Opportunistic infection in MS
Cytomegalovirus or CMV infection occurs in people with MS on intense immunosuppression. This is a reminder of the risks associated with some DMTs and is a reminder to pwMS to be vigilant.
Apologies in yesterday’s MS-Selfie Newsletter on lymphopaenia I inadvertently left out the fumarates. I have now updated the newsletter online to include information on this class of DMTs.
Opportunistic infection of interest
Today I cover a topic that is only really relevant to pwMS who are about to be treated with alemtuzumab or HSCT and have more intense short-term immunosuppression and are at risk of getting cytomegalovirus (CMV) infection or reactivation.
In people treated with alemtuzumab about 0.13% get CMV reactivation due to the intense short-term immunosuppression. With HSCT the incidence in CMV-positive cases can be as high as 50% depending on the intensity of the ablative protocol. However, bone marrow transplant units often use prophylactic antivirals to prevent this from occurring.
CMV reactivation typically occurs with quite marked immunosuppression that hits both innate (neutrophils and monocytes) and adaptive (T-cells) immunity. I have only had one patient at our centre with this complication and this patient did not have MS, but a condition called CNS vasculitis. He presented with pyrexia and pneumonia, about a week after having alemtuzumab treatment. He responded rapidly to ganciclovir treatment and made a full recovery.
A case of CMV meningitis has been reported in a pwMS on dimethyl fumarate, which is another indication that DMF really does hit CD8+ cytotoxic T-cell function, which is the main immune cell that keeps CMV at bay. Similarly, CMV gastritis, a localised form of CMV infection, has also been described with natalizumab that presumably reduced CD8+ T-cell trafficking in the stomach. What these rare opportunistic infections are telling us about DMTs is that we need to be aware of rare opportunistic infections and take any symptoms suggestive of infection very seriously.
What these rare case reports of opportunistic infections are telling us is that there are always undefined risks associated with immunosuppression, which have to be weighed up against the impact of not treating or undertreating MS.
Interestingly, at a population level, there is evidence that being infected with CMV may lower one’s risk of developing MS in the future. We don’t know why, but it may act as a counterbalance to EBV infection, which increases your risk of getting MS.
The following is some more details about CMV and the types of infections it can cause in pwMS who have been treated with alemtuzumab or HSCT.
Cytomegalovirus
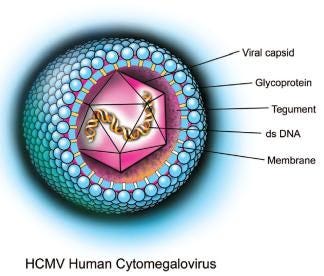
CMV is a member of the herpes virus family. CMV infection is typically asymptomatic in healthy people but can be life-threatening in immunocompromised people. After infection, CMV remains latent within the body throughout life and like other herpes viruses can be reactivated at any time. CMV is strongly associated with mucoepidermoid carcinoma and possibly other malignancies. CMV is found throughout the world and all socioeconomic groups and infects between 60% and 70% of adults in developed countries and almost 100% in emerging countries.
As with all herpes viruses CMV has genes dedicated to altering and/or evading innate (hard-wired) and adaptive (memory) immunity. The immune system has a lifelong battle with CMV and as we get older a large number of your peripheral T-cells, or T-cell repertoire, becomes dedicated to keeping CMV in check. CMV is the virus most frequently transmitted to the developing foetus and can cause congenital CMV infection, which is one of the leading causes of deafness, learning disabilities, and intellectual disability in children.
Clinical features of CMV reactivation
CMV infection post-alemtuzumab is usually due to reactivation of the latent virus and not a new infection. Reactivated CMV infection can affect different parts of the body:
Retina: CMV retinitis affects the eyes and can cause blindness.
Lungs: CMV pneumonia caused by CMV can be life-threatening.
Gastrointestinal tract: CMV can affect any part of the gastrointestinal tract, including the oesophagus, stomach, liver, gallbladder, pancreas and colon, causing ulcers, liver inflammation, intestinal obstruction and colitis. Symptoms can include painful and difficult swallowing, nausea, vomiting, abdominal pain, yellow skin (jaundice) and watery or bloody diarrhoea.
Brain: CMV can infect the brain and other parts of the nervous system, causing symptoms like headache, confusion, and leg weakness.
The diagnosis of CMV usually requires detailed physical and targeted tests depending on which part of the body is infected. Typically the virus is detected in the blood, urine and/or stools. Occasionally, a biopsy of the affected organ, such as the lung or colon, is needed to confirm the diagnosis. Retinal involvement is usually typical and most ophthalmologists suggest the diagnosis based on the retinal examination.
Treatment: CMV reactivation is usually treated with antiviral agents including ganciclovir, valganciclovir, cidofovir and foscarnet. Ganciclovir can be given intravenously, orally or as a pellet implanted in the eye to treat an infection in the retina. Valganciclovir has better oral absorption than ganciclovir but the two medications are otherwise very similar. Cidofovir is approved for the treatment of CMV retinitis. Foscarnet must be given intravenously and is usually reserved for those who have a virus that is resistant to ganciclovir or those who have serious side effects from ganciclovir. Side effects of ganciclovir and valganciclovir include the suppression of white blood cells, red blood cells and platelets. Because cidofovir and foscarnet can cause renal toxicity, kidney function needs to be monitored carefully.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.