Tired of life take-2
I would be interested to know when your neurologist last asked you if you were lonely.
I was surprised, not necessarily in a pleasant way, with the attention my newsletter on diagnosing someone as being ‘tired of life’ rather than depressed (‘Tired of Life’, 10-May-2024). The range of comments is intriguing, and I urge you to read them all to understand how divisive the term ‘tired of life’ is. This particular patient denied being depressed, and when I interrogated him, although he had some vegetative features of depression, he did not have enough to make a diagnosis of depression. Most of the vegetative features of depression were likely to be due to his MS.

What are the vegetative features of depression?
Depression is a complex mental health disorder that is characterised by a range of emotional, cognitive, and often physical symptoms. Vegetative features pertain to essential bodily functions and include problems with sleep, appetite, energy levels, and psychomotor activity.
Sleep disturbances: One of the most common vegetative features of depression is sleep disturbance, which can manifest in several ways, including:
Insomnia: Difficulty falling asleep, staying asleep, or waking up too early and unable to go back to sleep.
Hypersomnia: Excessive sleeping or prolonged sleep duration, often accompanied by persistent fatigue.
Poor Sleep Quality: Even if individuals can sleep, they may experience restless or non-restorative sleep, leading to feelings of tiredness upon waking.
This patient claimed his sleep was not a problem.
Changes in appetite and weight: Depression can significantly alter an individual's eating habits, leading to changes in appetite and weight:
Decreased appetite: Many people who are depressed lose interest in food, eat less, and experience weight loss.
Increased appetite: Conversely, some individuals may experience increased appetite, particularly cravings for carbohydrates and sugars, resulting in weight gain.
Altered eating patterns: Irregular meal times and changes in food preferences are also common.
Although this patient had gained weight, he claimed it was due to inactivity and excessive calorie intake from his alcohol misuse rather than due to a problem with his mood.
Fatigue and loss of energy: Fatigue and loss of energy are almost universal in people who are depressed.
Persistent fatigue: A pervasive sense of tiredness and lack of energy that does not improve with rest is a hallmark vegetative feature of depression.
Reduced motivation: Individuals may find it challenging to engage in daily activities, even those they once enjoyed.
Difficulty concentrating: Mental fatigue often accompanies physical fatigue, leading to issues with focus, decision-making, and memory.
Psychomotor changes: Psychomotor changes refer to alterations in physical movement and activity levels, and in depression, these can include:
Psychomotor retardation: Slowed physical movements, speech, and reactions. Individuals may feel as though they are moving in slow motion. This is difficult to diagnose in a person with advanced MS who is disabled. MS-related disability is the more likely cause of his slow movements.
Psychomotor agitation: Conversely, some people who are depressed may experience restlessness, fidgeting, or an inability to sit still.
Other vegetative symptoms of depression include:
Sexual Dysfunction: Depression can lead to a decreased interest in sexual activity and issues with sexual performance.
Physical aches and pains: Somatic symptoms such as headaches, abdominal pain and chronic pain without a clear medical cause can also be vegetative features of depression. This is often referred to as somatisation, i.e. developing somatic complaints. Somatisation is also cultural. In some cultures, where depression is a taboo subject, or they don’t have a word for it, people with depression are much more likely to present with somatic complaints.
Recognising vegetative features is, therefore, crucial in the diagnosis of depression and in monitoring the response of depression to treatment. Vegetative symptoms help HCPs assess the severity of depression and can provide insight into the physical and functional impairments a depressed patient is experiencing. Effective treatment for depression often involves addressing vegetative features through a combination of counselling, medication, lifestyle changes, and other support from healthcare and social care professionals.
On balance, I didn’t think this patient was depressed. Therefore, I didn’t suggest treatment for depression, which in my practice includes counselling (CBT and mindfulness), lifestyle changes (exercise, sleep hygiene, diet, …) and potentially anti-depressant medication.
If you identify with these symptoms and feel depressed, please raise this with your HCP. Depression is a treatable condition.
Social isolation and loneliness
Some of you suggested this man was socially isolated and lonely. I suspect he was both. Although he lived with his wife, they rarely saw anyone socially except their daughter. I guess their social isolation was due to many factors, in particular, this man’s level of disability and the fact that his elderly wife was frail. When I asked him if he felt lonely, he said no.
It is important to pause here and reflect on whether social isolation and loneliness are diseases or simply risk factors for disease.
What is the difference between social isolation and loneliness?
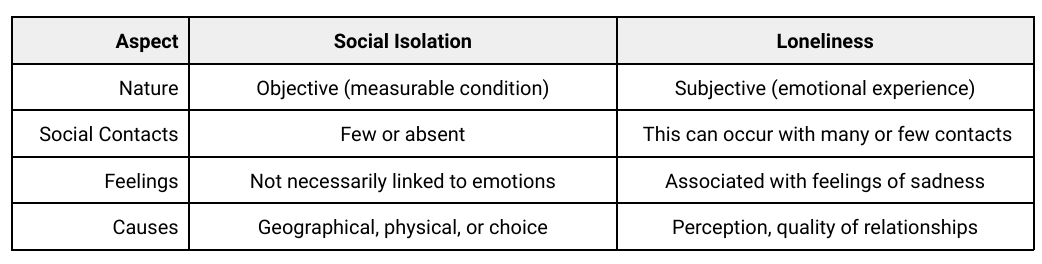
Understanding the distinctions between social isolation and loneliness is essential for addressing mental health and well-being. Although the terms are often used interchangeably, they have distinct meanings and implications.
Social isolation refers to a lack of social connections or interactions. It is a measurable, objective condition where individuals may have minimal contact with others. Factors contributing to social isolation can include living alone, geographic separation, or limited access to social activities and networks. Social isolation can be intentional, such as when someone chooses solitude, or unintentional, such as when physical or mental health issues restrict social engagement. This patient’s social isolation is probably both intentional and unintentional.
Characteristics of social isolation:
There are few to no social interactions or relationships
Physical separation from others
Limited participation in community or social groups
Measurable by the number or frequency of social contacts
On the other hand, loneliness is a subjective feeling of distress or discomfort from perceived social isolation. It involves an emotional response to the discrepancy between desired and actual social connections. Loneliness can be experienced even by those surrounded by people if they feel their relationships are not meaningful or fulfilling.
Characteristics of loneliness:
Emotional distress linked to perceived lack of companionship
Can be experienced despite being socially active
Related to subjective quality and satisfaction of relationships
Not necessarily connected to physical isolation
The primary difference lies in the objectivity of social isolation versus the subjectivity of loneliness. Social isolation can be quantified by the number of social contacts or the frequency of social participation. In contrast, loneliness is a personal, emotional experience that varies according to an individual’s perceptions and expectations of social relationships.
Differences
While social isolation and loneliness are related, they are not the same. Social isolation is an objective lack of social interactions, whereas loneliness is the subjective feeling of not having the desired level of social connection. This patient could not deny that he and his wife were socially isolated, but he was adamant that he was not lonely. Their social isolation could be tackled by increasing opportunities for social interaction, which he was reluctant to do. In comparison, loneliness would be better addressed by improving the quality and depth of existing relationships. He claimed to have a good relationship with his wife and daughter. This is why I finally settled on describing him as tired of life.
The corollary to being tired of life is wanting to live forever. Immortality is very topical amongst the ultra-wealthy. They may realise that if they only live to 100 or 120, they may not have enough time to spend their money. Many ultra-wealthy individuals invest heavily in anti-ageing initiatives, and some have started companies investigating ageing. Some are resorting to receiving blood transfusions from young donors because this has been shown to work in laboratory animals. Although I didn’t ask this patient whether or not he wanted to live forever, I would be surprised if he did. I don’t think I have ever asked a patient whether or not they want to live forever. I suspect any healthcare professional asking that question would be considered a crackpot. Do you agree?
A similar question would be, do you want to work forever? I, for one, don’t want to work forever. Firstly, I would be consuming resources that are better deployed to a younger, more energetic, and more productive person. Secondly, I also have many interests outside of work that I want to pursue that need deep time to be done properly. Thirdly, my wife wants to travel whilst we are still relatively healthy and mobile. Maybe it is time for me to make early retirement plans. What do you think?
Two articles I read yesterday prompted me to write this newsletter. The first was in the New England Journal of Medicine (Fernandez &, Chin. Keep Your Eyes on the Prize—Focusing on Health Care Equity. N Engl J Med. 2024 May 16;390(19):1733-1736). The authors believe that healthcare–centric goals, i.e. equity in patient experience and clinical outcomes, should be the primary aim of clinicians, healthcare administrators, and payers. Addressing unmet individual health-related social needs, i.e. the social determinants of health, should not be our remit. Do you agree? I have suggested that we routinely screen for modifiable social determinants of health in clinical practice and, if possible, signpost patients to the relevant social services. For example, if patients have problems with food security, they can be referred to their local food bank. If lonely, refer them for a social prescribing assessment. What do you think?
The second article was about loneliness (Servick K. Striving to connect. Science. 2024 Apr 26;384(6694):375-379.). The article addressed loneliness at a population level and why it is essential to identify and treat loneliness. It reviews the evidence linking loneliness to poor health outcomes and discusses emerging evidence on managing and treating loneliness. The issues raised in this article are very relevant to the management of MS. A survey done by the UK MS Society several years ago revealed that 3 in 5 people with MS report being lonely. This figure is worrying and is one of the reasons I include loneliness in my holistic management of MS. I suspect that pwMS who listen to and read MS-Selfie are likely to be more motivated than pwMS who don’t and hence less socially isolated and less lonely. Or maybe I am wrong. I would be interested to know when your HCP last asked you if you were lonely.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
X (Twitter) / LinkedIn / Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.




I didn't plan to comment on this topic, but you have come back to it and I applaud you for that. When I had a bad attack that put me in hospital for 5 and a half weeks, a number of things came to a head. Firstly, my working days were over so I was no longer the bread winner. Secondly, because of the first factor my wife left and demanded half our assets. I applied to trigger the insurance policies that had been in place for decades so, naturally, the insurance company wanted to deny my payout. In fact they accused me of lying about having MS for over 20 years and said the policy was thus void. When that was solved, the superannuation fund that held my policy tried to slash it's value by 60% on the basis that they had made a mistake calculating its worth over a decade earlier and, of course, it wasn't their fault and I should have known. In the end, I took them to the second highest court in Australia and the problem was solved. All this happened while I could barely think straight, my employer turned feral, my wife had walked out and I was trying to learn how to walk again.
As part of my health insurance (different from the other stuff) I was offered psychological counseling. I took it as I felt it would help support my legal cases, not because I believed it would benefit my soul. Throughout the rehab and the psychological process I felt like I was living in an asylum where the lunatics were in charge. No one was interested in how hard I was trying to recover, they just expected me to do things that had to be retaught. Every few days, I sat opposite the woman who kept yabbering on about 'mindfulness' and wondered how I could shut her up.
One day, the 2IC of the rehab place said "I just can't keep writing letters to your employer, you'll have to go back". I knew that meant rising at 5:15 each morning to be in the office at 7am and dealing with highly complex transactions that were now beyond me. I could barely stand at that stage.
The psychologist was my next appointment and she said something that reinforced her lack of understanding. My response was very dark and I won't repeat it. Suddenly she was very alert and it seemed the penny had dropped. In her answer she said "we want you to be safe".
That was something that no one had ever said to me. And she had articulated the key issue- I wanted to be safe and I was tired of doing it all on my own. Of course, I still do it all on my own but now I knew what I was missing. It wasn't companionship, or financial security, or a recovery, or anything else. I now knew that I wanted to be safe.
Too often, medical people and our social contacts send the message "Off you go". But go where, do what? MS brings with it a heightened sense of abandonment. There is no shared journey.
Ask that man if he feels safe enough to put down what he is carrying. If he tells you yes, he is probably lying. If he goes quiet and reflects on it, then you may have made a start.
When I was diagnosed, I started reading articles and became a member of several FB groups. As well as understanding that the disease is incurable, I was also struck by the isolation and loneliness of many pwMS with some level of disability. Nobody likes the sick in general. People don't want to take the time to listen to you when you're talking slowly, or go for a walk with all the logistics of a wheelchair. When you're not yet severely disabled, you live a "nuclear" life between work and home and don't really need a wider circle of contacts. And when disability makes us vulnerable, we no longer have the strength and opportunities to create social links. That's why I've taken a critical decision. I'm going to leave full-time work. The time that will be freed up, I'm going to invest in becoming a member of various associations, I haven't yet decided which ones:). For me it's an investment in the future and an attempt to prevent social isolation, which I've indeed identified as a major problem I may face.