Warts and HPV vaccination
I discuss dealing with warts on immunosuppressive therapies and the issue of HPV vaccination to prevent them and HPV-associated cancers.
Warts, both cutaneous and genital, are a relative contraindication to immunosuppressive therapies. I have had one patient who has a torrid time with cutaneous warts after receiving alemtuzumab treatment. Fortunately, her immune system rejected the warts when it reconstituted and she is now fine.
At least with alemtuzumab and other IRTs (immune reconstitution therapies) you can rely on the immune system reconstituting, then finding the virus (human papillomavirus or HPV causes warts), fighting it and hopefully rejecting it and clearing the body of HPV. This does not occur with continuous immunosuppressive therapies.

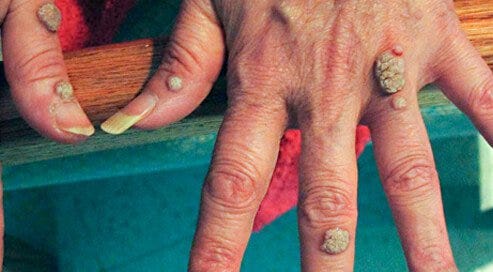
Although relatively uncommon, I have seen patients on fingolimod with cutaneous warts, which tend to spread and get worse with time. One person on fingolimod that I saw had warts on her hands, which were very disfiguring and causing a lot of discomfort. Whenever she bumped them they would bleed, some had become secondarily infected and they were obviously causing her distress. The bottom line is that her warts did not clear until she stopped fingolimod. Please remember that fingolimod was initially used as an immunosuppressant in the solid-organ transplant field and is therefore a chronic high-level immunosuppressant targeting both T and B cell responses of the immune system.
Warts on fingolimod, and by extension on the other S1P modulators (siponimod, ozanimod and ponesimod), are not a new problem and are well described in the medical literature. In general, warts only respond to treatment and clear when fingolimod is stopped. The problem we have is what to do about MS and MS rebound when you stop fingolimod or one of the other S1P modulators? In my opinion, the only solution is to go onto a DMT that is not a systemic immunosuppressive; these include interferon-beta, glatiramer acetate, teriflunomide and possibly natalizumab.
Interestingly, we now have a reasonably good vaccine that prevents the majority of human papillomavirus or HPV infections including the strains that cause warts. The Government now offers schoolchildren the HPV vaccine at age 12 or 13 to prevent cervical, penile, anal and some oral HPV-associated cancers. Unfortunately, the HPV vaccine offered by Public Health England is only the quadrivalent vaccine (Gardasil-4) and not the polyvalent vaccine (Gardasil-9), which covers more strains including most of the cutaneous and perineal wart strains.
The epidemiology of HPV infection is changing. People are becoming infected later in life and are spreading the virus. Social media and dating apps have revolutionised the adult dating world and many older people are becoming promiscuous in older age and are having unsafe sex. As a result of this, there has been a large increase in the incidence of sexually transmitted diseases in older people, including HPV infections. This has prompted some commentators to suggest that public health officials extend the HPV vaccine to all women and possibly all men. Why wouldn’t you want to reduce your risk of getting cervical or other HPV-associated cancers? Isn’t prevention better than having to treat HPV infection and its downstream effects, i.e. premalignant cervical lesions or cervical cancer?
As a result of these trends, an increasing number of pwMS are asking about the HPV vaccine. Similarly, when I go to meetings neurologists are asking me for advice or what to do about vaccines, in particular, the HPV vaccine There are several questions that HPV vaccination raises that are directly relevant to pwMS.
Question 1: If I have been vaccinated with the older quadrivalent vaccine could I receive the new vaccine to cover the other strains of the virus?
Yes, there is data that shows that the previous vaccination against HPV doesn’t stop your immune system from responding to the components that cover the additional strains.
Question 2: As I am on a DMT can I have the HPV vaccine?
This all depends on the DMT you are on. For the non-immunosuppressive immunomodulators such as interferon-beta and glatiramer acetate vaccination is not a problem. These agents do not blunt immune responses to vaccines. For the other DMTs, the story is not that clear. Fingolimod and ocrelizumab are known to blunt vaccine responses.
Vaccine responses to component vaccines on dimethyl fumarate (DMF) have been studied and were normal. However, I am not aware of any specific studies looking at the HPV vaccine and DMF; I would, however, think it would be fine to receive the HPV vaccine if you are on DMF.
Teriflunomide is similarly unlikely to blunt the immune response to HPV, but we don’t have specific data on the HPV vaccine and teriflunomide.
Natalizumab’s mode of action is unique and is unlikely to affect peripheral immune responses.
For the IRTs (alemtuzumab, cladribine, mitoxantrone and HSCT) vaccination should be delayed until after immune system reconstitution.
Question 3: I need to start a DMT, but I want to have the HPV vaccine or extend my cover with the new polyvalent vaccine. How long will I need to wait before I can start treatment?
The polyvalent vaccine at the moment requires 3 doses with the last dose given between 6 and 12 months. Ideally, to give your immune system a chance to respond to the vaccine you will need to wait until 4 weeks after the final booster.
Question 4: Should I delay starting DMTs to have the vaccine?
There is no simple answer to this question. You have to balance the risks and benefits of having the vaccine against the risks of under-treated or untreated MS. In relation to the IRTs, I would suggest going ahead and starting the IRT and delaying the vaccine until you have reconstituted your immune system. Delaying starting an IRT to have the vaccine does not make immunological sense in that the memory responses you have just made to the vaccine could potentially get depleted and depending on the intensity of the immunodepletion may not recover. For maintenance DMTs, in particular, fingolimod, DMF and ocrelizumab, you should probably delay starting treatment to have the vaccine; or at least the first two doses. Booster vaccine responses have been shown to occur on these treatments, which are better than so-called new or primary immune responses. Please note that these vaccine studies have tended to look at antibody response only and not T-cell responses. It is now clear even if you don’t mount a good antibody response to COVID-19 vaccines on ocrelizumab (anti-CD20) you still have detectable T-cell responses.
Question 5: If I want the new polyvalent vaccine will the NHS cover it?
At present, the answer is no. Public Health England covers the quadrivalent vaccine (Gardasil-4) under the national vaccine programme. If you want to be vaccinated against HPV you will have to cover the costs of the vaccine yourself. This is not too dissimilar to what happens with travel vaccines.
As you can see HPV vaccination is one of those factors that have to be put in the mix when deciding which is the correct DMT for you. It is not a major issue but is an important issue nevertheless. At the moment I don’t routinely advise my patients on this topic, but as it is something that has future health implications I am going to have to make it routine.
What is your view on this? Do you think healthcare professionals should be obliged to discuss issues around HPV vaccination before the start of a DMT?
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as generic advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.




When you do good i say ,when not i say also ... :)
Nice post