Is it MS or is it the menopause?
Dealing with menopause is hard enough without having MS. In this Newsletter Prof G goes through the pros and cons of HRT (hormone replacement therapy) for managing menopause in women with MS.
Case Study
“I am a woman with MS and I am perimenopausal. My last menstrual period was three months ago and I have frequent hot flushes. All of a sudden my MS seems to have worsened. I am more fatigued, my sleep is disrupted, my bladder problems are worse, my mood is all over the place and my walking has deteriorated. Is this my MS or is it simply my menopause? “
In my experience, menopause seems to change things for women with MS (wwMS). There is little doubt that in healthy women the menopause is associated with a well-defined syndrome or constellation of symptoms and physical signs. Some women cope very well with menopause and others don’t. There are several symptomatic treatments that can be prescribed to deal with specific menopausal symptoms or you can take hormone replacement therapy (HRT), which really delays menopause as it replaces the hormones your ovaries make as they fail.

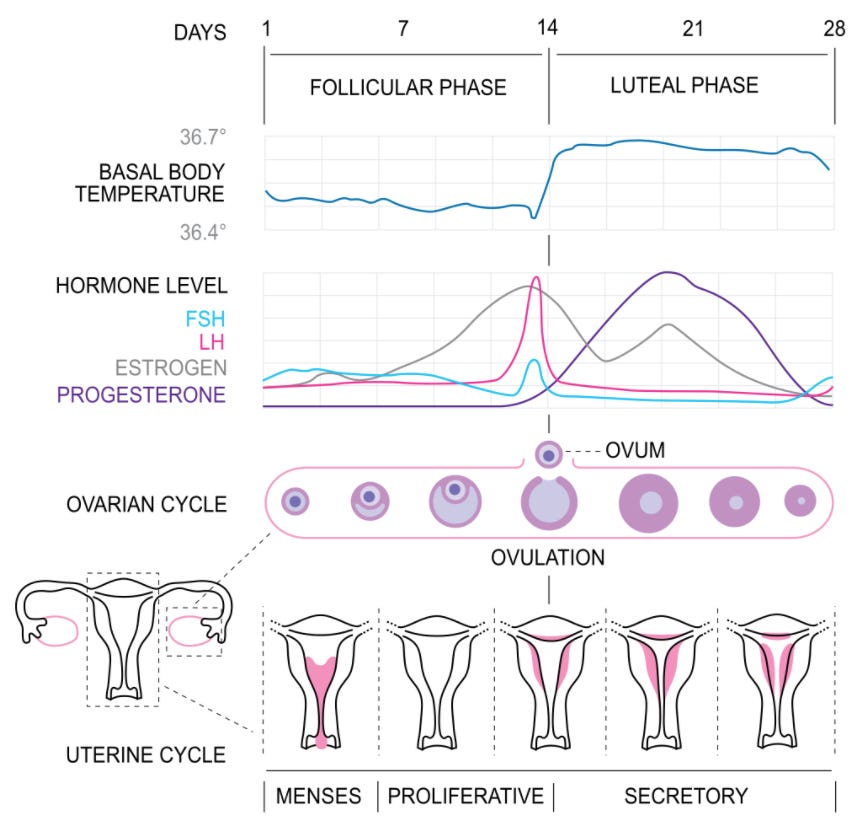
The menstrual cycle
The menstrual cycle is characterised by a well-defined series of hormone production, which change the structure and function of the uterus and ovaries of the female reproductive system to make pregnancy possible. The ovarian cycle controls the production and release of eggs and the cyclic release of oestrogen and progesterone. In comparison, the uterine cycle prepares and maintains the lining of the uterus to receive a fertilised egg.
The ovarian and uterine cycles are highly coordinated and typically last about 28 days and continue for about 30–45 years. A woman is born with a finite number of oocytes or eggs, which defines the number of ovulatory cycles she can have in a lifetime.
Hormone replacement therapy or HRT
There has been a relatively recent backlash against HRT by the medical community when HRT was shown to increase your chances of developing breast cancer and your chances of having a heart attack or stroke by 10-20%. However, these risks need to be put in the context of the benefits of HRT and the fact that both breast cancer and cardiovascular risks can be derisked with appropriate screening.
“... for women of average weight in developed countries, 5 years of HRT, starting at age 50 years, would increase breast cancer incidence at ages 50–69 years by about one in every 50 users of oestrogen plus daily progestagen preparations; one in every 70 users of oestrogen plus intermittent progestagen preparations; and one in every 200 users of oestrogen-only preparations. The corresponding excesses from 10 years of HRT would be about twice as great.” (Collaborative Group on Hormonal Factors in Breast Cancer. Lancet. 2019 Sep 28;394(10204):1159-1168.)
“A large meta-analysis comparing HRT with placebo showed that the use of HRT was associated with an additional six strokes per 10,000 women, 8 cases of venous thromboembolism (VTE) per 10,000 women and four cases of pulmonary embolism (PE) per 10,000 women.” (Boardman et al. Cochrane Database Syst Rev. 2015 Mar 10;(3):CD002229.)
It was therefore very reassuring when another very large and definitive meta-analysis showed that the all-cause mortality was not increased by HRT (Manson et al. JAMA. 2017 Sep 12;318(10):927-938.).
In other words, the benefits and risks of HRT in terms of life expectancy or survival balance each other off. Based on this I think HRT is safe provided you participate in your national breast cancer and cardiovascular screening programmes. By doing this women who are at high risk of these complications can be discouraged from taking HRT and women who are at low risk can at least have the option of receiving the benefits of HRT.
It is important to realise that the type of breast cancer that occur as a result of HRT is usually hormone-responsive and hence have a better prognosis. In terms of the cardiovascular risks associated with HRT, your family doctor or GP should make sure these are managed, i.e. if you are a smoker you need to stop smoking or at least go onto safer nicotine replacement therapies, you need to make sure your blood pressure and cholesterol levels are checked and if appropriate screened for diabetes. Your GP will also weigh you and ask about your activity levels and family history. Most UK GPs will plug all this information into one of the online cardiovascular risk calculators (e.g. QRISK-3) to see if you need treatment with a statin.
All of the above should happen anyway regardless of whether or not you have MS.
Is menopause different in women who have MS?
In my experience, menopause is likely to cause more problems in women with MS (wwMS) because of reduced brain reserve and the presence of many MS-related comorbidities. I suspect a lot of the problems the patient above describes are due to the menopause interacting with MS.
We now know from several studies that menopause affects the natural history of MS. The menopause seems to be a turning point; the relapse rate goes down after menopause and you are more likely to have worsening disability. One could argue that this could simply be due to ageing rather than menopause. However, there is compelling data that HRT is anti-ageing and many animal studies, including studies in MS animal models, show that oestrogens are neuroprotective.
HRT in menopausal women reverses many of the symptoms and signs of menopause, i.e. weight gain, hot flushes, depression, insomnia, dry vagina, hair and skin thinning, loss of breast tissue, urinary symptoms and reduced libido. HRT is anti-ageing when it comes to the skin, brain, reproductive system (vagina and breast) and bone health. The latter is very important for women with MS; pwMS tend to have more fragile bones (osteopaenia), particularly women and are more likely to fall and suffer fractures. Therefore anything that improves bone health should help wwMS overall.
So when it comes to advising my patients with MS about HRT it is a no-brainer. If you have MS and are menopausal the arguments for starting HRT are quite compelling. However, like everything else in medicine, it should be about choice and informed consent. What I am finding is that many GP's are reluctant to prescribe and monitor HRT in the NHS because of the ‘hassle factor'. It is easier for them not to prescribe HRT. I deplore this behaviour; in my opinion, every woman living in the UK who is menopausal should have the right to go onto HRT and at the same time they should have the right to say no thanks, I don’t want HRT because of associated cancer and vascular risks or I want to age naturally, but women with MS need to be given the choice. So don’t take NO for an answer and challenge your GP if they refuse to consider you for HRT.
In my practice, I also see a lot of women using natural HRT products independent of their GPs. Many of these products contain natural oestrogens and hence are working via the same mechanism as HRT. If you go this ‘natural’ HRT route you still need to make sure you are enrolled in your national screening programmes for both cardiovascular disease and breast cancer.
I suspect this post will generate a lot of questions and discussion. The three papers below are at least some food for thought.
If you are a woman with MS and perimenopausal or menopausal could you please share your experiences with us? I am hoping the MS-Selfie community will become a community of pwMS, in this case, wwMS, who can help each other. Thank you.
Subscriptions
I am encouraging readers to subscribe to the MS-Selfie Newsletter. The subscriptions will give you access to the case studies and the archive of these case studies. Please note all other newsletters, such as this one, are free. The money from subscriptions will be used to administer, transfer and curate the contents of the Newsletter onto a companion MS-Selfie microsite. The objective is to create an MS self-help guide.
The MS-Selfie case study from the 23rd of September is about a patient on ocrelizumab, who asked me whether or not she should delay her next dose of ocrelizumab to have the COVID-19 booster vaccine. She also wanted advice about which COVID-19 vaccine she should have for her booster.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.


Glad to hear that some readers of the Newsletter have been getting second opinions on the advice I have given. Fortunately, it has been congruent with my advice.
It is very important to check facts and get second and third opinions and check other sources. the only way you be confident about what is for real and what is fake is to do due diligence on the contents.
Huge thanks - this is a topic that I’ve brought up/questioned with various medical professionals for the last 10+ years!! Always to be told the same - ‘not enough research ....’ My ms has definitely deteriorated in the last 10 or so years (during menopause) and whether or not my menopause is to blame — ?? I have asked about HRT too and been told ‘no’ (without reason, investigation, etc)
So, I do think your research should be sent to Every professional connected to ms, so HRT can at least, be considered
Thanks again
Keep well /safe