It was the worst pain I have ever had
Trigeminal neuralgia, brief, very painful, electric shock-like episodes in the distribution of the trigeminal nerve is common in people with MS. This newsletter describes its management.
Pain syndromes are common in people with MS. The ones that seem to be the most disabling are the neuralgic syndromes in particular trigeminal neuralgia (TN).

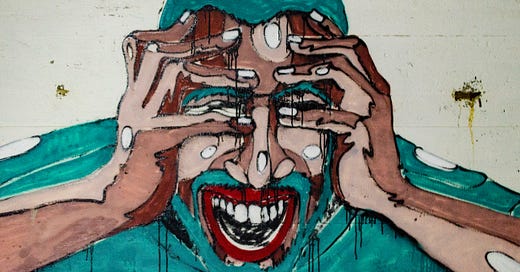
TN is recurrent, brief (seconds to minutes), very painful, electric shock-like episodes in the distribution of the trigeminal nerve (see picture below). Typically the pain is unilateral, but can rarely be bilateral. TN is very debilitating and impacts pwMS’ ability to function. The pain can be so severe that it makes smiling, talking, eating, drinking, brushing one’s teeth, shaving and even touching your face difficult, thereby resulting in a poor quality of life. People with TN are more likely to be anxious and depressed and the pain can be so severe that some people consider suicide.
TN in pwMS is usually due to a lesion where the trigeminal nerve leaves the brainstem; this area is called the root entry zone. In people with classic TN, the most common finding is neurovascular compression, where a blood vessel presses on the nerve in the posterior fossa. Recent studies suggest that about 50% of pwMS have neurovascular compression, which implies that the TN is unrelated to their MS or MS lowers the threshold for developing TN. Finding evidence of neurovascular compression is important because it means some pwMS with TN resistant to medical treatment may respond to surgical intervention.
It is estimated that approximately 1 in 50 pwMS will develop TN in the course of their disease course. So TN is much commoner than you realise. I suspect some of you may have already had TN. I would be interested to know if it was diagnosed as TN or something else.
I have seen TN occur as part of a relapse, i.e. with a new lesion in the brainstem that has enhanced after the administration of gadolinium on MRI. In the case of TN from an acute relapse, it may respond to a course of high-dose steroids.
When someone with MS develops pain suggestive of TN it is important to exclude other causes and not assume it is MS-related for example temporomandibular joint problems, migraine or other headache syndromes with facial pain, sinusitis, tooth abscess, etc. TN most frequently affects the distribution of the maxillary (V2) and mandibular (V3) divisions of the trigeminal nerve, although involvement of the ophthalmic (V1) division can occur.
The frequency and duration of TN attacks are variable. The pain typically lasts from less than a second up to 2 min in the majority of affected pwMS. However, a minority report attacks lasting longer. Many pwMS can have clusters of attacks that last hours to days. Some pwMS describe several hundred attacks daily, but most pwMS have less than 10 attacks daily. TN often has a relapsing-remitting pattern with no pain between clusters. However, a third of people with TN have chronic low-grade background pain, which may require an additional add-on treatment.
A feature of TN is that attacks can be triggered by seemingly innocuous mechanical stimulation of the face and mouth on the side of the pain, e.g. light touch, talking, chewing, brushing teeth, washing or drying, drinking and shaving.
The neurological examination can be normal but about a half of pwMS will have reduced light touch on the side of the face where the pain occurs.
The pain is probably triggered by the inappropriate firing of demyelinated nerves, which the brain then perceives as a painful stimulus. This is supported by the observation that TN usually responds to a group of drugs called sodium channel blockers. Sodium channels are responsible for conducting electrical currents along nerve fibres and by blocking them you prevent this abnormal firing.
All patients with MS and TN should have an MRI of the brain to see if an MS lesion can be seen in the brainstem and to exclude other causes of TN, in particular, neurovascular compression.
In my experience carbamazepine and oxcarbazepine, which are both sodium-channel blockers, are the most effective therapies for TN, with about 80% of patients responding quite rapidly to these drugs. As with all sodium channel blockers, about 40% of subjects can’t tolerate them at the effective dose. The commonest side effect is excessive sedation. Carbamazepine has many drug interactions, which can be problematic, particularly the oral contraceptive pill (OCP). Carbamazepine induces liver enzymes that metabolise the OCP rendering it ineffective.
Oxcarbazepine has fewer side effects and fewer drug interactions than carbamazepine, which is why I favour its use in TNR. In addition to sedation and drug interactions, some pwMS will develop allergic skin reactions to carbamazepine and oxcarbazepine and a small number of people will develop a low sodium level (hyponatraemia) and abnormal liver function tests. Rarely, a severe allergic skin reaction called Stevens-Johnson syndrome and toxic epidermal necrolysis can occur. This is linked to a particular genetic make-up that can be screened for before starting these treatments. The latter is much more common in Asians, in particular the Han Chinese.
Other sodium channel blockers that can be tried include lamotrigine, phenytoin and eslicarbazepine. Some patients respond to the gabapentinoids (gabapentin and pregabalin). Other agents that may help include baclofen, botulinum toxin, tizanidine, levetiracetam and misoprostol. The latter is a so-called prostaglandin analogue and I have had one patient who had such a good response to misoprostol that I promised myself to try using it earlier in patients who don’t respond to carbamazepine and oxcarbazepine. Many neurologists are reluctant you use opioids to manage pain, but they can occasionally be helpful during a crisis. I have one patient who has such bad TN that he was barely able to eat or drink until I started him on fentanyl patches.
In resistant cases surgical treatments may be required, which include microvascular decompression, controlled lesioning of the trigeminal ganglion or root by balloon compression, thermocoagulation or chemically using glycerol. Non-invasive ablation can now be done using so-called stereotactic radiosurgery with a gamma knife. All these procedures can leave the face numb, which some people find uncomfortable. Please note that the surgical management of TN is highly specialised and if it is required you are better off being referred to a specialist TN unit.
If any of you have had TN please let us know about your experiences and what worked for you.
Subscriptions
I am encouraging readers to subscribe to the MS-Selfie Newsletter. The subscriptions will give you access to the case studies and the full archive. Please note all other newsletters, such as this one, are free. The money from subscriptions will be used to employ somebody to administer, transfer and curate the contents of the Newsletter onto a companion MS-Selfie microsite. The objective is to create an MS self-help guide.
The MS-Selfie case study from the 7th of October is about a patient with rapidly evolving severe MS who was denied the option of an IRT by her neurologist because he thought it was too risky. This case study raises many issues about who is responsible for deciding what treatment strategy to adopt and who takes the risk; the HCP or the patient? You tell me!
Please note if you have MS and can’t afford the subscription please drop me an email and I can arrange a complimentary one.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.




My Trigeminal Neuralgia was the second MS relapse I suffered in 1987. (The first was sensory deprivation in my hand in 1986). There was an extremely sharp pain in my right cheek, and my speech became slurred.
Tegretol calmed both symptoms down very effectively within minutes of taking it. After 3 months I was able to wean off the medication completely.
34 years later I still haven't had a recurrence, and hope I never will.
AndrewC.
I am suffering from TN as you write. On 150mgs twice a day of pregabalin. MS nurse and Gp say they will review next week.