Type 1 diabetes prevention: lessons for MS
As a thought experiment would you trade in MS for having T1DM or would you stick with the autoimmune disease you know already?
I was invited to speak at a Type 1 Diabetes Mellitus (T1DM) meeting in Birmingham. The meeting focused on the early disease detection for potential secondary prevention. You can download the programme here. The T1DM field thinks the field of MS has something to teach them about disease modification and prevention. I believe the contrary, i.e. we have a lot in the field of MS to learn from them.
Many of the issues for T1DM prevention are similar to those for MS, but the main difference is that we have probably found the cause of MS and hence will potentially start primordial prevention studies earlier in MS than they will in T1DM. However, regarding secondary prevention, we are slightly ahead of T1DM. We can identify people with radiologically isolated syndrome (RIS), soon-to-be defined asymptomatic MS, albeit serendipitously at present, and then treat them to prevent them from developing clinically definite MS. However, many healthcare systems don't cover the costs of treating patients with RIS. Saying this, the vast majority of patients referred to me with RIS when interrogated clinically have clinical signs that they are not aware of, which allows them to label them as having MS.
T1DM has the advantage over MS in that it has better prediction tests, i.e., autoantibodies that can predict the development of T1DM in the near future. In addition, it now has a licensed treatment that delays the onset of T1DM in high-risk antibody-positive people—the drug teplizumab works by targeting T cells through antibodies against CD3 on T-cells. At present, this therapy is not covered by the NHS, but paediatric endocrinologists have started treating high-risk patients before NICE has approved the drug.
The downside for the field of T1DM is that diabetologists are very good at managing the disease. Patients on closed-loop systems that function as an artificial pancreas are likely to live almost ‘normal’ lives despite the costs and the not-so-insignificant hassle of living with an artificial pancreas. These excellent metabolic outcomes change the risk-benefit balance of potentially high-risk preventive therapies. However, I am not so sure about these arguments. Having an artificial pancreas with all the paraphernalia of glucose sensors and insulin pumps, and the costs of living a lifetime with T1DM, is not something I would want in comparison to a potential early high-risk immunotherapy to prevent the disease. People with T1DM also have mental health issues associated with having the disease, and many other hidden symptoms that are not highlighted. Although arguably not as bad as MS, T1DM is a stigmatising disease and reduces quality of life. I think using effective insulin replacement therapy as an argument against secondary prevention in T1DM is a poor and flawed position.
People with relapse-onset MS are lucky in that they have a sentinel event or events, i.e. an attack or relapses, that should allow a timely and relatively early diagnosis before too much irreversible end-organ damage has occurred. The same cannot be said for people with primary progressive MS (PPMS) who present when they have lost a lot of function. In comparison, the vast majority of people with T1DM present with end-organ damage, which is end-stage, and the only treatment option is insulin replacement therapy and rarely pancreatic islet transplantation. The challenge for the T1DM field is implementing population screening to diagnose T1DM before the loss of the end-organ.
Population screening raises many ethical issues about identifying people without treatment. We in the field of MS are in a catch-22. We have two licensed MS DMTs, dimethyl fumarate and teriflunomide, that have been shown to delay patients with RIS from developing clinically-definite MS. However, these trials were small and have not resulted in a label change for these DMTs. Hopefully, changing the definition of MS by reclassifying RIS as MS, albeit asymptomatic MS, will allow us to start treatment earlier. The funding of DMTs for asymptomatic MS will be a battle. Still, we may convince funders of the merits of treating asymptomatic MS as both DMF and teriflunomide are now generic and relatively cheap. At the same time, I would argue for further RIS trials to generate additional evidence for better and more pragmatic DMTs, particularly cladribine. Cladribine, in my opinion, would be the best therapy for asymptomatic MS as it is a short course, relatively safe, well tolerated and has better efficacy than teriflunomide and DMF. Do you agree? I think it will be hard to convince people with asymptomatic MS to remain on a tablet lifelong when they have not had any obvious symptoms of MS.
The T1DM field has taken the route of initially focusing on high-risk individuals, i.e family members of people with T1DM. It is now expanding to the general population with new antibody screening assays in development. I was impressed to see them developing point-of-care lateral flow tests for autoantibody screening. Sadly, we in the MS field are far from having screening tests that are reliable and validated. Even using genetic testing with polygenic risk scores (PRS) will not be sufficient to identify those who will develop MS with sufficiently high sensitivity and specificity. The area under the receiver operating curve for an MS PRS of less than 0.8 makes it unsuitable for MS prediction.
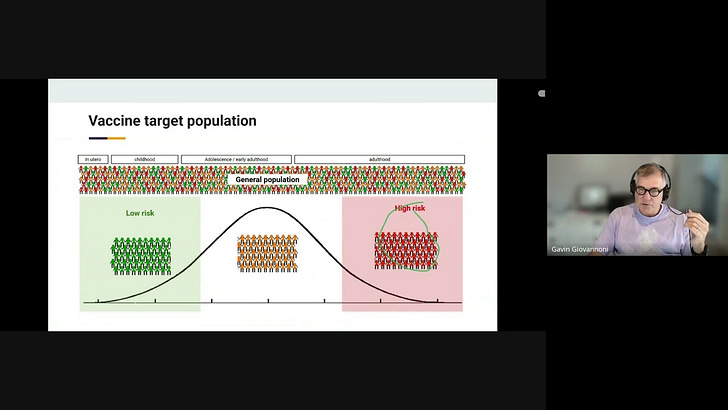
The downside of focusing on high-risk individuals is that, from a preventative perspective, it will prevent only a small proportion of people from developing MS. The reasons for this are that only a minority of people who develop MS can be classified as being high-risk before they develop MS. For example, only one in seven people with MS has a positive family history of MS. The majority of people who develop MS are, in fact, at low or moderate risk of developing MS and will not get through screening with our current tools. I favour targeting the general population for MS prevention to cast a wide net. I covered this in my recent talk at the Nobel MS symposium in Stockholm, which you can watch or review the slides.
My advice for the T1DM community from an MS is the following:
Adopt your new biological definition of T1DM to diagnose asymptomatic disease as early as possible, i.e. double auto-antibody positivity should be classified as T1DM.
Develop and validate markers of early pancreatic end-organ damage
This may require focusing on exocrine pancreatic function, which appears to precede the loss of endocrine function
Relying on endocrine stress testing with C-peptide curves after an oral glucose tolerance test may be too late in the evolution of T1DM. By the time you have a compromised area under the C-peptide curve, i.e., metabolic dysfunction, it is probably too late to modify the course of the disease substantially. We need to define and diagnose T1DM before this stage of the disease. The message here should be ‘time is pancreas’.
Develop and validate an easy-to-do stress test of exocrine pancreatic function, which may be affected earlier than endocrine function. This could be matched by structural evidence of pancreatic damage, i.e., volume loss.
Define a T1DM cure (e.g. loss of antibody positivity)
More work needs to be done on high-risk individuals with spontaneous cures, i.e. loss of autoantibodies. Do these people have evidence of regeneration of the pancreas? Is pancreatic end-organ damage reversible?
Defining a treatment-related cure will allow the field to treat a target in early disease prevention.
Focus on prevention
Primary prevention, for example, helps develop a multivalent enterovirus vaccine. Enterovirus infections are considered the most likely trigger of T1DM. Will a pan-enterovirus vaccine reduce the incidence of T1DM? I was impressed to notice that rotavirus vaccination reduces the incidence of T1DM by about 10%. I was told that SARS-CoV-2 infection increases the risk of getting T1DM by about 5-fold. In response, the UK is conducting a COVID-19 vaccine study on high-risk individuals to see if it can prevent the development of T1DM-associated autoantibodies.
Paediatric and adult T1DM incidence registers need to be established. These are essential for observational studies to see if an intervention reduces the incidence of T1DM. We need to have one for MS in England. Scotland is the only home country to have an MS incidence register.
Secondary prevention trials of disease-modifying therapies in presymptomatic T1DM with little end-organ damage, such as anti-CD40, anti-CD40L, anti-CD20, anti-CD3, cladribine, etc., will require the field to set up a platform study similar to those in place for oncology trials. This will allow multiple potential DMTs to be tested in parallel.
Develop adult T1DM secondary prevention models, e.g., stiff-person syndrome (SPS), an adult model of T1DM. At diagnosis, a third of people with stiff-person syndrome already have T1DM, and another third will develop T1DM in the next few years. Treating SPS with novel immunotherapies will allow one to study the effect of these treatments on T1DM evolution and provide a clue that they may work in children with early T1DM.
Work on finding the cause: “What is necessary for the development of T1DM?” This will allow the field to focus on one factor to prevent T1DM, similar to our focus on EBV as a prevention target to prevent MS.
You can view and download my slides from this meeting here. You are welcome to use them and hack them as you feel appropriate.
As a thought experiment would you trade in MS for having T1DM or would you stick with the autoimmune disease you know already?
I want to thank Parth Narendran for inviting me. It is good to see that we are not the only disease area with many miles to go before we sleep.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.




Definitely T1DM, although this is ‘autoimmune’ too. If I had that I would like an insulin syringe driver and continuous blood glucose monitor like the freestyle libre. In the next few years we’ll see these married into an automatic system which, once attached, removes the need to plan activities, insulin and meals in advance. Pancreatic implants are likely in the next decade. We’re just not so advanced in MS. MS treatment is in the dark ages compared to DM. To compare the pathologies the aetiologies are similar with the exception of end organ: Pancreas vs. Brain and spinal cord. I’d rather lose my pancreas. One day replacements will be available. That’s never going to happen for the CNS.
“As a thought experiment would you trade in MS for having T1DM or would you stick with the autoimmune disease you know already?”
Gladly swap MS for T1DM. Reasons: images of a post mortem MS brain; the impact of MS on mobility / walking (MS destroys the most simple of pleasures - game of tennis, stroll around an old city…..).