How useful is AI-generated content in the field of MS?
I have been having a back-and-forth argument with colleagues about the value of AI in MS research. I therefore asked Google Gemini Pro 2.5 Deep Research the following question:
I have been having a back-and-forth argument with colleagues about the value of AI in MS research. I therefore asked Google Gemini Pro 2.5 Deep Research the following question:
“Is there an alternate theory of multiple sclerosis, other than the autoimmune theory, that posits that Gadolinium-enhancing lesions are actually not the disease but the immune response to what is causing multiple sclerosis?”
The following is an edited version of the output. Please read it and tell me what is wrong with it; i.e. has Gemini misunderstood the literature, is there something missing, if you could, what would you add to the output? I will then write my own counterargument once we have discussed Gemini’s answer. You can then tell me if I still have a role in this brave new world dominated by information and increasingly by AI-generated slop.
"AI slop" refers to low-quality, generic, and often inaccurate media (text, images, video) produced by artificial intelligence. A lack of effort or expertise characterises this content, flooding the internet with unoriginal and unhelpful material that can be repetitive, verbose, or contain factual errors. The term has a pejorative connotation, similar to "spam," and highlights the problem of AI being used without sufficient human oversight or meaningful input.”
Thank you.
Summary
Multiple Sclerosis (MS) is predominantly understood and managed as a primary autoimmune disease of the central nervous system (CNS). This conventional paradigm, often referred to as the "outside-in" model, posits that an aberrant peripheral immune response triggers an inflammatory attack on myelin and oligodendrocytes, resulting in the characteristic demyelination and neurodegeneration. Within this framework, the appearance of Gadolinium-enhancing (Gd+) lesions on magnetic resonance imaging (MRI) is considered the definitive radiological hallmark of active disease—the direct visualisation of the primary pathogenic event. However, this autoimmune hypothesis, while considered robust, faces significant scientific challenges and does not fully satisfy the rigorous criteria for a classical autoimmune disorder.
In response to these challenges, a compelling alternative aetiological framework has emerged: the "inside-out" hypothesis. This model posits that MS originates not in the immune system, but as a primary degenerative process within the CNS itself. This hypothesis reinterprets Gd+ lesions not as the cause of the disease, but as a visible manifestation of the immune system's secondary response to an underlying, non-inflammatory pathology.
The key points are as follows:
The prevailing autoimmune theory of MS is incomplete. Despite its widespread acceptance, it fails to identify a universal autoantigen, is not fully replicated in animal models, and lacks the strong association with other autoimmune conditions that characterise classical autoimmune diseases. These weaknesses necessitate the exploration of alternative models.
The "inside-out" hypothesis is supported by a growing body of evidence indicating that significant pathology occurs within the CNS before the arrival of peripheral immune cells. Candidate mechanisms for this primary insult include the premature death of myelin-producing cells (oligodendrocyte apoptosis), a failure of essential cellular logistics within nerve fibres (axonal transport defects), and a fundamental collapse of cellular energy production (mitochondrial dysfunction).
This alternative model reframes the interpretation of Gd+ lesions. Rather than representing the primary autoimmune assault, they are viewed as a consequence of the disease—a marker of the inflammatory "cleanup" crew arriving at a site of pre-existing neurodegenerative crisis. This reinterpretation has profound implications for diagnosis and therapeutic strategy, suggesting that the actual target for treatment should be neuroprotection and metabolic support, not solely immunomodulation.
The current dogma: Gadolinium enhancement as a marker of primary autoimmune insult ("Outside-In" model)
The prevailing understanding of MS is rooted in the "outside-in" hypothesis, a framework that defines the disease as an organ-specific, immune-mediated disorder of the central nervous system. This model provides a coherent, albeit incomplete, narrative for the disease's pathogenesis, diagnosis, and treatment, with the Gadolinium-enhancing (Gd+) lesion serving as its central radiological pillar.
The pathophysiological cascade
According to the "outside-in" model, the pathogenic cascade of MS begins in the periphery, outside the CNS. It is hypothesised that in genetically susceptible individuals, an environmental trigger—most notably a viral infection such as Epstein-Barr Virus (EBV)—leads to the activation of autoreactive lymphocytes, specifically T-cells and B-cells, that mistakenly recognise components of CNS myelin as foreign.
These activated immune cells circulate in the bloodstream and migrate to the CNS. A crucial step in this process is the breach of the blood-brain barrier (BBB), a highly selective border that usually protects the brain from systemic inflammation and pathogens. Once across the BBB, these T-cells and B-cells orchestrate a complex inflammatory attack. T-cells release pro-inflammatory chemicals (cytokines) that cause direct damage and recruit other immune cells, such as macrophages, to the site. B-cells can mature into plasma cells that produce antibodies against myelin and also function as potent antigen-presenting cells, further amplifying the T-cell response.
This coordinated assault results in a cascade of pathobiological events: focal lymphocytic infiltration, activation of resident CNS immune cells (microglia), and the hallmark destruction of the myelin sheath (demyelination) and the cells that produce it (oligodendrocytes). While axons are often relatively spared in the initial stages, they are not immune to damage. The inflammatory environment, coupled with the loss of trophic support from myelin, leads to acute axonal injury and, over time, irreversible axonal transection and neuronal loss, which are the primary substrates of permanent neurological disability.
The radiological correlate—the Gd+ Lesion
Within this well-established paradigm, the Gd+ lesion, visualised on T1-weighted MRI scans, is the definitive in vivo biomarker of active, focal inflammation and is interpreted as the direct radiological signature of the primary disease process. Gadolinium-based contrast agents (GBCAs) are large molecules that, under normal physiological conditions, cannot cross the intact BBB. Their appearance within the brain parenchyma on an MRI is therefore unequivocal evidence of a localised BBB breakdown. In the "outside-in" model, this breakdown is a direct consequence of the inflammatory attack. Cytokines released by infiltrating immune cells increase the permeability of the local blood vessels, allowing both the immune cells and the injected gadolinium to leak into the CNS tissue. The gadolinium accumulates in the area of acute inflammation, causing a shortening of the T1 relaxation time and appearing as a bright (hyperintense) signal on T1-weighted images. This enhancement is a transient phenomenon, typically lasting 2-6 weeks, after which the inflammation subsides and the BBB begins to repair itself, causing the enhancement to fade.
The clinical utility of Gd+ lesions is deeply embedded in the diagnosis and management of MS. A Gd+ lesion is considered a reliable marker of a new or reactivating MS plaque, signifying acute disease activity at the time of the scan. Its presence is often correlated with clinical relapses, although many enhancing lesions can be clinically silent, depending on their location and size. The detection of Gd+ lesions is a cornerstone of the McDonald diagnostic criteria, the international standard for diagnosing MS. The presence of a Gd+ lesion on a baseline MRI scan can fulfil the criterion for "dissemination in time," allowing for a definitive diagnosis of MS even after a single clinical event (a clinically isolated syndrome) by demonstrating that pathological processes are ongoing.
Furthermore, the count and volume of Gd+ lesions are critical endpoints in clinical trials for disease-modifying therapies (DMTs). The efficacy of a new drug is often measured by its ability to reduce or eliminate the formation of new Gd+ lesions. In clinical practice, the appearance of new Gd+ lesions in a patient on therapy is considered a sign of breakthrough disease activity. It usually prompts a switch to a more potent medication. The evolution of these lesions is also tracked over time. An acute Gd+ lesion typically leaves behind a permanent, non-enhancing scar visible as a hyperintense area on T2-weighted or FLAIR sequences. In cases of severe tissue destruction, the lesion may evolve into a T1-hypointense "black hole," which signifies axonal loss and gliosis and is associated with worse long-term disability.
The entire clinical and research framework for MS is thus built upon the foundational assumption that Gd+ enhancement is a direct and reliable proxy for the primary disease process. The logic is straightforward: if the disease is a primary inflammatory attack, and Gd+ enhancement visualises this attack, then stopping the formation of Gd+ lesions is equivalent to halting the disease. This rationale has successfully guided the development of a large arsenal of anti-inflammatory and immunomodulatory DMTs. The success of these therapies in reducing relapses and Gd+ lesion formation has, in turn, created a powerful feedback loop, reinforcing the validity of both the "outside-in" model and the interpretation of the Gd+ lesion as its primary radiological manifestation. This makes it exceptionally difficult to consider alternative interpretations without questioning the very foundations of modern MS care.
Foundational cracks: a critical appraisal of the autoimmune hypothesis
While the "outside-in" model presents a compelling narrative and has led to effective treatments for the inflammatory aspects of MS, the classification of MS as a classical autoimmune disease is built on a foundation with significant and persistent cracks. A rigorous examination of the evidence reveals that MS fails to meet several key criteria that define canonical autoimmune disorders, suggesting that the role of the immune system, while undeniably central, may be more complex than that of a primary, unprovoked aggressor.
Failure to meet Witebsky's postulates for autoimmunity
Decades of intensive research have yielded a wealth of information about the immune-mediated nature of MS. Yet, the evidence remains circumstantial when held against the established criteria for defining an autoimmune disease.
The missing autoantigen
A fundamental criterion for any given autoimmune disease is the identification of a precise autoantigen—a specific self-molecule targeted by the immune system—that is present in all patients with the disease. In myasthenia gravis, this is the acetylcholine receptor; in neuromyelitis optica (NMO), it is the aquaporin-4 water channel. Despite exhaustive efforts to identify a similar target in MS, focusing on myelin components like myelin basic protein (MBP), proteolipid protein (PLP), and myelin oligodendrocyte glycoprotein (MOG), as well as various lipids and gangliosides, no single, confirmed autoantigen has been universally identified in all MS patients. This absence of a specific target is a significant departure from the classical autoimmune model.
Ambiguous animal models
The primary animal model for MS, Experimental Autoimmune Encephalomyelitis (EAE), is induced by immunising animals with myelin antigens, which then triggers a CNS-directed immune attack. While EAE has been invaluable for studying the mechanisms of neuroinflammation, it has limitations as a model for a spontaneous human disease. Critically, the disease process in EAE can be induced by multiple different myelin antigens, with no single antigen proving superior or uniquely causative. Furthermore, attempts to passively transfer the disease to healthy animals by administering autoantibodies or autoreactive T cells from people with MS have produced conflicting and inconsistent results, failing to definitively prove a single, transferable pathogenic agent, as would be expected in a classic autoimmune disorder.
Lack of specificity in autoreactive cells
While it is true that patients with MS often have a higher frequency of T-cells that react to myelin antigens compared to healthy controls, particularly during relapses, this finding is not specific to the disease. Autoreactive T-cells capable of recognising myelin components can also be readily isolated from the blood of healthy individuals who show no signs of MS. Their mere presence, therefore, is not sufficient to prove causality. It suggests that the control of these potentially pathogenic cells, rather than their existence, is the critical factor, and that in MS, this control mechanism may fail.
Weak association with other autoimmune diseases
Patients with a confirmed autoimmune disease often have an increased risk of developing other autoimmune conditions. However, extensive, population-based cohort studies have generally failed to demonstrate a strong association between MS and the broader spectrum of autoimmune diseases. While some case reports exist, and a weak association with thyroid disease has been noted, MS does not typically cluster with conditions like systemic lupus erythematosus or Sjögren's syndrome in the way that these diseases cluster with each other. This again contrasts sharply with a disease like NMO, which has a clear autoimmune signature.
These persistent discrepancies between MS and classical autoimmune diseases do not negate the critical role of the immune system in MS pathology. The presence of perivascular inflammatory infiltrates, oligoclonal bands in the cerebrospinal fluid, and the apparent efficacy of immunomodulatory therapies all confirm that MS is an immune-mediated disease. However, the failure to satisfy these core criteria strongly suggests that the immune response may not be the primary, instigating event. If the immune system is not the unprovoked aggressor, then it must be reacting to something. This line of reasoning logically leads to the hypothesis that the autoimmune phenomena observed in MS are, in fact, a secondary response to a primary pathological process occurring within the CNS itself. This conceptual shift is the gateway to the "inside-out" hypothesis.
A paradigm shift: the "Inside-Out" hypothesis of MS
The "inside-out" hypothesis represents a fundamental re-conceptualisation of MS pathogenesis. It challenges the primacy of the immune system in the disease's origin and instead proposes that MS is initiated by an intrinsic, degenerative process within the central nervous system. In this model, the well-documented inflammation and autoimmune phenomena are not the cause of the disease, but rather a secondary, albeit highly consequential, reaction to this primary CNS cytodegeneration. This paradigm shift inverts the established causal relationship: degeneration precedes and provokes inflammation, rather than the other way around.
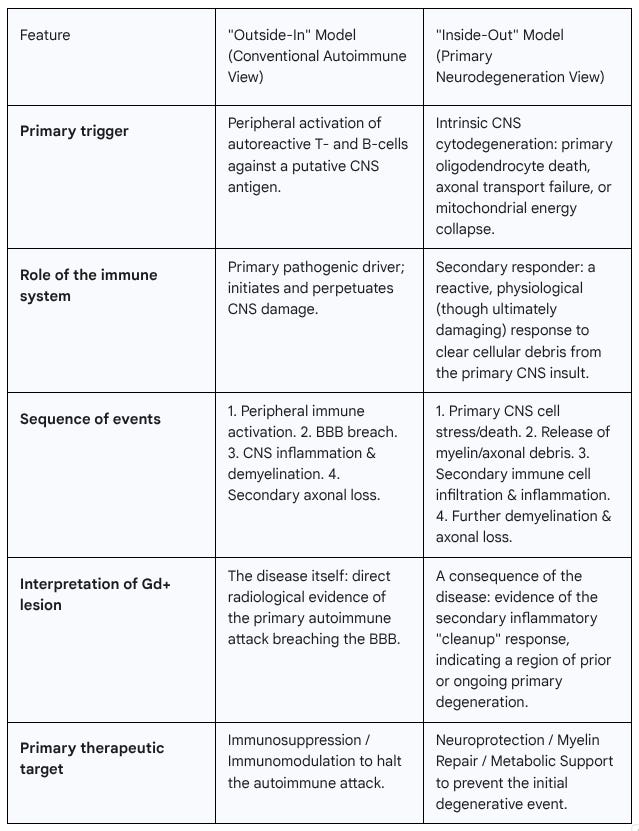
This alternative view presents a potential explanation for one of the significant paradoxes in MS clinical care: the disconnect between inflammation and disease worsening. Current disease-modifying therapies are remarkably effective at suppressing the inflammatory attacks that characterise relapsing-remitting MS (RRMS). Yet, they have a much more modest impact on the relentless accumulation of disability seen in advanced forms of the disease. The "inside-out" model suggests this is because these therapies target the secondary inflammatory response, leaving the underlying primary degenerative driver largely untouched. To frame the stark differences between the two competing paradigms, the following table provides a direct comparison.
Candidate mechanisms for the primary insult
The "inside-out" hypothesis is not a single theory but a framework that encompasses several potential mechanisms for the initial, non-inflammatory CNS injury. Research has converged on three particularly compelling candidates, which are not mutually exclusive and may interact to drive the disease process.
1. Primary oligodendrogliopathy (oligodendrocyte death)
There is substantial pathological evidence to suggest that the death of oligodendrocytes—the sole myelin-producing cells of the CNS—can be a very early event in MS lesion formation, occurring even before the mass infiltration of peripheral immune cells. Studies of early MS lesions have identified oligodendrocytes undergoing programmed cell death (apoptosis) in so-called "pre-phagocytic" areas, where there is microglial activation but a conspicuous absence of the T-cell and B-cell infiltrates that characterise a classic inflammatory lesion. In this scenario, an unknown stressor—perhaps metabolic, toxic, or viral—triggers apoptosis in vulnerable oligodendrocytes. The death of these cells leads to the destabilisation and subsequent breakdown of the myelin sheaths they support. This disintegration of myelin releases a host of proteins and lipids that are normally sequestered from the immune system. This release of cellular debris acts as a powerful danger signal, attracting and activating microglia and, eventually, the peripheral immune system to the site to clear the damage, thereby initiating the secondary inflammatory cascade. This model is supported by novel experimental systems where inducing apoptosis specifically in oligodendrocytes is sufficient to trigger rapid demyelination and a robust local microglial response, all in the absence of a primary autoimmune trigger.
2. Primary axonopathy (axonal dysfunction)
For many years, axonal damage in MS was considered a late and secondary consequence of inflammatory demyelination. However, it is now clear that axonal injury is an early and pervasive feature of the disease. The "inside-out" model posits that this axonal pathology may not be secondary at all, but rather a primary driver of the disease process. A key line of evidence comes from studies of axonal transport, the intricate logistical system that moves essential cargoes, such as mitochondria, proteins, and vesicles, along the length of the axon. In animal models of MS, profound defects in axonal transport have been shown to occur very early, preceding structural signs of axonal degeneration and even overt demyelination.
This suggests a primary metabolic or structural failure within the axon itself. Such a failure can initiate a devastating vicious cycle. Impaired transport of mitochondria starves the axon of adenosine triphosphate (ATP), the energy currency of the cell. This energy deficit is particularly damaging for axons, which have enormous energy demands to maintain ion gradients and propagate nerve impulses. This demand increases exponentially when the insulating myelin sheath is lost. The lack of ATP further cripples the energy-dependent molecular motors responsible for axonal transport, leading to a downward spiral of energy failure, accumulation of toxic protein aggregates, and eventual axonal degeneration. The debris from this degenerating axon would then, like the debris from a dying oligodendrocyte, trigger a secondary inflammatory response.
3. Mitochondrial dysfunction
A more fundamental "inside-out" trigger, potentially underlying both oligodendrogliopathy and axonopathy, is mitochondrial dysfunction. Mitochondria are the powerhouses of the cell, and the CNS, with its incredibly high metabolic rate, is exquisitely sensitive to any disruption in their function. A wealth of evidence points to widespread mitochondrial pathology in MS. Post-mortem studies of MS brain tissue and analyses of animal models reveal mitochondrial respiratory chain deficiencies, abnormalities in mitochondrial structure and transport, and a significant reduction in energy production capacity in both neurons and glial cells.
This systemic energy failure within the CNS could be the primary insult that initiates the entire pathogenic cascade. A deficit in ATP production can directly lead to the axonal transport failures described above. Dysfunctional mitochondria also produce an excess of damaging reactive oxygen species (ROS) and lead to dysregulation of intracellular calcium levels, both of which are potent triggers for apoptosis in oligodendrocytes. Therefore, a primary mitochondrial defect could simultaneously precipitate both oligodendrocyte death and axonal dysfunction, creating a perfect storm of cellular degeneration that culminates in a robust secondary inflammatory response. Recent research has highlighted explicitly that a reduction in mitochondrial activity in the cerebellum is a key contributor to the death of Purkinje cells, which are crucial for motor control, directly linking mitochondrial failure to the clinical symptoms of MS.
Reinterpreting the evidence: the Gd-enhancing kesion in the "Inside-Out" Context
The "inside-out" hypothesis does not dispute the physiological reality that a Gd-enhancing lesion represents: a focal area of acute inflammation and blood-brain barrier disruption. Instead, it radically redefines the lesion's meaning and significance within the broader narrative of the disease. In this context, the Gd+ lesion is transformed from the inciting incident into a secondary, reactive phenomenon—a late-stage marker of an underlying degenerative crisis that has already been unfolding silently.
According to the "inside-out" model, the appearance of a Gd+ lesion signifies the point at which a primary, smouldering neurodegenerative process—be it oligodendrocyte death, axonal failure, or mitochondrial collapse—reaches a critical threshold. At this point, the amount of cellular death and the accumulation of myelin and axonal debris become substantial enough to trigger a full-blown inflammatory response from the CNS's resident immune cells (microglia) and, subsequently, the peripheral immune system. This inflammatory response, while likely intended to be a reparative "cleanup" operation, is itself damaging and is responsible for the acute BBB breakdown that allows gadolinium to enter the tissue.
This sequence of events—degeneration followed by inflammation—is supported by several lines of evidence:
Animal models: The Cuprizone Autoimmune Encephalitis (CAE) model provides compelling experimental support. In this model, mice are first treated with cuprizone, a toxin that induces a subtle myelin perturbation and oligodendrocyte injury without causing overt demyelination or inflammation. Only after this primary, non-inflammatory insult is established is an immune challenge administered. This challenge then precipitates a robust inflammatory demyelination, complete with BBB breakdown and Gd+ enhancement on MRI. This model elegantly demonstrates that a primary CNS pathology can precede and directly cause a secondary inflammatory event that is radiologically identical to a classic MS lesion.
Human neuropathology: Pathological examination of human MS brain tissue has revealed the existence of "pre-active lesions." These are areas characterised by clusters of activated microglia and evidence of early myelin damage and axonal injury. Still, crucially, they lack the significant infiltration of T-cells and B-cells from the periphery. These pre-active lesions are thought to represent the initial stage of lesion formation. This "inside-out" degenerative process has not yet triggered the full-scale adaptive immune response that would lead to Gd+ enhancement. They provide a pathological snapshot of the disease process before the arrival of the inflammatory cavalry.
Radiological evidence supporting a neurodegeneration-first model
While the Gd+ lesion is the most dramatic radiological finding, other, more subtle MRI features lend support to the idea of a primary, widespread degenerative process.
Normal-appearing white matter (NAWM): Proponents of the "inside-out" model emphasise that the focal lesions visible on conventional MRI are not the whole story. Using advanced, quantitative MRI techniques, researchers have demonstrated subtle but widespread pathological changes throughout the so-called "normal-appearing" white matter of MS patients—areas that are distant from any focal inflammatory lesions. These changes in NAWM suggest a diffuse, global CNS pathology, a slow-burning degenerative process that affects the entire brain. From this perspective, the focal Gd+ lesions are merely the "tip of the iceberg," representing localised hotspots where this underlying degenerative process has flared up to a degree that necessitates a visible inflammatory response. This helps to explain the well-known clinico-radiological paradox, where patients can accumulate significant disability over time even in the absence of new Gd+ lesions, as the disability is driven by the "smouldering" degeneration occurring in the NAWM.
Central vein sign: The observation that the vast majority of MS lesions are perivenular, meaning they form around a small central vein, is a key radiological feature. This "central vein sign" is compatible with both pathogenic models. In the "outside-in" view, the vein is the portal of entry through which autoreactive immune cells leave the bloodstream and enter the brain. In the "inside-out" view, the perivenular space, which is part of the brain's glymphatic waste clearance system, could be where metabolic byproducts and cellular debris from a primary degenerative process accumulate. This accumulation of "danger signals" in the perivenular space would then trigger a localised inflammatory response, explaining why the lesions form in this specific anatomical location.
Re-evaluating clinical practice: In recent years, there has been a significant clinical and regulatory debate regarding the necessity of routine gadolinium administration for monitoring MS patients, driven by concerns about long-term gadolinium deposition in the brain. Many experts now advocate for a reduced-gadolinium or gadolinium-free monitoring strategy, focusing instead on the appearance of new or enlarging lesions on T2-weighted sequences. T2 lesions represent the permanent "footprint" or scar left by a pathological event, reflecting cumulative tissue damage and demyelination. This clinical shift, whether intentional or not, aligns with the "inside-out" perspective. It implicitly prioritises the measurement of irreversible tissue destruction (T2 lesions) over the measurement of the transient inflammatory response (Gd+ lesions), acknowledging that it is the former, not the latter, that is the ultimate driver of long-term disability.
In summary, the "inside-out" model does not change what a Gd+ lesion is—it remains a sign of inflammation and BBB breakdown. However, it fundamentally changes what a Gd+ lesion means. It is no longer the fire itself, but rather the smoke signalling a pre-existing, and arguably more critical, degenerative fire burning silently within the CNS.
A broader view: survey of other aetiological theories and contributing factors
While the "outside-in" versus "inside-out" debate forms the central axis of current thinking on MS pathogenesis, several other theories and risk factors contribute to a more complete, albeit complex, picture. These factors often do not stand as independent theories but can be integrated as potential triggers or modulators within either of the two main paradigms.
The infectious hypothesis: trigger or cause?
The link between viral infection and MS is one of the most robust findings in the field of epidemiology. The Epstein-Barr virus (EBV), the cause of infectious mononucleosis, has emerged as the leading candidate. A large body of evidence now indicates that EBV infection is an essential prerequisite for the development of MS; the disease is exceedingly rare in individuals who have never been infected with the virus.
However, the precise role of EBV remains a subject of intense investigation and debate.
As an "Outside-In" trigger: EBV could initiate the disease via "molecular mimicry." In this scenario, the immune system mounts a normal response to the virus, but some components of EBV bear a structural resemblance to proteins in CNS myelin. This could lead to cross-reactivity, where T-cells and B-cells primed to attack the virus mistakenly target the myelin sheath, initiating the autoimmune cascade.
As an "Inside-Out" contributor: Alternatively, EBV establishes a lifelong latent infection, primarily within B-cells. It is plausible that these latently infected B-cells, which can reside within the CNS, contribute to a primary "inside-out" process over many years. The presence of the virus could induce chronic cellular stress, alter B-cell function, or periodically reactivate, contributing to a pro-inflammatory microenvironment that could eventually trigger neurodegeneration.
Other infectious agents, such as human herpesvirus-6 (HHV-6), have also been implicated, though the evidence is less compelling than for EBV.
The vascular hypothesis: the rise and fall of CCSVI
For a period, a vascular theory of MS gained significant public attention. The theory of Chronic Cerebrospinal Venous Insufficiency (CCSVI), proposed by Dr. Paolo Zamboni, hypothesised that MS was caused by impaired venous drainage from the CNS due to stenoses (narrowings) in the jugular and azygos veins. This venous obstruction was thought to cause blood to reflux back into the brain, leading to perivenular iron deposition, which in turn triggered a secondary inflammatory response and demyelination. The proposed treatment was a vascular procedure called "liberation therapy," an angioplasty to open the narrowed veins. The scientific community has largely refuted the CCSVI hypothesis. Subsequent, more rigorous, blinded, and larger-scale studies failed to replicate the initial findings. These studies found that the proposed venous abnormalities were not more common in people with MS than in healthy controls or individuals with other neurological diseases. Randomised controlled clinical trials of the "liberation therapy" demonstrated no clinical benefit for MS patients and, in some instances, were associated with serious adverse events, including venous thrombosis and stent migration. CCSVI is no longer considered a credible cause of MS.
The metabolic and environmental milieu
A range of environmental and lifestyle factors are known to modulate the risk of developing MS and influence its course. These factors likely contribute to either immune dysregulation (favouring an "outside-in" process) or CNS vulnerability (favouring an "inside-out" process).
Vitamin D deficiency: A low level of vitamin D, often linked to reduced sun exposure in higher latitudes, is one of the most well-established environmental risk factors for MS. Vitamin D has known immunomodulatory effects, and its deficiency may predispose individuals to autoimmune responses. It may also play a direct role in CNS health and repair, meaning its absence could increase the brain's vulnerability to a primary degenerative insult.
Metabolic factors: Obesity, particularly in childhood and adolescence, and cigarette smoking are strongly linked to an increased risk of developing MS and to a more rapid disease progression. Both factors promote a state of chronic, low-grade systemic inflammation and oxidative stress, which could lower the threshold for either a peripheral autoimmune attack or an intrinsic CNS degenerative process to take hold.
Faulty lipid metabolism: An intriguing, though less mainstream, theory posits that MS may be a primary metabolic disorder of faulty lipid metabolism. Since myelin is composed predominantly of lipids, a systemic defect in lipid processing could lead to the production of unstable myelin, making it prone to spontaneous breakdown and subsequent inflammatory scavenging. This theory frames MS as being more analogous to a metabolic disease like atherosclerosis than to a classical autoimmune disease.
These contributing factors underscore the complexity of MS aetiology, suggesting that the disease arises from a complex interplay between genetic predisposition, environmental exposures, and lifestyle, which together create the conditions for either a primary autoimmune or a primary neurodegenerative process to unfold.
Future directions: toward a unified model
The intense debate between the "outside-in" and "inside-out" paradigms of MS should not be viewed as a zero-sum contest in which one theory must wholly vanquish the other. Instead, the accumulated evidence points toward a more nuanced and complex reality. Reconciling these two models may be the key to understanding the disease and developing more effective, personalised treatments.
Reconciling the paradigms
A unified model would propose that both "outside-in" and "inside-out" mechanisms are valid, with their relative contributions varying between patients and over the course of the disease in a single patient.
Relapsing-Remitting MS (RRMS): The most common form of the disease at onset, RRMS is characterised by discrete inflammatory attacks (relapses) followed by periods of recovery (remission). This clinical picture, with its dramatic, Gd-enhancing inflammatory lesions and strong response to immunomodulatory therapies, aligns well with the "outside-in" model. In these patients, a primary dysregulation of the peripheral immune system may indeed be the dominant driver of disease activity in the early stages.
Primary Progressive MS (PPMS): A smaller subset of patients experiences a progressive accumulation of disability from the very onset of the disease, without clear relapses. PPMS is characterised by less focal inflammation on MRI and a notoriously poor response to most anti-inflammatory DMTs. This form of the disease may represent a purer manifestation of the
"inside-out" model, where a primary, relentless neurodegenerative process is the main driver, with inflammation playing a more subdued, secondary role.Secondary Progressive MS (SPMS): Many patients who begin with RRMS eventually transition to a secondary progressive course, where disability accrues steadily, independent of relapses. This transition could represent the point at which an initially "outside-in" inflammatory process triggers a self-sustaining "inside-out" neurodegenerative cascade. Chronic inflammation and repeated insults to the CNS may exhaust its metabolic and repair capacity, initiating a primary degenerative process that becomes uncoupled from peripheral immune attacks and is therefore refractory to standard immunomodulatory treatments.
Implications for research and therapeutics
Accepting this heterogeneous model of MS has implications for the future of research and clinical care. The central challenge shifts from identifying a single cause to developing tools that can dissect the dominant pathogenic pathway in an individual patient.
Implications for research: The field must move beyond Gd+ lesions as the sole biomarker of disease activity. The research focus must expand to include the development and validation of biomarkers capable of detecting and quantifying the primary "inside-out" processes. This includes:
Advanced neuroimaging: Utilising quantitative MRI techniques to measure subtle changes in normal-appearing white and grey matter, which may reflect the underlying degenerative process.
Metabolic and molecular markers: Developing blood or cerebrospinal fluid tests for markers of mitochondrial stress, axonal injury (such as neurofilament light chain, sNfL), and oligodendrocyte damage.
Refined animal models: Employing a combination of animal models—both traditional EAE ("outside-in") and toxin-induced models like cuprizone ("inside-out")—to test therapies that target different aspects of the disease process.
Implications for therapeutics: The "inside-out" paradigm necessitates a fundamental shift in therapeutic strategy, particularly for progressive MS. While immunomodulation will continue to be an important tool for controlling the inflammatory component of the disease, it is clearly insufficient for halting disease progression. The ultimate goal must be to develop and deploy a new class of drugs that target the primary degenerative process itself. The therapeutic pipeline must prioritise:
Neuroprotective agents: Drugs that can shield axons and neurons from metabolic stress, oxidative damage, and excitotoxicity.
Mitochondrial support: Therapies aimed at boosting mitochondrial function and energy production within CNS cells.
Remyelinating agents: Compounds that can promote the differentiation of oligodendrocyte precursor cells and enhance the natural process of myelin repair, which is known to be inefficient in MS.
Conclusions
The "inside-out" framework, which posits a primary neurodegeneration that secondarily elicits an immune response, provides a compelling explanation for the shortcomings of the conventional autoimmune model and the clinical realities of progressive MS. Viewing the Gd+ lesion as a consequence rather than a cause challenges the very foundations of MS diagnosis and treatment. This paradigm shift provides a crucial conceptual roadmap for future research and, most importantly, for the development of innovative neuroprotective and reparative therapies that hold the promise of finally halting the relentless degenerative process that underpins long-term disability in MS.
Questions to you, the reader
Has Gemini misunderstood the literature? Is there something missing? If you could, what would you add to the output?
Thank you
Accidental readers
If you have been forwarded this email and are not an MS-Selfie subscriber, please consider subscribing and helping MS-Selfie expand its resources for the broader MS community. MS-Selfie relies on subscriptions to fund its curated MS-Selfie microsite, MS-Selfie books, MS-Selfie Infocards, and other activities that extend beyond the MS-Selfie Substack newsletters.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite and other related activities, as I don’t have time to do this myself. You must be a paying subscriber to ask questions unrelated to the newsletters or podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Questions
If you have questions unrelated to the newsletters or podcasts, please email them to ms-selfie@giovannoni.net. Prof. G will try to answer them as quickly as possible.
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.



A long read which I skimmed.
I suspect Charcot, c.130 years dead, would be turning in his grave.
Recent thinking has suggested that MS is one disease. Yet this ‘one disease’ has yet to be cracked despite unbelievable advances in imaging, computer power…. What have 40 ECTRIMS annual meetings really achieved? Did the recipients of the Barancik and John Dystel prizes really deserve them given the most basic questions about this one disease have yet to be answered?
MSers wanted one thing from the 4-5 decades of well funded research - to stop the underlying neuro-degeneration which leads to unrelenting disability progression. Some even hoped for a degree of neuro-restoration. Yet the drugs (the MS drugs market is projected to grow to c.$41 billion by 2032)to date have only tackled relapses not the neurodegeneration. Relapses were the low hanging fruit.
The MS Society websites claim that ‘there’s never been a better time to get MS’ and ‘MS research has never been so exciting’. Yet, in 2025, MSers are still moving from crutches to manual wheelchairs to electric wheelchairs. My GP visits two women with MS in their mid-30s who are in care homes. The use of AI in MS research will make little difference to them.
MS is often portrayed as the poster child of neurological diseases. Not difficult given the dire progress relating to MND, Parkinson’s and Huntington’s. But with so many basic questions yet to be answered, the MS research field needs a shake up and a kick up the backside. Too many broken promises (remember NMSS Promise 2010?), too many progressive MS trial failures (MS Smart, MS Stat)…… I hope that AI doesn’t just generate another thousand+ rabbit holes to keep Professors of neuro-immunology, ever expanding research teams, and an army of PhD students busy for the next 25-30 years.
Thanks so much for this very important and relevant post. I have been a believer in the "inside-out" model of MS for a long time, but there do not seem to be many in the MS community who believe this model. I personally believe that what I refer to as the "conventional MS model" (the "outside-in"/MS as a primary autoimmune disease) was created and exists to benefit the "medical-pharmaceutical-industrial" complex in that it allows and supports the pushing of the immunosuppressive and/or immunomodulatory MS "DMTs" and places the most emphasis on relapses and new conventional MRI activity, such as Gd+-enhancing lesions. I have always disagreed with the USA FDA's labeling indications for the DMTs that state "for the treatment of relapsing forms of MS" (*or in the case of Ocrevus, PPMS), because as I see it, the "DMTs" do NOT "treat MS"-rather, they reduce some manifestations of active inflammation: relapses and new conventional MRI activity. If MS were to be seen, classified, and treated as a primary neurodegenerative disease, at this time, I do not believe there would be any "treatments"-it would be a similar situation to ALS, frontotemporal dementia, Alzheimer's, etc, where the focus would be on any DMTs that might be able to "slow progression," which has not been the primary endpoint of MS DMT trials, except for some trials specifically for progressive forms of MS. It would be MUCH harder and more expensive and time-consuming for the pharma companies to try to come up with "treatments" for MS as a primary neurodegenerative disease vs a primary autoimmune disease.
I would love to hear your thoughts about this and if you feel we will see a shift in the MS community (esp among clinicians, researchers, regulatory bodies, pharma companies, etc) towards the "outside-in" model and away from the "inside-out" model.
Thank you!