Are ultra-processed foods a problem in multiple sclerosis?
A poor diet, high in ultra-processed foods (UPFs), low in fibre, and insufficient water consumption underlies chronic constipation. What can be done about it?
Case study
I am 47 years old and have had MS for 28 years. I am pretty disabled and use a walking stick indoors and a wheelchair for outdoor mobility. My biggest problem is severe constipation. I may have a bowel movement once every two weeks. I have started having episodes of diarrhoea, which has caused me to be incontinent on several occasions. What can I do to help?
Prof G’s answer
This patient likely has faecal impaction and overflow diarrhoea. If properly managed, this patient should not be in this state. Do you agree?
Faecal impaction is a common cause of pwMS having unscheduled or emergency hospital admissions. When severe, it can cause intestinal obstruction and rarely bowel perforation. If you are constipated and have severe abdominal pain and bloating, you need to seek medical attention. Pressure from the impacted stool can cause tears in the rectum or rectal fissures. In more severe cases, it might lead to rectal prolapse, where part of the rectum protrudes through the anus. Hard stool can cause ulcers in the lining of the rectum and colon. These ulcers might bleed, leading to further complications like anaemia.
Faecal impaction can lead to infections that cause abscesses. If bacteria from the stool enter the bloodstream or other tissues, this can potentially lead to life-threatening conditions like sepsis. In extreme cases, the pressure from the impacted faeces can cause a perforation or tear in the bowel. This leads to peritonitis, an infection of the abdominal cavity, which can be life-threatening. A severely impacted colon can press against the bladder, leading to urinary incontinence, urinary tract infections, or other urinary problems, which is why you can’t manage bladder problems without sorting out constipation.
Repeated occurrences of faecal impaction can worsen chronic constipation, creating a vicious cycle that can be difficult to break without medical intervention. The reason why this happens is that the colon stretches and becomes less mobile. Severe and chronic faecal impaction can damage the nerves and muscles of the intestines, leading to long-term or permanent impairment of intestinal function. This can result in a megacolon, a condition where the colon enlarges. This exacerbates constipation and complicates future bowel movements. I have had three pwMS in my career as an MSologist who has had to have hemicolectomies and colostomies to manage this problem.
Chronic constipation and faecal impaction are associated with an increased risk of colorectal cancer, possibly due to prolonged contact of the intestinal lining with potentially harmful substances in the stool and an altered microbiome.
How do you treat faecal impaction?
This involves several steps to remove the impacted stool and prevent its recurrence. In some cases, especially when the impaction is severe, manual removal of the stool may be necessary. This is usually done by a healthcare professional using gloves and lubricated instruments to break up and remove the stool from the rectum. When I was a trainee, it was always the house officer's job to do the manual removal. It is a very unpleasant procedure and can be painful. However, most patients were very grateful after they were unimpacted.
Enemas can help soften the impacted stool and stimulate bowel movements. Different enemas can be used, i.e., saline, mineral oil, or phosphate. Both oral and rectal laxatives can help to soften the stool and promote bowel movements. I often use stool softeners, like docusate sodium and magnesium sulphate, and a potent stimulant laxative such as bisacodyl. Most patients whom I diagnose with faecal impaction and overflow diarrhoea can be managed as an outpatient at home. It is rare to have to admit someone with this problem.
Rectal suppositories containing glycerine or bisacodyl can be sufficient to stimulate bowel movements and soften the stool. They are inserted into the rectum and dissolve, providing localised action. Once the rectum and colon are emptied, this patient must take the necessary steps to prevent this from reoccurring.
How do you manage MS-related constipation?
Optimise your diet by eating lots of fibre (please see ‘Which is the best MS diet? (25-Aug-2021)’.
Don’t dehydrate yourself. Drink plenty of water; don’t think caffeine and alcoholic beverages are hydrating. Both caffeine and alcohol cause the kidney to make more urine (diuresis) and are, in fact, dehydrating.
Try and eliminate concomitant medication that exacerbates constipation (anticholinergics and opioids).
Exercise regularly; the anticipation of exercise and exercise stimulates a defaecation reflex.
If you need laxatives, start with a prokinetic agent, such as Senna, that stimulates the bowel to move. Then, add bulking (e.g., psyllium husks or other fibre substitutes), followed by liquifying agents (lactulose or polyethylene glycol).
Don’t suppress the need to go to the toilet; many people with chronic constipation learn bad habits; for example, they don’t like using toilets that are unfamiliar to them.
Some patients find probiotic supplements or fermented foods help, presumably by altering the microbiome.
Please read my MS-Selfie Newsletter Faecal Incontinence (4-Aug-2021) for more information.
How important is diet?
About ten years ago, one of our MSc students did a detailed dietary and bowel habit survey in a small cohort of patients with multiple sclerosis (MS) at our centre. The results were very sobering. Almost one-third of people with MS suffered from severe constipation, which was associated with reduced quality of life. Underlying this problem was a poor diet high in ultra-processed foods (UPFs), low in fibre, and insufficient water consumption. I am, therefore, not surprised by this US study on the general population, which shows that ultra-processed food consumption is associated with constipation (see research paper below). I have also added some basic information about UPFs.
Add to UPFs MS-related bowel hypomotility and concomitant medications that exacerbate constipation, e.g. anticholinergics; it is not surprising that constipation is one of the commonest symptomatic problems in pwMS.
Everyone who has MS needs to ask themselves if they are constipated. If so, what are you doing about it? Please be aware that constipation is associated with bacterial overgrowth syndrome, which can have systemic effects that could make MS-related symptoms worse. Bacterial metabolites are pro-inflammatory; some bacterial metabolites affect cognitive function and have adverse metabolic effects. The latter is a particular problem in people who have comorbid liver disease, which is unable to break down these toxic factors, or they bypass the liver due to a portosystemic shunt. One of the principles of gut health is preventing bacterial overgrowth associated with chronic constipation. For more information, please read ‘How is your gut health? (3-Jul-2023)’?
Finally, you can discuss gut health without addressing your diet. I have written extensively on diet and MS and now consider diet essential in the management of MS. The problem I have is what diet to recommend. For my thoughts on diet, please read ‘Which is the best MS diet? (25-Aug-2021)’.
One of the common themes underpinning all so-called healthy diets is the elimination or at least reduction in consumption of ultra-processed foods (UPFs). This is easier said than done, but the issue of UPFs is at least getting the attention of public health officials and politicians. For those of you who need to get up to speed on UPFs, I have included new data linking UPF consumption to constipation.
I would like to hear how you have taken action on your UPF consumption and what has worked to get you off UPFs.
What are ultra-processed foods (UPFs)?
UPFs are industrial formulations typically containing five or more ingredients. These ingredients often include substances not generally used in culinary preparations, such as preservatives, emulsifiers, sweeteners, and artificial colours and flavours. Key characteristics of ultra-processed foods are:
1. Ingredients: They contain ingredients rarely used in home cooking, such as high-fructose corn syrup, hydrogenated oils, emulsifiers, and protein isolates.
2. Additives: They often include additives that enhance flavour, appearance, or shelf life, such as artificial colours and flavours, preservatives, and sweeteners.
3. Nutritional Content: Ultra-processed foods tend to be energy-dense and low in essential nutrients. They are often high in sugars, unhealthy fats, and sodium yet low in protein, fibre, vitamins, and minerals.
4. Preparation: These foods are often ready-to-eat or require minimal preparation, making them convenient but potentially less healthy options.
5. Examples: Examples include soda, packaged snacks, sweets or candy, instant noodles, and pre-packaged meals.
Due to their high levels of unhealthy fats, sugars, and salt, ultra-processed foods are associated with various health concerns, including obesity, heart disease, diabetes and cancer. They are often contrasted with minimally processed or whole foods, which usually retain most of their original nutritional properties.
Why is it difficult to stop eating UPFs?
1. Addiction: UPFs are designed to be hyper-palatable, meaning they are engineered to taste exceptionally good. High levels of sugar, fat, and salt trigger pleasure centres in the brain, similar to other addictive substances. This leads to cravings and overeating.
2. Convenience and accessibility: UPFs are usually ready-to-eat or require minimal preparation, offering convenience. They are widely available in supermarkets, convenience stores, vending machines, etc., making them an easy choice for people with busy lifestyles.
3. Marketing and advertising: UPFs are heavily marketed, often using persuasive advertising techniques to target easy-to-influence populations such as children. Frequent exposure to UPF marketing material creates a psychological association between these foods and positive emotions or convenience.
4. Economic factors: UPFs tend to be much cheaper than healthier, whole-food alternatives, which is why their consumption is closely linked to poverty.
5. Cultural and social influences: in many societies, UPFs have become a significant part of the diet and social activities. From fast food chains to packaged snacks at social gatherings, these foods are deeply integrated into social experiences, making them harder to avoid.
6. Habituation and taste preferences: Regular consumption of UPFs leads to habituation, where the body becomes accustomed to high levels of sugar, fat, and salt. This alters taste preferences, making whole foods seem less appealing.
7. Emotional and stress eating: Some people turn to UPFs for emotional comfort or stress relief. The immediate pleasure and temporary relief from stress or negative emotions reinforce the habit of consuming these foods in response to emotional triggers. This is why dietary interventions don’t work very well unless they are combined with behavioural therapy.
8. Lack of nutritional education: A population-level lack of awareness or understanding of nutrition leads people to make poor dietary choices. Without education and adequate knowledge about the health risks associated with UPFs and the benefits of whole foods, people continue to consume them out of habit or convenience.
Research paper
Background & aims: Ultra-processed foods (UPFs) may have a negative impact on bowel habits. We aimed to assess the association between UPF and unprocessed or minimally processed food (MPF) intake and bowel habits among adults in the United States (U.S.).
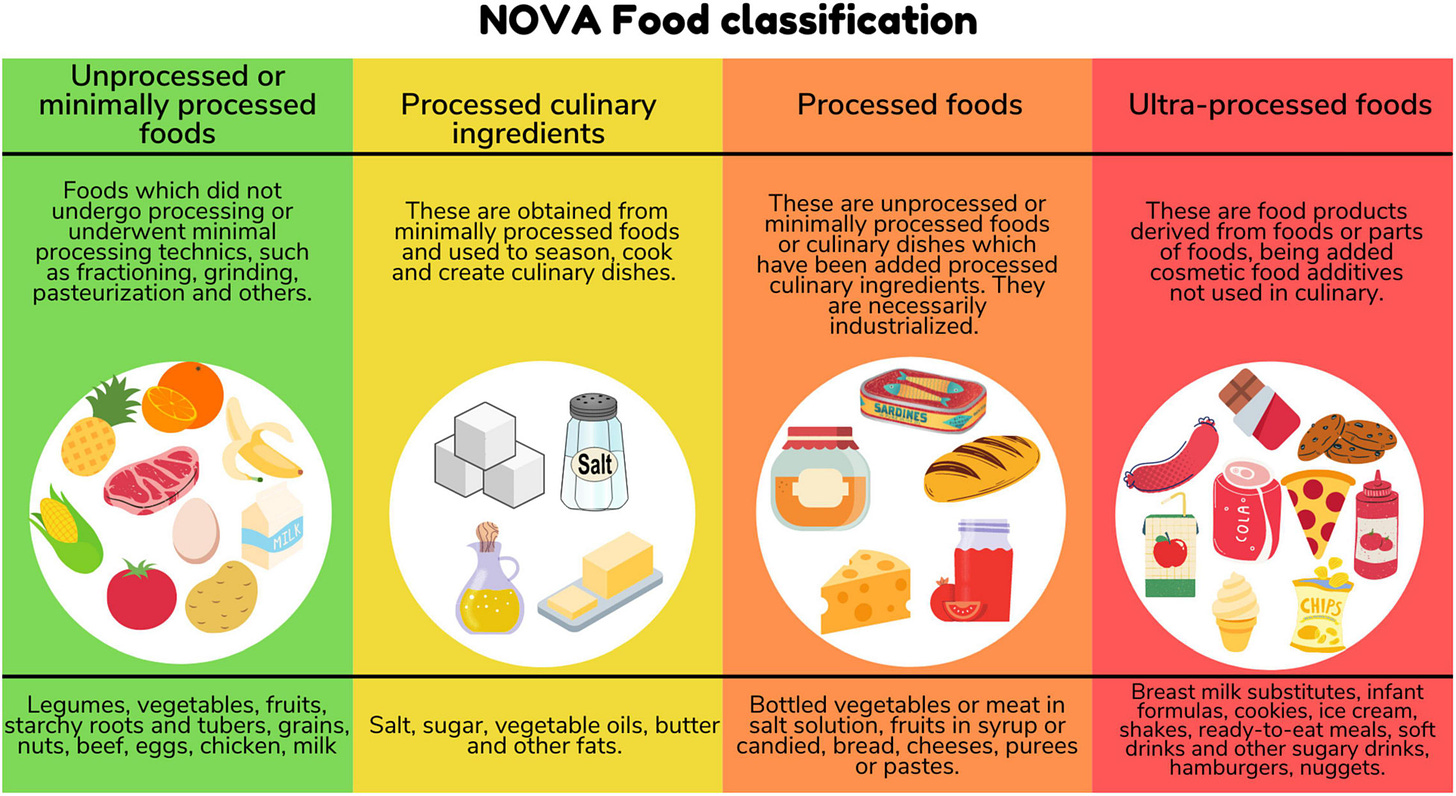
Methods: We performed a cross-sectional study using data from the National Health and Nutrition Examination Survey (2005-2010). We used two 24-hour dietary recalls and, based on the Nova classification, calculated intakes of UPFs and MPFs. Constipation and diarrhea were defined using the Bristol Stool Form Scale and stool frequency. We performed survey-weighted logistic regression and substitution analysis to estimate the odds ratios (ORs) and 95% confidence intervals (CIs).
Results: Among 12,716 U.S. adults, there were 1290 cases of constipation and 1067 cases of diarrhea. Median UPF and MPF intakes were 26.5% and 66.2% of total grams per day, respectively. Greater UPF consumption (in % gram/d) was associated with higher odds of constipation (adjusted OR [aORQ4 vs Q1], 2.20; 95% CI, 1.76-2.74) (Ptrend < .001) but not diarrhea (aORQ4 vs Q1, 0.82; 95% CI, 0.62-1.09) (Ptrend = .12). Increased MPF consumption was associated with lower odds of constipation (aORQ4 vs Q1, 0.46; 95% CI, 0.370-0.57) (Ptrend < .001). Associations with constipation were attenuated after adjusting for diet quality (aORQ4 vs Q1, UPF, 1.53; MPF, 0.69). Substituting 10% of UPF intake with an equivalent proportion of MPFs was associated with lower odds of constipation (aOR, 0.90; 95% CI, 0.87-0.93).
Conclusions: UPF intake was associated with higher odds of constipation, whereas the odds were lower with greater MPF consumption. The effect of food processing on bowel habits was independent of diet quality.
Keywords: Colon; Epidemiology; Nova; Nutrition.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
X (Twitter) / LinkedIn / Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.





I switched to remove as much of the "low fibre" from my diet - try to go whole grain and unprocessed wherever possible. It doesn't fix the problem of MS gut transit but it doesn't make it worse. There are "fast" alternatives particularly when cooking at home - wholemeal wraps (lightly grilled so they don't go soggy) instead of white bread sandwiches, whole grain rice, leave skins on potatoes cos they're the best bit anyway, that sort of thing. Try to make it convenient to eat healthy.
For the "other end" of things I found laxatives took ages to work and ended up working when I needed to be away from a convenient loo. I was given a Peristeen trans-anal irrigation device to use (which I have dubbed "The Poo-matic") which is an absolute godsend. Being able to just do that every couple of days, at my own convenience, when I have time set aside means I stay in control. I can do that for an hour (usually less), clean up, shower and then I'm good for 24 - 48 hours. Psychologically having some control over the more potentially embarrassing parts of MS is so important.
I know the theory, but in practice it's hard.
I try to eat organic and make homecooked meals most days (fibre, lots of fluids, correct posture for making stool, supplements, etc.: all check).
I would love to try a true holistic approach to treat my MS: with HIIT, a really clean diet, enough rest, less stress,...
But I still (need to) work for a living and fatigue is a big issue for me, as I'm sure it's for many PwMS.
Finding time and energy to acquire all that healthy food daily, cook it, exercise, do some HIIT, keep working, and btw not stressing too much about those and other things...
I'm sure not the only one.