I am still receiving several queries a week about COVID-19, its vaccines and the management of MS during the tail of the pandemic. The following is a quick summary of important things to know about COVID-19 and MS.
New BA.2 Variant
The new BA.2 variant, which was first identified in Denmark, has started to surge. BA.2 is likely to become dominant and take over from the Omicron BA.1 variant in the next few weeks.
The BA.2 variant is likely to be more infectious, with more household contacts becoming infected than the Omicron BA.1 variant (13.4% vs. 10.3%) (BMJ 5-Feb-2022).
At least 25 weeks after the two doses of COVID-19 vaccine the effectiveness against symptomatic infection is reported as 9% and 13% for the BA.1 and BA.2 variants respectively, which increases to 63% for BA.1 and 70% for BA.2 at 2 weeks after a third dose of the vaccine (BMJ 5-Feb-2022).
Different symptoms
With the Omicron BA.1 and BA.2 variants, the symptoms of COVID-19 have changed. The Zoe app study in the UK shows that runny nose, headache, fatigue, sneezing and sore throat are what define the Omicron COVID-19 syndrome. The high temperature and loss of taste and smell, seen with earlier SARS-CoV-2 variants, are now uncommon.
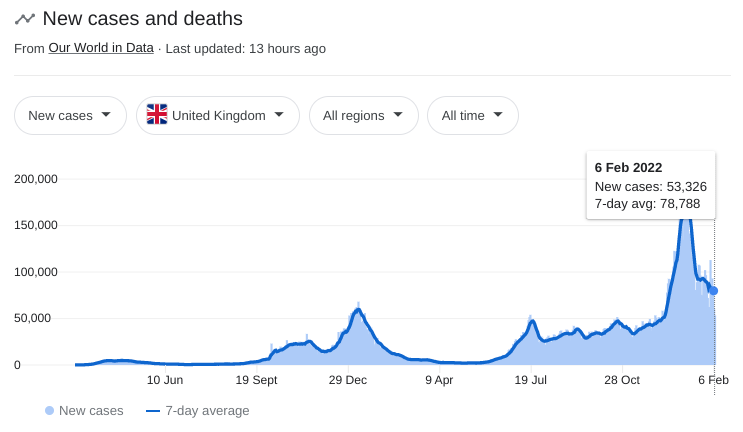
Case numbers
Although absolute UK case numbers remain high we should be relieved with what is happening on the ground. There are far fewer hospital admissions, in particular, intensive care admissions for ventilatory support. Even when patients are being admitted to a hospital they are spending on average only 3-4 days in hospital compared to over 7 days with the earlier SARS-CoV-2 variants.
The one stand-out message is that the majority of people with COVID-19 in ITU are people who are unvaccinated and if vaccinated they tend to be unboosted, i.e. they have had not had a third dose of the vaccine. The takehome message remains the same #GetVaccinatedASAP or #GetBoosted.
COVID-19 death rates, however, are staying stubbornly high and this may relate to the fact that many people being admitted to hospital with other diagnoses are found to be incidentally infected with SARS-CoV-2 and hence if they die their deaths are being classified as being due to COVID-19. It is suspected that some of these incidental infections are nosocomial, i.e. they are occurring in hospitals. So the deaths being ascribed to COVID-19 in the current wave need to be contextualised.
Vulnerable
People with MS should be on the NHS’s vulnerable list and hence subject to rapid PCR diagnosis, which grants them rapid access to antiviral therapies that are being prescribed in the community. Please note this PCR system is different to the standard non-urgent PCR test system. If you have MS and are not on the vulnerable list you need to contact your GP.
New antivirals
From the 10th of February, the more effective nirmatrelvir (Paxlovid) from Pfizer will be available for use in the community in vulnerable people who have developed COVID-19. The UK government has procured 2.75 million courses of the drug. When nirmatrelvir is given within of symptom onset it reduces COVID-19 related hospital admission and/or death by 89% compared to placebo. Nirmatrelvir (Paxlovid) is therefore a welcome alternative to molnupiravir (Lagevrio), which is less effective. Of the monoclonal antibodies, sotrovimab (Xevudy) is the only one still being used on the NHS as the other monoclonals are not effective against the Omicron variants.
Vaccines
Booster doses are being offered to all adults in the UK from three months since their last dose. For those of you who are immunosuppressed, in particular, those of you who are on anti-CD20 therapy (ocrelizumab, ofatumumab or rituximab) or an S1P modulator (fingolimod, siponimod, ozanimod or ponesimod) your third dose of the vaccine should be classified as being part your primary vaccine and therefore you are eligible for a fourth dose, i.e. the first official booster dose, three months after your third dose of the vaccine.
It is clear from recent data that pwMS on fingolimod and ocrelizumab make blunted vaccine responses that are associated with a higher incidence of COVID-19 (see articles below) and for ocrelizumab more severe COVID-19 (see Schiavetti et al., 2022, below). For this reason, I am still recommending patients on anti-CD20 therapies get their booster vaccine as soon as possible rather than trying to time the vaccine to optimise the anti-spike protein antibody response. Optimising antibody vaccine responses is a moving target particularly in relation to Omicron and its variants, which are only really neutralized by very high titres of antibody. The aim of the vaccine booster is to boost T-cell immunity rather than B-cell immunity with the aim of protecting you against severe disease.
Please note that on-balance severe COVID-19 is less likely now because of pre-existing immunity, less virulent strains of the virus, effective antivirals and in the case of those with infections requiring hospitalisations better treatment of COVID-19.
Self-isolation
Several of my patients are still self-isolating almost 2 years into the pandemic. If you are vaccinated and boosted there is no reason to self-isolate. The Omicron variants, even the new BA.2 variant, are less virulent and less likely to cause severe pneumonia and we now have effective antiviral drugs to treat the virus. At some point, we have to accept living with this virus and hence a cautious reintegration into society makes sense and in my opinion, is essential for your mental health (#ThinkSocial).
Research articles of interest
Article 1
Figure: Monthly incidence rate of SARS-CoV-2 infection among multiple sclerosis (MS) patients receiving disease-modifying therapies (DMTs) versus the general population of 20-years-old or above in England. Data for individual DMTs are presented in separate graphs. The coloured line in each graph is the incidence rate of infection during each month per 100 MS patients taking each DMT, and the shaded areas are the 95% confidence intervals. The black line is the incidence rate of infection during each month per 100 people aged 20 years or above in the general population. The dashed grey line is the cumulative SARS-CoV-2 vaccination (both doses) uptake during each month among the adult population in England.
Background: Contradicting assumptions have been made about the effectiveness of SARS-CoV-2 vaccines in patients with multiple sclerosis (MS) receiving immunomodulatory disease-modifying therapies (DMTs) based on the quantification of humoral and cellular immune responses. This study aimed to understand changes in the risk of SARS-CoV-2 infection among the total population of patients receiving MS DMTs in England following mass vaccination.
Methods: This is a retrospective analysis of national data collected prospectively and longitudinally. National Health Service (NHS) England and NHS Improvement (NHSE/I) hold prescribing data on all commissioned MS DMTs in England. United Kingdom Health Security Agency (UKHSA) has been collecting data on all registered SARS-CoV-2 test results, including polymerase chain reaction and rapid antigen tests. All patients receiving MS DMTs were identified using NHSE/I datasets. All patients receiving MS DMTs with SARS-CoV-2 infection (i.e., positive test) from March 2020 to August 2021 were identified by merging NHSE/I and UKHSA datasets. Similar data for the general population were captured using publicly available datasets of the United Kingdom government. The incidence rate ratios (IRR) of SARS-CoV-2 infection among patients receiving MS DMTs compared to the general population during the pre-vaccination (November 2020 to January 2021) and post-vaccination (June to August 2021) periods were calculated.
Results: A mean (standard deviation) of 41,208 (4,301) patients received an MS DMT in England during each month from March 2020 to August 2021. The IRR (95% confidence interval) of infection in patients taking ocrelizumab versus the general population increased from 1.13 (0.97–1.31) during the pre-vaccination period to 1.79 (1.57–2.03) during the post-vaccination period. For patients on fingolimod, it increased from 0.87 (0.73–1.02) to 1.40 (1.20–1.63) during the same periods. There were no significant changes for patients on other MS DMTs.
Conclusion: SARS-CoV-2 vaccines offer less protection against infection to patients taking ocrelizumab or fingolimod, who have an impaired immune response to vaccines, than the general population. These findings will have implications for vaccination policies.
Article 2
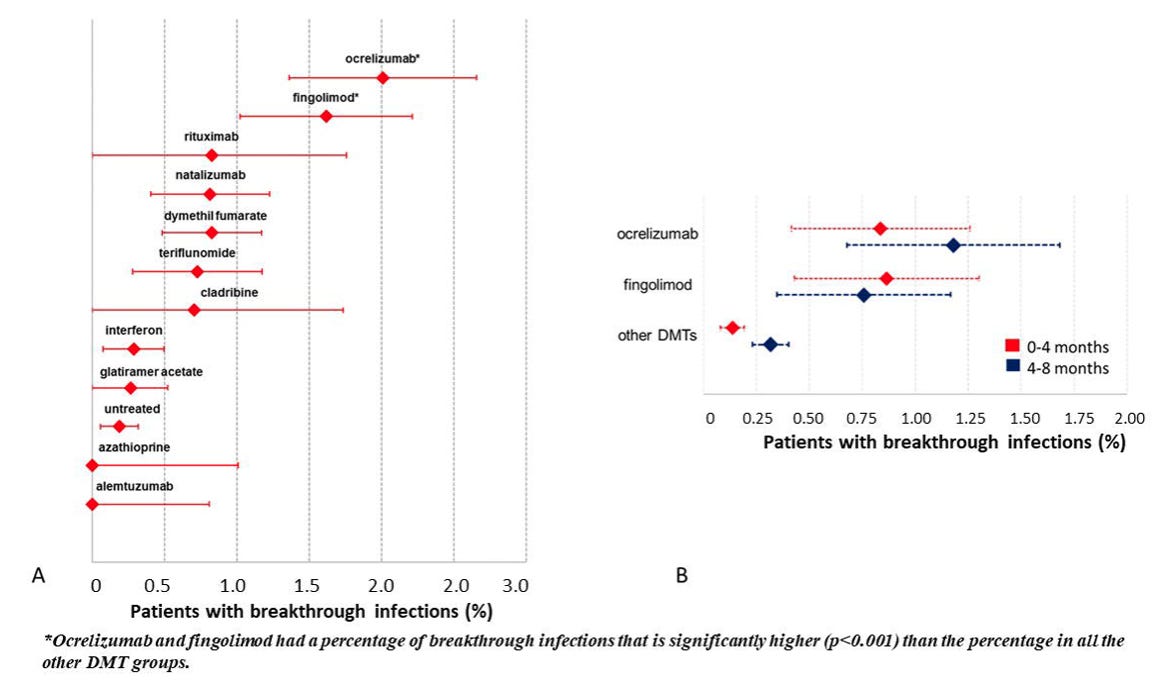
Background: Patients with Multiple Sclerosis (pwMS) treated with anti-CD20 or fingolimod showed a reduced humoral response to SARS-CoV-2 vaccines. In this study, we aimed to monitor the risk of breakthrough SARS-CoV-2 infection in pwMS on different Disease-Modifying Therapy (DMT).
Methods: Data on the number of vaccinated patients and of patients with a breakthrough infection were retrospectively collected in 27 Italian MS centres. We estimated the rate of breakthrough infections and of infection requiring hospitalization per DMT.
Findings: 19641 vaccinated pwMS were included in the database. After a median follow-up of 8 months, we observed 137 breakthrough infections. As compared to the other DMTs, the rate of breakthrough infections was significantly higher on ocrelizumab (0.57% vs 2.00%, RR=3.55,95%CI=2.74-4.58, p<0.001) and fingolimod (0.58% vs 1.62%, RR=2.65,95%CI=1.75-4.00, p<0.001), while there were no significant differences in any other DMT group. In the ocrelizumab group the hospitalization rate was 16.7% vs 19.4% in the pre-vaccination era (RR=0.86,p=0.74) and it was 3.9% in all the other DMT groups vs 11.9% in the pre-vaccination period (RR=0.33,p=0.02).
Interpretation: The risk of breakthrough SARS-CoV-2 infections is higher in patients treated with ocrelizumab and fingolimod, and the rate of severe infections was significantly reduced in all the DMTs excluding ocrelizumab.
Subscriptions
I am using the paid subscriptions to administer the MS-Selfie Newsletter and associated MS-Selfie microsite that is currently in development. If you are an active paying subscriber thank you, your contribution is much appreciated.
The funds are being used to pay a professional medical writer to curate, rewrite and transfer the contents of the Newsletter onto a companion MS-Selfie microsite, which is being designed and maintained by a freelance web designer.
If you find these Newsletters helpful and want the wider MS community to continue to have access to all content I would encourage you to become a paid subscriber. Thank you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.
















Share this post