Is the neurological examination obsolete?
I recently saw a new neurologist when I relapsed. He did a cursory examination that took two or three minutes and told me my EDSS was 4.5. Is it possible to do an EDSS in three minutes?
Case study
Dear Professor Giovannoni, I recently saw a new neurologist when I relapsed. He did a cursory examination that took two or three minutes and told me my EDSS was 4.5. Is it possible to do an EDSS in three minutes?
Prof G’s Opinion
No, it is not possible to do an EDSS in three minutes. It takes me anywhere from 15-30 minutes to do one properly; the range depends on the level of disability the patient has and the time it takes to walk 500 m.
How many times have you had a neurological examination by your neurologist? How thorough was it? Did you know that to have an accurate EDSS (expanded neurological status score) done, you must have an extensive neurological examination and an observed walk over at least 500m?
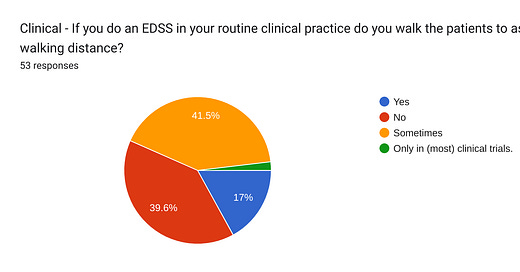
When I surveyed EDSS practice several years ago, it was clear that many neurologists were documenting EDSS scores without doing detailed neurological examinations or actively observing their patients walking 500m. This indicates that many routine EDSS scores outside clinical trials are inaccurate.
A more fundamental question is how reliable is the neurological examination. During the COVID-19 pandemic, two ECTRIMS fellows and I designed an online virtual neurological examination (VirtuEx). This is a three-part examination using a smartphone video call.
We then wanted to compare the virtual examination with the face-to-face neurological examination to see how good it was. What we discovered is that the neurological examination has never itself been validated. What do I mean by this? In short, we have no idea how good it is at picking up neurological disease, its sensitivity, or excluding disease, its specificity. We also have no idea how variable it is, i.e., intra-rater or inter-rater variability.
For example, if someone has a normal neurological examination, can you say they do not have a neurological disease? Clearly not. Many people with early MS recover from their early relapses and have no neurological signs, i.e. they score zero or 0.0 on the EDSS. However, when performing neurological stress tests on these subjects, you often find deficits that the neurological examination misses. In particular, subtle cognitive, balance, fine coordination and motor problems.
On the other side of the coin, I have been referred patients with early MS or a radiologically isolated syndrome with no localising signs or a normal neurological examination. However, when I examine these patients, I find deficits. Sometimes, the patients are aware of these deficits, which the examing neurologist missed. So, how ‘normal’ or ‘abnormal’ a neurological examination is depends on the operator.
The neurological examination, which takes years to learn and perfect, is the one physical skill neurologists and neurosurgeons have that separates us from other specialities, apart from maybe old-school general physicians. However, my recent experiences tell me that the neurological examination is more of a ritual than a science. I suspect within the next 5-10 years, a tech company will develop a battery of tests, which could potentially be self-administered, using a smartphone application or another technology that will outperform neurologists at detecting neurological deficits. Already, several standalone tests pick up subtle deficits that traditional neurological examinations will miss. I am not saddened or frightened by this. Anything that improves on what I can do physically has to be better for patients.
Link the automated quantitative neurological examination to investigations, for example, MRI brain imaging, blood tests, CSF results, electrophysiological tests, etc. and feed this into an AI algorithm with deep learning, and you can see a future where neurologists will be outperformed as diagnosticians. This is not so far away.
I was lecturing the year four medical student the other day and asked how many of them had stethoscopes, and all put their hands up; yes, 100%. When I asked who had a patella hammer, tuning forks and an ophthalmoscope, the tools of my trade, less than 5% of the class put up their hands. This is quite amazing as the stethoscope is almost obsolete and is being rapidly replaced by handheld ultrasound devices. I know at least one US medical school that has already mandated their medical student use a smartphone-enabled portable ultrasound device and have stopped teaching auscultation using a stethoscope.
In the NHS, each person with MS, or at least those on a disease-modifying therapy, should have a detailed neurological examination once a year so an EDSS score can be documented. This mandate is one of the reasons why I helped design and validate an online web-EDSS calculator. This is a good surrogate of the neurologist-measured EDSS and at least allows people with MS to get an estimate of their EDSS. It is not about me being lazy, but my consultation time is best used to talk to my patients and address their symptomatic problems. Do you agree?
The main reason I still do detailed neurological examinations in people with MS is (1) to look for dissemination in space during the diagnostic consultation, (2) to use this information as part of the prognostic profile, (3) when doing an EDSS in a clinical trial and (4) when doing a relapse assessment. However, I do short, targeted neurological assessments to decide on treatments, such as postural righting reflexes as part of the risk-of-falls assessment, spasticity when considering starting an antispastic agent, etc. I often do general examinations when looking for complications associated with MS, e.g. the mouth for poor oral hygiene, the feet for poor foot hygiene, the buttocks for pressure sores, etc. So, examining patients is still necessary, but it needs to be done for a reason; i.e. if the findings are not going to change your management, why waste time doing it?
Our online web-EDSS tool is now widely used by both pwMS and HCPs. Is this a success? No. The fundamental problem is that using the EDSS continues to entrench it as the gold standard for measuring disability in pwMS. This is a problem as almost all of us in the field know that the EDSS is not fit for purpose. Firstly, it is not a disability scale; at the lower end, it measures impairments (0.0-3.0). From 3.5 to 7.0, the EDSS is a walking scale. The EDSS is also non-linear (EDSS 4.0 is not twice as bad as EDSS 2.0), and it has ceiling and floor effects. Floor effects mean that at the lower end, the EDSS is missing a lot of hidden disabilities, and the same happens at the other end of the scale. For example, you stay at EDSS 6.5 (bilateral support to walk 10 metres) for many years despite your disease worsening in other domains. The EDSS also has high intra and inter-rate variability and is subject to fatigue-related changes. The EDSS changes depending on what time of day you do the assessment. So why are we still using the EDSS? It is a good question and is largely driven by regulators. The regulators are used to seeing the EDSS as an outcome measure in clinical trials, which is unlikely to change soon. Whenever you suggest to the FDA or EMA that we want to use a different primary outcome measure, they always come back to the EDSS. They want it as part of a composite or a standalone primary outcome measure.
This state of affairs is very sad as the EDSS as an outcome measure is holding the field back, particularly in doing trials on smouldering MS. The EDSS is too insensitive to change, i.e. too few patients have events (confirmed disability worsening) on existing DMTs to do reasonably sized studies.
I have said enough. I would be interested to know if your neurologist does an annual detailed neurological examination and whether or not he/she walks you 500 m before documenting your EDDS score. I would also be interested in your thoughts on the automated neurological examination. Would you be up for it?
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. If people want to ask questions unrelated to the Newsletters or Podcasts, you need to be a paying subscriber. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your own healthcare professional, who will be able to help you.





I have NEVER had my walking observed by any neurologist in the past 30 years. They do a finger/nose test, observe me looking from left to right, test my hand strength & plantar reaction. I can't walk more than 800m. I tell them that. They pluck an EDSS out of the air. Some years it's 2.6 or 3, others it's 4.5. Depending on who I see. They never ask about bladder and bowel function. I think you are the Carlsberg of neurologists. If only every neurologist were as good!!!
My neurologist bases his EDSS score from my annual mri. I have remained at 3 since DX 10 years ago, despite having new symptoms. But convinced no new lesions means I can’t be worse.