Prof G's response to the AI-generated newsletter
One of Gemini’s scotomas (blind spots) was the lack of mention of a systemic or local toxin driving MS pathology.
Thank you for all your thoughtful comments about my AI-generated newsletter on ‘How useful is AI-generated content in the field of MS?’ (13-Sept-2025). These are some of my initial thoughts.
General comments:
At present, large language models, such as Gemini Pro, are very good at doing rapid, detailed searches and producing a summary document with references in about 30-45 minutes. This would take a trained academic like me days, if not weeks, to complete. However, you need to be an expert to weed out the misinformation and inaccurate references in the search. Yes, it makes false claims. In addition, these LLMs have walls or limits to what they can produce, i.e. their training is generally based on information that is accessible on the web and not behind firewalls. Many academic publishers hide content behind firewalls and don’t allow bots to hoover up data behind these walls. In addition, the LLMs at present don’t necessarily go beyond their training material. This is why more specialised LLMs that have access to articles and information behind firewalls are better, for example, SciSpace and OpenEvidence or creating your own LLM by teaching it with resources you define or upload. I do this all the time using Google’s NotebookLM.
Another issue is how to prompt LLMs to give you the most appropriate answers. There is a new science of how to prompt LLMs. For more information on how to prompt LLMs, please read this article from Google.
I note that some, but not all, of you were impressed with the Newsletter that Gemini Pro 2.5 Deep Research produced in response to the prompt: “Is there an alternate theory of multiple sclerosis, other than the autoimmune theory, that posits that Gadolinium-enhancing lesions are actually not the disease but the immune response to what is causing multiple sclerosis?”. Please note I edited this newsletter to make sure I took out the hallucinations, and I culled all the references to make it easier to read. The raw, unedited version was not fit for purpose.
On a superficial level, the review it produced summarised the debate on the "Outside-In" versus the “Inside-Out” models reasonably well, but failed to discuss some pivotal insights from the field that need to be considered, nor did it discuss in any detail what is driving the pathology within the central nervous system (CNS). It only briefly mentioned viruses and spent most of the time discussing oligodendrocyte death and mitochondrial pathology. Surely any thinking person would think of oligodendrocyte death and mitochondrial pathology as being downstream of the cause of MS?
One of Gemini’s scotomas (blind spots) was the lack of mention of a systemic or local toxin driving MS pathology. The two leading contenders are Clostridium perfringens exotoxin and Frederik Gay’s bacterial toxin sphingomyelinase.
Toxins:
Clostridium perfringens is a common inhabitant of the human gut, but certain strains produce potent toxins. The epsilon toxin is a neurotoxin known to cause significant damage to the CNS in animals. Studies have reported a higher prevalence of epsilon toxin-producing strains of Clostridium perfringens in the gut microbiome of individuals with MS compared to healthy controls. Some research has found a higher frequency and/or elevated levels of antibodies against the toxin in MS patients, suggesting a past or ongoing exposure to the toxin. The epsilon toxin is a potent neurotoxin with the ability to cross the blood-brain barrier, which prevents harmful substances from entering the CNS. Once in the CNS, epsilon toxin has been shown in animal studies to target and kill oligodendrocytes selectively.
Sphingomyelinase is an enzyme that breaks down sphingomyelin, a key component of the myelin sheath that insulates nerve fibres. The breakdown product of this reaction is ceramide. High levels of ceramide are known to trigger apoptosis, or programmed cell death. The accumulation of ceramide could lead to the death of oligodendrocytes in the CNS, which are responsible for producing and maintaining myelin. Studies have found increased levels of both sphingomyelinase activity and ceramide within active MS lesions and elevated levels of ceramide in the CSF of pwMS compared to healthy controls. Several bacteria produce sphingomyelinase (e.g., Staphylococcus aureus, Pseudomonas aeruginosa, Bacillus cereus, …). Frederik Gay’s research points to the involvement of a specific bacterial sphingomyelinase as the initiator of the primary lesion of MS, in advance of demyelination, with the bacterial toxin gaining access to the CNS via the mucosa of the paranasal sinuses.
This is why it makes sense to develop therapies to neutralise these toxins to test as DMTs in pwMS. I will do a separate newsletter on the toxin hypothesis of MS later.
Field Hypothesis:
Another Gemini scotoma was stereotypical attacks suggestive of relapse. Did you know that if you have an MS relapse or attack in one particular area of the brain or spinal cord, you are more likely to have subsequent attacks in this area (see paper 1 below). I have in the past referred to this as the so-called field hypothesis, i.e. something locally triggers recurrent attacks in the same site.
What underlies the field effect? One explanation is that the area that is damaged by the initial attack is more likely to trigger autoimmune responses in future as a result of the local up-regulation of so-called second, or danger, costimulatory immune signals. This occurs in response to the factor produced as part of the initial inflammatory event. For T-cells to become activated, they need an antigen-specific signal via the T-cell receptor and an additional signal via co-stimulation.
Another hypothesis, which I favour, is that there is something in the field that triggers relapses. Possibly a virus? Why do I say this? Firstly, when pwMS were treated with interferon-gamma, a cytokine or inflammatory mediator that stimulates immune responses, they all had relapses (paper 2). The interesting thing about these interferon-gamma induced relapses is that they occurred in sites previously affected by MS. When I discussed this observation with the late Hillel Panitch, who was the principal investigator on the gamma-interferon trial, he thought that this observation was fundamental and was telling us something important about the cause of MS. It was this insight and my discussion with Hillel that led me to formulate my leprosy hypothesis about MS (paper 6).
Another observation that supports the abnormal field hypothesis is the rebound effect after natalizumab. This suggests that whilst you keep T and B cells out of the nervous system with natalizumab, the field (brain and spinal cord) becomes more abnormal. When you let the immune cells back in, they detect the abnormal field and run amok trying to clear up what is causing MS in the field. This is what happens with IRIS (immune reconstitution inflammatory syndrome) and PML (progressive multifocal leukoencephalopathy). When natalizumab is washed out, the immune system finds the JC virus and tries to clear the virus by initiating an inflammatory process. Some of us think that rebound post-natalizumab is simply IRIS in response to the virus or viruses that cause MS.
Another observation comes from serial MRI studies that have shown subtle changes in the white matter many weeks or months before a gadolinium-enhancing lesion appears. This suggests that the primary pathology is something in the nervous system that takes weeks or months to trigger a focal inflammatory lesion. The challenge for us all is to find out what this field abnormality is. I think the best chance we have of doing this is to study the brains of people with MS on natalizumab. To do this, we will need someone with MS to die whilst on natalizumab treatment and to donate their brain to a unit with the necessary techniques to look for viruses. In fact, this has happened twice already, and the results are compelling, but seldom discussed by MS researchers.
Brain tissue from two patients who tragically died during a fulminating MS relapse following natalizumab withdrawal showed numerous EBV-infected B cells and plasma cells with infiltrating cytotoxic CD8+ T lymphocytes (CTLs) infiltrating all of the lesions in the white matter (papers 3 & 4). The highest number of EBV lytically infected cells and granzyme B+ CTLs were observed in actively demyelinating lesions. This case suggests the rebound post-natalizumab may be in response to EBV-infected B-cells and plasma cells in the brains of people with MS.
I am aware that two swallows do not make a summer, but could these cases be the smoking gun we are looking for?
Subsequent studies show that a large number of CD8 T-cells in the brains of pwMS are EBV-specific, targeting EBV proteins from both the latent and lytic phase of the EBV life-cycle (paper 5). This study included post-mortem samples from 12 people with progressive MS. A hole in the EBV-infected brain and CD8+ T-cell hypothesis is why patients do so well on natalizumab, and why does anti-CD20 therapy prevent rebound post-natalizumab?
If the brain were infected with EBV and you blocked immune surveillance using natalizumab, surely you could expect some ill effects? We don’t see this happening from a clinical perspective, at least in the short to intermediate term. In fact, we know the opposite happens; pwMS on natalizumab usually have no evident inflammatory disease activity (NEIDA) and many of them experience an improvement in disability. After rebaselining brain volume loss on natalizumab, it is close to the normal range, and fatigue and/or sickness behaviour improve. Surely, these observations argue against a direct CNS infection as being the cause of MS? Maybe not. Natalizumab may reduce smouldering MS, but it does not stop smouldering MS, which, in my opinion, is the real MS, and this may take many decades to manifest itself. It is common to see patients who have been on natalizumab for a decade or more with worsening MS and worsening brain volume loss.
Suppose MS is due to EBV-specific CD8+ cytotoxic T-lymphocytes attacking the brain of pwMS. Why does rituximab, a drug that takes out predominantly B-cells, prevent rebound disease activity post-natalizumab? Some have argued that the B-cells are needed to travel to the brain to present antigen to the CD8+ T-cells. I don’t buy this explanation, as there are other professional antigen-presenting cells in the brains of pwMS that can take on this role. Others cite evidence that T-cells require assistance from B-cells to cross the blood-brain barrier. This does not explain why some of the carry-over PML cases from natalizumab to rituximab (or ocrelizumab) have developed IRIS (immune reconstitution inflammatory syndrome). In the latter instances, IRIS-causing T-cells have clearly trafficked to the brain in the absence of circulating B-cells.
So these papers generate more questions than they necessarily answer. Still, it does demonstrate that we need to really find out if EBV is driving MS from within the CNS or from its effects on the immune system in the periphery. These two scenarios require different treatment approaches. However, this should not stop us from exploring both approaches; it is the results of the experiment that disprove the hypothesis. This is why we need to be exploring both EBV-specific antiviral agents and a therapeutic EBV vaccine as potential treatments for MS.
Leprosy hypothesis of MS:
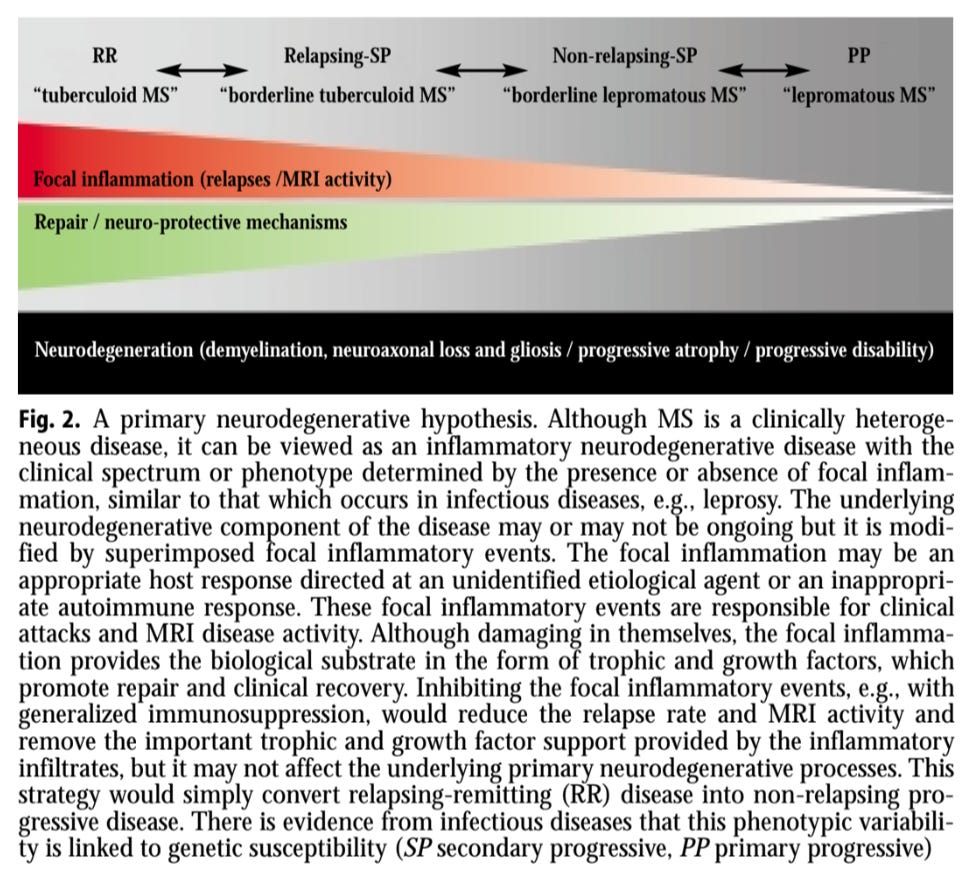
Leprosy is an infectious disease caused by a bacterium with a well-defined set of antigens that can be used to interrogate the adaptive immune system’s responses to antigens. Depending on the immune response, you get a different clinical picture. If you have a brisk inflammatory response, you get tuberculoid leprosy, which presents with inflamed lesions. On the other side of the spectrum, you get lepromatous leprosy, which is more of a smouldering disease with low-grade inflammation. Between these two extremes, you get a grey zone called borderline subtypes. Interestingly, people can convert from having lepromatous to tuberculoid leprosy if they shift their immune response to a so-called type 1 immune response driven by interferon-gamma.
I view primary progressive MS as lepromatous MS and relapsing-remitting MS as tuberculoid MS. The SPMS sits in the middle and is borderline MS. Interestingly, gamma interferon seems to have the same effect in MS as in leprosy, driving lepromatous MS (PPMS) to become tuberculoid or relapsing MS. The trial of gamma-interferon in MS was stopped because it causes subjects to have relapses. The corollary is that immunosuppressive treatments of relapsing MS suppress relapses but do not stop smouldering or the real MS. In other words, immunosuppressive therapies convert relapsing MS into PPMS. To test the leprosy hypothesis of MS, we would need to know the autoantigen or inciting organism driving MS. Despite decades of research, we have yet to find the MS autoantigen. I doubt we will see an autoantigen, so we should instead focus on the most likely cause of MS, EBV.
For more information on the leprosy hypothesis of MS, please read paper 6 below.
Conclusion
From the few examples discussed above, it is clear that Gemini missed many of the alternative theories of what is driving smouldering MS or the ‘inside-out hypothesis’ of MS. I have only scratched the surface on this topic and will give some additional thoughts on this topic in the future.
However, I am biased! I am firmly in the ‘Inside-Out’ camp and think EBV can explain a lot of the observations above. This is why I am trying to develop, or help develop, with little success, treatments for MS targeting EBV and strategies targeting EBV to prevent MS.
I would like to know what you think of this newsletter compared to the AI-generated one. Do I still have a role? Does MS-Selfie have a future? Do you like these blue-sky type newsletters? Are they too scientific or off-topic for you?
Thanks
Paper 1 - Stereotypical relapses
Paer 2 - Gamma interferon
Paper 3 - Case study 1 - lytic EBV infection with natalizumab rebound
Paper 4 - Case study 2 - lytic EBV infection with natalizumab rebound
Paper 5 - Case series
Paper 6 - Leprosy hypothesis
Accidental readers
If you have been forwarded this email and are not an MS-Selfie subscriber, please consider subscribing and helping MS-Selfie expand its resources for the broader MS community. MS-Selfie relies on subscriptions to fund its curated MS-Selfie microsite, MS-Selfie books, MS-Selfie Infocards, and other activities that extend beyond the MS-Selfie Substack newsletters.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite and other related activities, as I don’t have time to do this myself. You must be a paying subscriber to ask questions unrelated to the newsletters or podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Questions
If you have questions unrelated to the newsletters or podcasts, please email them to ms-selfie@giovannoni.net. Prof. G will try to answer them as quickly as possible.
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.



Emaill: "Possible typo?:
'Natalizumab may reduce smouldering MS, but it does not stop smouldering MS, which, in my opinion, is the real MS, and this may take many decades to manifest itself.'
Is the first line relapsing ms?"
No. PwMS treated with natalizumab have reduced brain volume loss and reduced microglial activation on TSPO-PET imaging, which are biomarkers of smouldering MS. It is clear smouldering MS is reduced by natalizumab, but not stopped.
Thanks for your comments on AI blind spots on the question of 'Inside out' and bacterial toxins. What you get clearly depends on who you ask and how you put your question! I was astonished by the insightful and comprehensive response I got using 'Google studio' , asking the question, What is the significance of Staph aureus sphingomyelinase in relation to the high rate of Multiple sclerosis on the Orkney islands? If you anticipate asking more questions on this topic, you may also find it useful! Very best wishes. I really don't know how you manage to keep up with all of this !!