Understanding your liver function tests or LFTs
How healthy is your liver? Do you know how to interpret your LFT blood results?
In light of my two recent Q&A newsletters on drug-induced liver disease (DILI), I thought I should provide you with a quick guide that explains how HCPs interpret basic liver function tests (LFTs) for people with multiple sclerosis (MS) on disease-modifying therapies (DMTs) and other drugs.
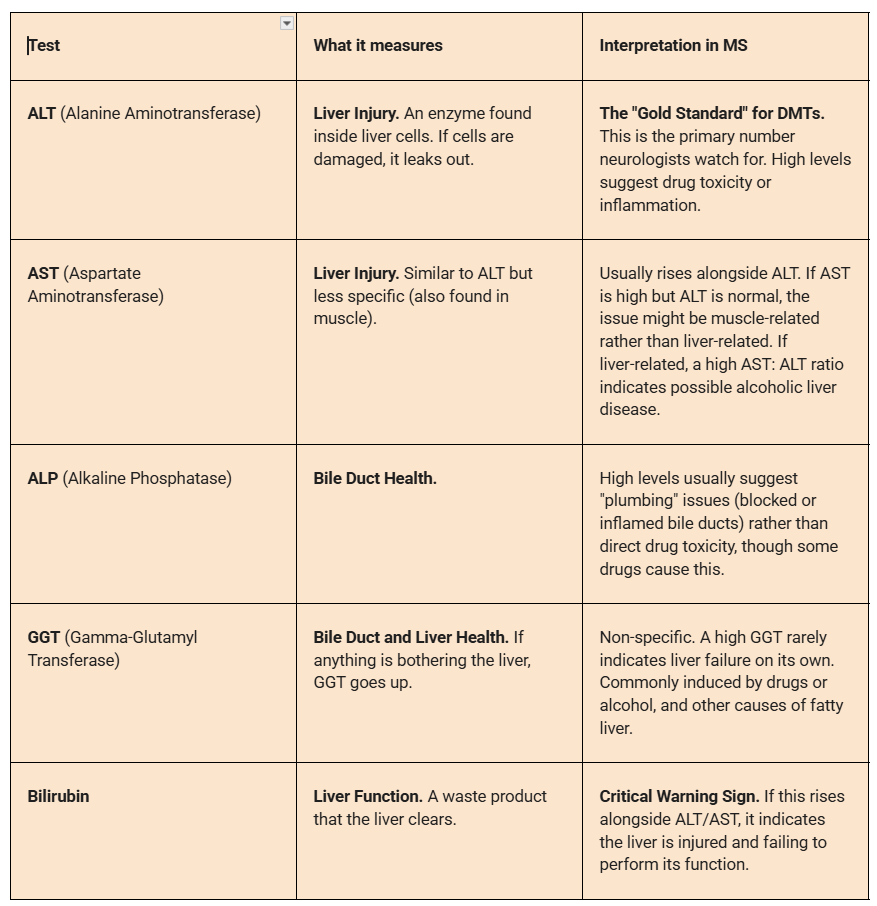
A standard hepatic or liver panel measures two things: liver Injury (leakage of enzymes) and liver function (how well it builds/processes things).
The “Traffic Light” system (the 3x rule)
In MS clinical trials and clinical practice, raw numbers matter less than the number of times they exceed the Upper Limit of Normal (ULN).
🟢 Green Zone (1x – 3x ULN):
Interpretation: Mild elevation. Very common, especially in the first 6 months of starting a new DMT (e.g. teriflunomide).
Action: Usually “watch and wait.” Treatment with the DMT typically continues, but the HCP is likely to retest in a month to ensure it stabilises.
🟡 Yellow Zone (3x – 5x ULN):
Interpretation: Moderate elevation. This is the threshold for concern.
Action: Caution. Your HCP will often re-test immediately to confirm. They may pause the DMT or increase monitoring frequency (e.g., every 2 weeks) until it drops.
🔴 Red Zone (>5x ULN OR “Hy’s Law”):
Interpretation: Severe elevation or potential liver failure.
Action: Stop. The DMT is usually discontinued immediately.
“Hy’s Law”: This is a critical safety rule. If a patient has ALT >3x ULN AND Bilirubin >2x ULN, it indicates a high risk of fatal drug-induced liver injury (DILI). This is a medical emergency and warrants referral to a hepatologist.
DMT summary for liver risks
Different MS drugs hit the liver in different ways.
Is it the drug or something else?
If your enzymes are elevated, it isn’t always the DMT. HCPs will look for patterns and may do additional testing.
Hepatocellular pattern (high ALT/AST): Likely the drug (DMT), fatty liver disease (common), or viral hepatitis.
Cholestatic pattern (high ALP/GGT): Likely gallstones or a bile duct issue.
The “Steroid Spike”: High-dose steroids used for relapses can cause a temporary, sharp spike in liver enzymes that resolves on its own.
The “alcohol & drug” markers
GGT is uniquely sensitive to substances that the liver has to process.
Alcohol: GGT is the primary marker for chronic alcohol consumption. It rises when someone drinks heavily and drops (slowly, over 2–6 weeks) when they stop.
Enzyme Induction: This is critical for pwMS. Many drugs do not damage the liver but cause it to “rev up” its machinery to metabolise the medication. This is called enzyme induction. This causes GGT to leak into the blood.
Common culprits of a raised GGT in pwMS are anticonvulsants (often used for MS nerve pain, like carbamazepine), antidepressants, and some muscle relaxants. If a patient on these meds has an isolated high GGT (with normal ALT/AST), it is often just a sign the liver is working hard to process the drugs, not that the liver is being damaged.
The AST/ALT Ratio is a simple calculation that can provide a surprisingly strong clue about what is damaging the liver. Because AST and ALT are stored in different parts of the liver cell, different types of damage release them in different amounts. In a healthy liver, ALT is typically higher than or equal to AST. Therefore, a normal ratio is usually < 1. If the AST is double the ALT, it is strongly suggestive of alcohol-related liver disease. Alcohol is toxic to mitochondria (the cell’s power plant), where most AST is stored. When alcohol damages these structures, large amounts of AST are released. Producing ALT requires vitamin B6. Chronic alcohol use depletes B6, meaning the liver physically cannot make enough ALT to raise the levels high, even if it is injured.
The “fatty liver signature” (ratio < 1)
If the ALT is higher than AST, it usually points to non-alcoholic fatty liver disease (NAFLD), which is a common cause of abnormal liver tests. Both AST and ALT are mildly elevated, but ALT is typically higher. This is often seen in patients with poor metabolic health, i.e. weight gain, high cholesterol, or type 2 diabetes. Reduced mobility in MS can sometimes lead to weight gain; this pattern is frequently observed during DMT monitoring.
The “danger flip” (cirrhosis)
There is one critical exception to the fatty liver rule. If a patient typically has a fatty liver pattern (ratio < 1) and over time the ratio flips to > 1 (AST becomes higher), it is a warning sign of progression to fibrosis or cirrhosis. As the liver becomes scarred (fibrotic), it produces less ALT and clears AST more slowly, leading to a reversal of the ratio. At this stage, the liver may reduce its synthesis of albumin, an important blood carrier protein, and various clotting factors. Low levels of albumin and a poor blood clotting profile are poor prognostic signs in people with chronic liver disease.
Patients with cirrhosis may develop a condition called portal hypertension when the blood from the gastrointestinal tract has difficulty passing through the liver. This often causes the spleen to enlarge and blood to pool there. When this happens, the platelet counts may drop. Low platelets in someone with cirrhosis is also an ominous sign.
The “muscle mimic”
AST is not just in the liver; it is also found in muscle. ALT is almost exclusively in the liver. In an MS patient who has severe spasticity, has had a recent fall, or has done intense physical therapy, a high AST and normal ALT is likely due to muscle injury, not liver damage. The ratio will be high (>1), mimicking the “alcohol” pattern, but the normal ALT and clinical history of muscle issues give it away. Checking CK (creatinine kinase) levels, a muscle enzyme, helps diagnose a muscle disease.
Gilbert’s syndrome
Gilbert’s Syndrome (pronounced zheel-BAYRS) is a common cause of an abnormal liver profile and is completely harmless. It is a benign genetic condition affecting roughly 3–7% of the population. It causes elevated bilirubin levels without any actual liver damage or disease. The hallmark of Gilbert’s syndrome is isolated unconjugated hyperbilirubinemia, with the other liver function tests being normal. People with Gilbert’s have a genetic mutation that leaves them with only ~30% activity of the specific enzyme responsible for conjugating bilirubin so it can be excreted in bile. People with Gilbert’s often have normal bilirubin levels most of the time, but they spike dramatically during times of physical stress. Common triggers include fasting, dehydration, infections such as flu or a cold, stress (lack of sleep or intense physical exertion) and menstruation. For a pwMS on DMTs, Gilbert’s Syndrome can be a source of confusion. However, if indirect or unconjugated bilirubin is elevated, the DMT can be continued.
I hope this explainer helps you understand your LFTs. I would be interested to know if any of you have had abnormal LFTs. What was explained to you and what was done about it? Do you find these sorts of explainers helpful, as there are many other online resources that explain LFTs in more detail than this?
Accidental readers
If you have been forwarded this email and are not an MS-Selfie subscriber, please consider subscribing and helping MS-Selfie expand its resources for the broader MS community. MS-Selfie relies on subscriptions to fund its curated MS-Selfie microsite, MS-Selfie books, MS-Selfie Infocards, and other activities that extend beyond the MS-Selfie Substack newsletters.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite and other related activities, as I don’t have time to do this myself. You must be a paying subscriber to ask questions unrelated to the newsletters or podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Questions
If you have questions unrelated to the newsletters or podcasts, please email them to ms-selfie@giovannoni.net. Prof. G will try to answer them as quickly as possible.
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have any problems, please tell your healthcare professional, who can help you.



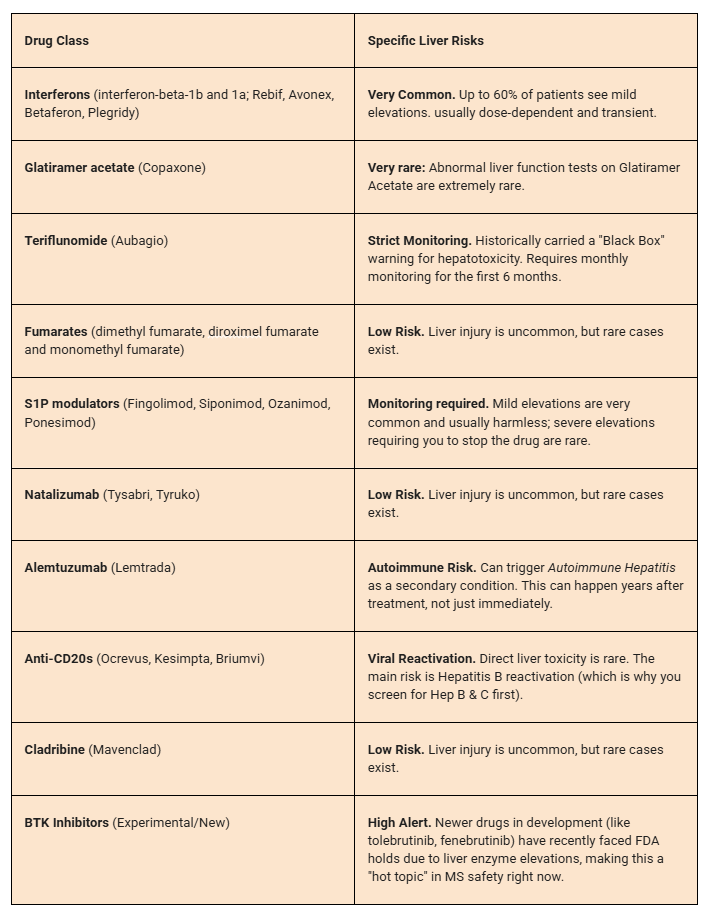
I had toxic hepatitis from Copaxone! After investigating autoimmune hepatitis, they ruled this out and concluded it was a rare reaction to Copaxone.
This is very helpful thank you.
Could you add a list of symptoms for liver injury or diseases that we can reference? I only know eyes or skin looking yellow and nausea. Can we tell anything about liver health from stool colour? Mine are often tan coloured or very light brown.
For how long after taking the last Cladribine pill do I need to be concerned about liver issues? Y2 bloods at 6 months liver function panel was all in range.