd-enhancing lesions or new T2 lesions). If we see any rebound disease activity you will be restarted on natalizumab as rescue therapy. This study is a true experimental medicine study and is directly testing whether or not focal MRI activity is associated with EBV infection. If this study is positive it will prove that EBV causes focal MS disease activity and will result in larger phase 3 EBV antiviral studies being performed. The question I have would you be willing to participate in one or both of these studies?
I have therefore prepared a short survey to get your feedback on the trial design that will be included in a grant application later this year if this study proves to be feasible. If you are a healthcare professional can you also please complete the survey I am interested in your responses as well.
Papers 1a & 1b
Rebound of disease activity in multiple sclerosis patients after natalizumab withdrawal is a potentially life-threatening event. To verify whether highly destructive inflammation after natalizumab withdrawal is associated with Epstein-Barr virus (EBV) reactivation in central nervous system infiltrating B-lineage cells and cytotoxic immunity, we analyzed post-mortem brain tissue from a patient who died during a fulminating MS relapse following natalizumab withdrawal. Numerous EBV infected B cells/plasma cells and CD8+ T cells infiltrated all white matter lesions; the highest frequency of EBV lytically infected cells and granzyme B+ CD8+ T cells was observed in actively demyelinating lesions. These results may encourage switching to B-cell depleting therapy after natalizumab discontinuation.
Studying rebound mechanisms in MS patients after interruption of natalizumab may advance our understanding of MS pathogenesis. To verify the role of Epstein-Barr virus (EBV) infection and anti-EBV immunity in post-natalizumab rebound, we analyzed postmortem brain tissue of a case of fatal MS relapse. Using immunohistochemistry, EBV latent, early and late lytic proteins and CD8+ T cells sticking to EBV lytically-infected cells were detected in multiple inflammatory white matter lesions. Using the pentamer technology on brain sections, EBV-specific CD8+ T cells were observed perivascularly. Cell-free EBV DNA was detected in cerebrospinal fluid. These findings confirm and extend the results obtained in another case of post-natalizumab fatal MS relapse, suggesting that this condition represents an EBV-associated immune reconstitution inflammatory syndrome.
Paper 2
ABSTRACT: Epstein-Barr virus (EBV) is a ubiquitous herpesvirus strongly associated with multiple sclerosis (MS), a chronic inflammatory disease of the central nervous system (CNS). Yet, the mechanisms linking EBV infection to MS pathology are uncertain. Neuropathological and immunological studies suggest that a persistent EBV infection in the CNS could stimulate a CD8 T-cell response aimed at clearing the virus but inadvertently causing CNS injury. Inasmuch as in situ demonstration of EBV-specific CD8 T cells and their effector function is missing, we searched for EBV-specific CD8 T cells in MS brain tissue using the pentamer technique.
Postmortem brain samples from 12 donors with progressive MS and known HLA class I genotype were analyzed. Brain sections were stained with HLA-matched pentamers coupled with immunogenic peptides from EBV-encoded proteins, control virus (cytomegalovirus, influenza A virus) proteins and myelin basic protein. CD8 T cells recognizing proteins expressed in the latent and lytic phases of the EBV life cycle were visualized in white matter lesions and/or meninges of 11/12 MS donors. The fraction (median value) of CD8 T cells recognizing individual EBV epitopes ranged from 0.5 to 2.5% of CNS-infiltrating CD8 T cells. Cytomegalovirus-specific CD8 T cells were detected at a lower frequency (≤0.3%) in brain sections from 4/12 MS donors. CNS-infiltrating EBV-specific CD8 T cells were CD107a-positive, suggesting a cytotoxic phenotype, and stuck to EBV infected cells.
Together with local EBV dysregulation, selective enrichment of EBV-specific CD8 T cells in the MS brain supports the notion that skewed immune responses toward EBV may contribute to inflammation causing CNS injury.
IMPORTANCE: EBV establishes a lifelong and asymptomatic infection in most individuals and more rarely causes infectious mononucleosis and malignancies, like lymphomas. The virus is also strongly associated with MS, a chronic neuroinflammatory disease with unknown etiology. Infectious mononucleosis increases the risk of developing MS and immune reactivity toward EBV is higher in persons with MS indicating inadequate control of the virus. Previous studies have suggested that persistent EBV infection in the CNS might stimulate an immunopathological response causing bystander neural cell damage. To verify this, we need to identify the immune “culprits” responsible for the detrimental antiviral response in the CNS. In this study, we analyzed postmortem brains donated by persons with MS and show that CD8 cytotoxic T cells recognizing EBV enter the brain and interact locally with the virus infected cells. This antiviral CD8 T cell-mediated immune response likely contributes to MS pathology.
Paper 3
Background: Natalizumab (NTZ) is a highly effective disease modifying treatment for relapsing multiple sclerosis (RMS), but it increases risk of progressive multifocal leukoencephalopathy (PML) in patients with serum anti- John Cunningham virus (JCV) antibodies.
Objective: To assess the safety and efficacy of rapid transition, from NTZ to teriflunomide (TFM) in RMS patients.
Methods: Clinically stable NTZ-treated, anti-JCV antibody positive RMS patients were switched to TFM 28 ± 7 days after their last dose of NTZ. The primary endpoint was proportion of relapse free patients at 24 months.
Results: Median [IQR] age of the 55 enrolled patients was 47 [40.7, 56.3] years, 76% were female. The median [IQR] number of prior NTZ treatments was 34 [18, 64]. annualized relapse rate (ARR) was 0.07 and 77% of the patients were relapse free at 24 months. Mean time to first GAD + lesion was 19.6 months, and to new/enlarging T2 lesion was 19.2 months. Mean time to 3 month sustained disability worsening (SDW) was 22 months and proportion free of 3-month SDW was 0.87. There were no cases of PML.
Conclusions: The washout-free transition of NTZ to TFM was an efficacious and safe strategy for patients at risk of developing PML.ClinicalTrials.gov Identifier: NCT01970410.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite that is currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers, I would appreciate it if those who can afford a subscription please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry or Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.














Share this post