The Lazarus effect in MS
When someone transitions from almost being confined to a wheelchair to being able to walk and run, we call this the Lazarus effect.
I always ask the question, ‘How many swallows does it take to make a summer?’. Sometimes one is enough. I may have just seen what an MS cure promises to be.
I just returned from the annual European Charcot Foundation (ECF) meeting in Italy. This is a small yearly meeting that is predominantly focused on teaching rather than original research. I started the meeting off with a debate. I took the position that MS is progressive in all people with MS. I made the argument that the real MS was smouldering MS and explained that those who had RIS (radiologically isolated syndrome) who did not go on to develop MS were able to cure themselves of having MS. In other words, smouldering MS only happens in people who can’t spontaneously cure themselves of what is causing their disease. I reiterated the point that relapses and focal MRI were simply the immune system’s response to what is causing the disease. I presented my theory that the clinical phenotypes we observe are merely an immunological phenotype, using leprosy as an analogy. Several people didn’t like the leprosy analogy to explain what we see happening in MS.
I also spoke at a sponsored symposium on the past, present and future of MS care, making the point that MS prevention could become a reality and that for people who had MS, we could offer a cure in the future. I based the latter on the EBV driver hypothesis, i.e MS disease activity is being driven by EBV latent-lytic cycling. On the penultimate day, I discussed emerging antiviral strategies targeting EBV for the treatment of MS. I covered the data supporting how I believe AHSCT and alemtuzumab, our most effective DMTs, are working as immunotherapies targeting EBV, specifically as T-cell rejuvenation therapies in combination with EBV autovaccination. For more information on how I think AHSCT and alemtuzumab work, please see: “AHSCT with ATG vs AHSCT with rituximab vs alemtuzumab” (14-Feb-2025).
I spent some time discussing CAR T-cell therapies, emphasising the need to have CNS penetration. When defining a cure for MS, I hypothesised that we would likely have to clear the CNS of pathogenic plasma cells responsible for producing intrathecal (within the meninges) oligoclonal IgG bands, or OCBs. This is why CD19-targeted CAR T-cell therapy may not be sufficient to cure MS. Plasma cells don’t express CD19 and, therefore, will escape deletion with anti-CD19-targeted therapies. A solution to this would be to focus on targeting B-cell maturation antigen (BCMA), which is expressed on plasma cells. This is when a swallow flew into the lecture hall, and instead of it being winter, the lecture theatre was full of sunshine.
Professor Barbara Willekens from Antwerp showed us a video of a young man with advanced progressive MS who had been treated in a first-in-human study of anti-BCMA CAR-T Cell therapy in China. He had an EDSS of 6.5 (two sticks) to 7.0 (wheelchair) as he had started using a wheelchair for outdoor mobility. He underwent CAR T-cell therapy in January 2025, and by October 2025, he was able to run, albeit with some residual spasticity in his lower legs. I estimated, looking at the video, that his EDSS must now be around 3.5-4.0. The audience was so impressed that after the video, the audience spontaneously started clapping, and I must admit I had a tear in my eye.
When someone transitions from almost being confined to a wheelchair to being able to walk and run, we call this the Lazarus effect. The effect is named after the biblical figure Lazarus, who was raised from the dead. In reality, this effect refers to the spontaneous return of signs of life, such as a pulse, after the cessation of cardiopulmonary resuscitation. Also known as autoresuscitation, this occurs within minutes of resuscitation efforts being stopped, with the patient appearing to have “come back to life” after being pronounced dead.
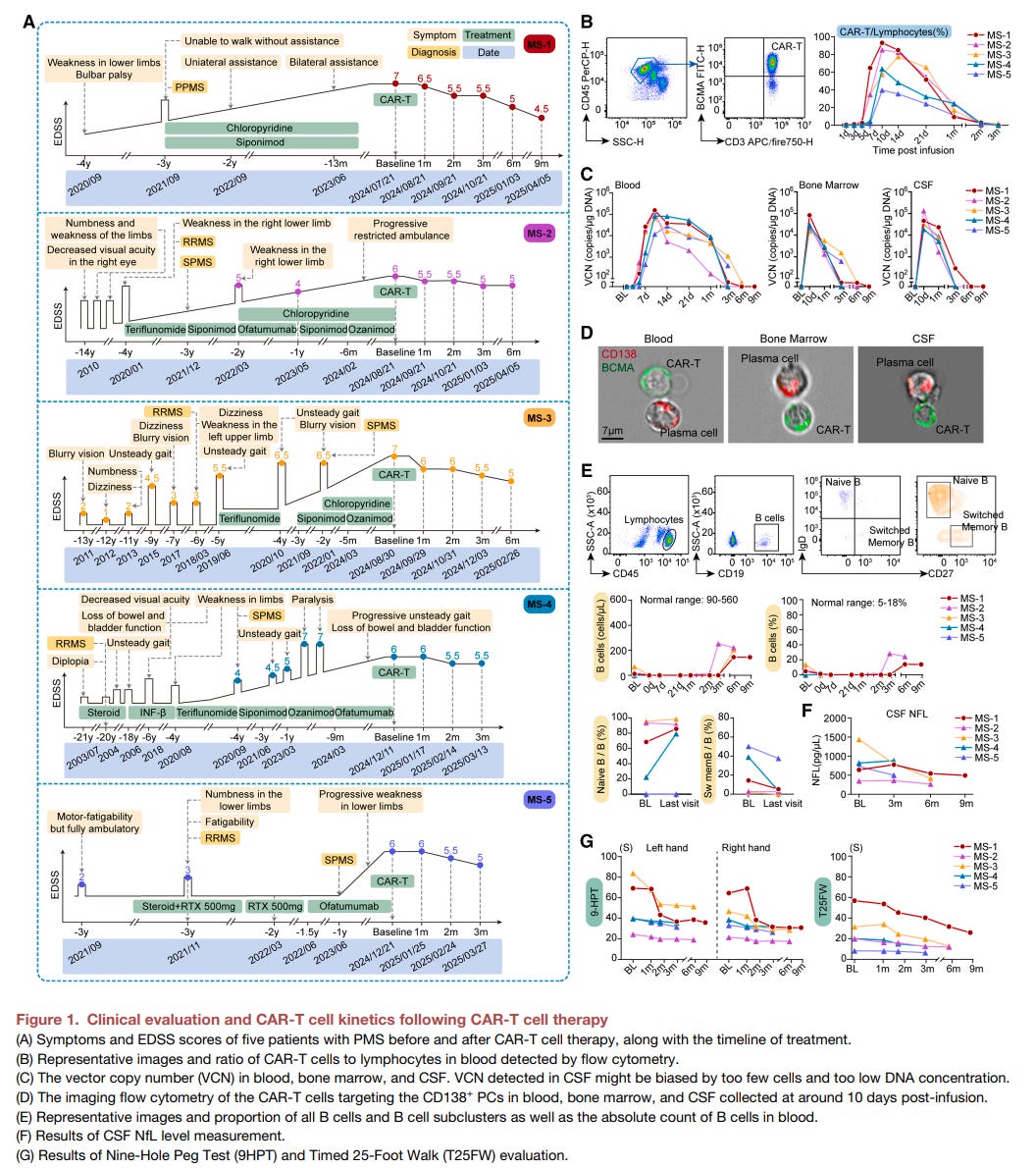
I sincerely hope this one swallow is not the end of this story. I don’t think so. This patient is one of five patients in the small case series below. This study reports the results of the first-in-human study of anti-B-cell maturation antigen (BCMA) chimeric antigen receptor T (CAR-T) cell therapy in patients with progressive MS (PMS).
The study investigated the safety and efficacy of this CAR-T cell treatment, which is designed to target CNS resident plasma cells, a subset of B cells implicated in central nervous system (CNS) inflammation in PMS. The study found a favourable safety profile, significant depletion of plasma cells in the CNS, and the alleviation of microglial activation in the CNS, suggesting CAR-T therapy holds potential for managing this severe form of MS. The investigators also present detailed single-cell multi-omics analyses to explain the dynamics and mechanism of the CAR-T cells within the patients’ blood, bone marrow, and cerebrospinal fluid.
The study doesn’t overhype the treatment effect, as it was open-label; however, the results are remarkable when considering the EDSS, 9-hole peg test, and timed 25-foot walk results. All patients improved to a greater or lesser extent. I suspect that the patient we saw in the video progressed from an EDSS of 7.0 to 4.5 over 9 months. Let’s hope these results hold up when further randomised trials are completed.
This strategy for treating MS supports my hypothesis that we need to purge the body of EBV-infected B-cells, including those resident in the CNS, and simultaneously remove pathogenic plasma cells from the CNS. The CSF data from these patients show that the kappa free light chains plummet in the CSF, which is a biomarker of antibody production within the CNS. We are using the latter in our SIZOMUS study to investigate the impact of a second-generation proteasome inhibitor (ixazomib) on CNS-resident plasma cells. This CAR T-cell trial gives me confidence that we are on the right track.
I would appreciate your thoughts on these results. Am I overhyping them? Do we need more than 5 swallows to make a summer?
This study also demonstrates how rapidly Chinese scientists are catching up with us in North America and Europe. When it comes to testing these innovative strategies in MS, they are ahead of the game.
Progressive multiple sclerosis (PMS), which is characterized by relentless disease progression, lacks effective treatment. While recent studies have highlighted the importance of B cells in driving compartmentalized central nervous system (CNS) inflammation in PMS pathogenesis, current B cell depletion therapies, such as CD20 monoclonal antibodies, face challenges in targeting plasma cells within the CNS. Here, we treated five patients with PMS (one primary PMS and four secondary PMS) with anti-B cell maturation antigen (BCMA) chimeric antigen receptor T (CAR-T) cell therapy in an ongoing phase 1 clinical trial (ClinicalTrials.gov: NCT04561557). Only grade 1 cytokine release syndrome was observed, and all grade ≥3 cytopenias occurred within 40 days post-infusion in all five patients. Meanwhile, we detected plasma cell depletion in CNS compartments, prolonged expansion and relieved exhaustion of CAR-T cells in the cerebrospinal fluid, and attenuation of microglial activation. These findings provided insights into the potential application of anti-BCMA CAR-T therapy for advancing clinical management of PMS.
Accidental readers
If you have been forwarded this email and are not an MS-Selfie subscriber, please consider subscribing and helping MS-Selfie expand its resources for the broader MS community. MS-Selfie relies on subscriptions to fund its curated MS-Selfie microsite, MS-Selfie books, MS-Selfie Infocards, and other activities that extend beyond the MS-Selfie Substack newsletters.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite and other related activities, as I don’t have time to do this myself. You must be a paying subscriber to ask questions unrelated to the newsletters or podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Questions
If you have questions unrelated to the newsletters or podcasts, please email them to ms-selfie@giovannoni.net. Prof. G will try to answer them as quickly as possible.
Important Links
🖋 Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you experience any problems, please consult your healthcare professional, who will be able to assist you.




This seems extraordinarily promising. Being able to reverse disability in people with high EDSS gives hope.
I would consider age too. I’m sure when I was younger and not treated, ( unaware I had MS) some symptoms repaired. Mainly my arm function. As we age is it not harder to self repair with or without meds. I think it’s crucial to treat as soon as diagnosis is made. With the most effective medicine. Not the cheapest. As in the long run it’s not the cheapest for the person or society.