Gavinitis or flipping the pyramid
‘Gavinitis’ refers to adopting a treatment strategy of offering and potentially starting your patients with multiple sclerosis on high-efficacy DMTs first-line.
After attending ECTRIMS 2023, it is clear that the argument about early treatment has been won. I would be surprised if anyone in the broader MS community would argue that there is a rationale for delaying starting treatment in someone with active MS. Despite this, there are problems in healthcare systems that result in unnecessary delays in people with MS being diagnosed and treated. This could be due to medical gaslighting and/or delays in getting referred to a neurologist for a diagnostic work-up, followed by further delays in being referred to an MS expert for treatment initiation.
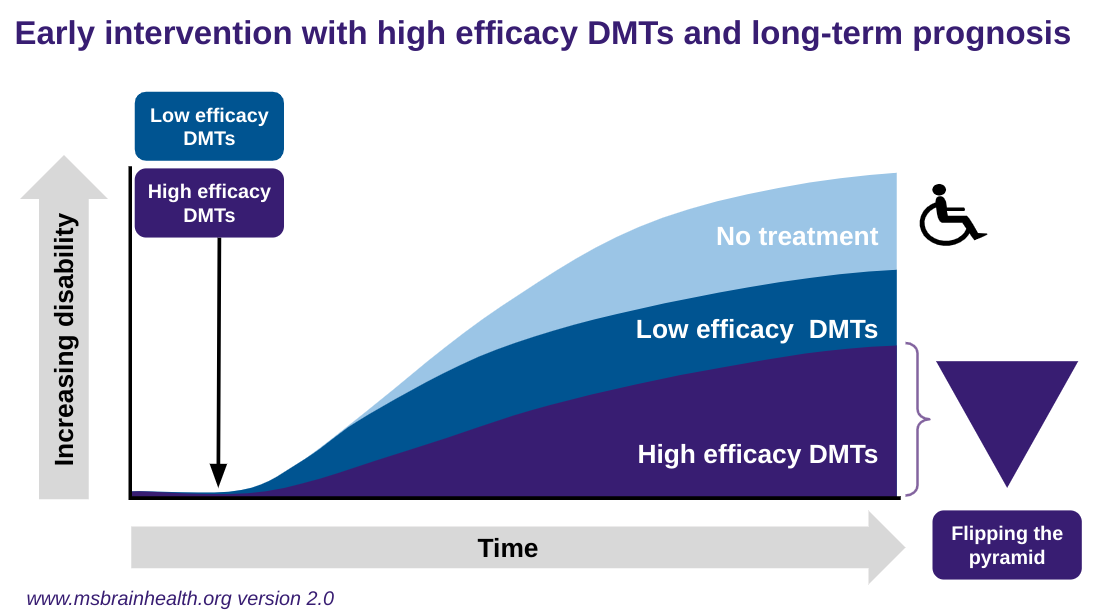
The next battle is getting the MS community to accept flipping the pyramid, i.e. offering and starting someone on high-efficacy treatment first-line to give them the best chance of optimising their MS outcome. The data supporting flipping the pyramid is now overwhelming.
I was surprised when another UK colleague diagnosed a close colleague and friend with ‘Gavinitis’. Apparently, this new affliction refers to adopting a treatment strategy of offering and potentially starting your patients with MS on high-efficacy DMTs first-line. This particular individual still thinks we have equipoise and that you can randomise patients to either a maintenance-escalation versus high-efficacy DMTs in a clinical trial to see who does better in the long-term. I hope this individual saw the stunning ocrelizumab open-label long-term extension data we presented at ECTRIMS.
After long-term (10 years) continuous ocrelizumab treatment, 8 out of 10 people with relapsing MS (PwRM) and a third of PwPPMS were progression-free using the EDSS. Greater than 90% of PwRMS did not need a walking aid (EDSS < 6.0), and >80% of PwPPMS did not need a wheelchair (EDSS < 7.0).
Most importantly, early treatment with ocrelizumab extends the progression-free event window by almost ten years in PwRMS, compared with starting treatment with interferon-beta-1a, a lower efficacy DMT, for the first two years. In comparison, earlyish treatment with ocrelizumab extends the progression-free event window by 1.6 years in PwPPMS, compared with a 2-year delay in starting treatment. Please note I use the term earlyish because pwPPMS are typically diagnosed ten years later than pwRMS. In other words, they are much further in the course of their disease and don’t benefit from early treatment. It is clear to me that MS in one disease and that by missing out on a sentinel event, i.e. an attack, pwPPMS have to wait until they run out of reserve in a particular neuronal pathway before being investigated and diagnosed as having MS.
It is galling to be diagnosed as having ‘Gavinitis’ when all you are trying to do is optimise the treatment of your patients. Maybe this particular neurologist will get his comeuppance when one of his patients complains that they have been mismanaged by being denied the option of high-efficacy first-line. What do you think? I find it sad that the management of MS is so variable and really depends on which healthcare professional you see. This is one of the reasons I started and continue to run MS-Selfie: to empower you with information to challenge the status quo.
If any funders read this newsletter, please support the next version of ‘Brain Health: Time Matters in MS’; it will help us fight therapeutic inertia and the entrenched contrarians unprepared to accept the overwhelming evidence that flipping the pyramid makes a difference in MS.
You are welcome to download the 10-year ocrelizumab OLE ECTRIMS poster here.
Please note the data above is all based on disability progression and not relapses and focal MRI activity, i.e. the real MS and not the immune system’s response to what is causing the disease. I stress this because we still have equipoise when using teriflunomide as an active comparator in clinical trials. For the arguments regarding this, please see my MS-Selfie Newsletter ‘Is it ethical to use teriflunomide as an active comparator in phase 3 trials?’ (14-Jun-2023). Finding out why teriflunomide disconnects relapses and focal MRI activity from disability worsening and brain volume loss is one of the ‘billion dollar’ questions that needs answering in MS.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if you want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.






Personally I hope neurologists everywhere catch a big dose of Gavinitis 😁. Thank you Gavin - you are so appreciated by PwMS.
I hope that Gavintis also develops into Gavintis Geriatricus as a sub-genre. I still don't understand the 60 year old cut off for the most effective DMDs when the evidence shows that 10 year efficacy most promising. Or are older people with MS expected to live with disability as a consequence of growing old? Why when surely the clinical and care costs would be less if MS continues to be treated? It is time older people were included in research and policy guidance since more than 50% of people with MS are over the age of 55 years.